Anxiety Reduction for Panic Disorder: Preventing and Managing Attacks
Specific methods for preventing and handling panic attacks.
Specific methods for preventing and handling panic attacks.
Imagine this: You're in a grocery store, reaching for a loaf of bread, when suddenly, the world tilts. Your heart hammers against your ribs, your breath catches in your throat, and a wave of pure, unadulterated terror washes over you. The fluorescent lights seem too bright, the chatter too loud. You're convinced you're having a heart attack, that you're dying, or worse—losing your mind. This is not just nervousness; this is a panic attack.
For the millions living with panic disorder, these episodes are not rare moments of stress but recurring storms that can strike without warning, upending daily life. The intense fear of the next attack can become its own prison, a condition known as anticipatory anxiety, which paradoxically fuels the very panic it seeks to avoid. Yet, here is the most crucial truth to hold onto from the very beginning: Panic attacks are treatable, and a life not dominated by fear is not only possible—it is within your reach.
Today, we stand at a remarkable intersection of ancient wisdom and cutting-edge technology in the fight against anxiety. We have at our disposal not only time-tested psychological techniques and natural remedies but also a new generation of intelligent tools that offer unprecedented insight into our own bodies and minds. This comprehensive guide is the first step on a journey toward sustainable calm. We will dismantle the panic cycle piece by piece, equipping you with a modern toolkit for prevention, management, and lasting resilience. From the immediate steps to halt an attack in its tracks to the long-term strategies that rewire your brain's response to stress, we will explore a holistic path forward, empowering you to reclaim your sense of safety and control.

To effectively conquer an enemy, you must first understand it. A panic attack is not simply feeling "very anxious." It is an abrupt, intense surge of overwhelming fear and discomfort that peaks within minutes. It's your body's ancient "fight-or-flight" system—designed to save you from immediate physical danger—firing at full force when no true threat exists.
During an attack, a cascade of physiological and cognitive symptoms takes over. Physically, you may experience a racing or pounding heart, sweating, trembling, shortness of breath or a feeling of being smothered, chest pain, nausea, dizziness, chills, or hot flashes. Cognitively, the experience is often marked by a profound sense of unreality (derealization) or detachment from oneself (depersonalization), a fear of losing control or "going crazy," and, most acutely, an overwhelming fear of dying.
When these attacks are recurrent and unexpected, and are followed by at least a month of persistent worry about having another attack or a significant maladaptive change in behavior related to the attacks (like avoiding places where they've occurred), a diagnosis of panic disorder may be made. It's a specific, diagnosable condition that affects a significant portion of the population.
The line between a single panic attack and panic disorder is crucial. Many people might experience an isolated panic attack in their lifetime, often during periods of extreme stress. Panic disorder, however, is characterized by the cycle of fear. The dread of the next attack becomes a constant background hum, which increases baseline anxiety and makes future attacks more likely. This cycle can lead to agoraphobia, where individuals avoid situations or places where they fear escape might be difficult or help unavailable if a panic attack occurs.
Understanding this is the foundation of recovery: recognizing that while the sensations are terrifying, they are a false alarm. Your body is misinterpreting signals. The chest pain is muscle tension, not a heart attack. The dizziness is from over-breathing, not an impending collapse. This cognitive shift—from "I am in mortal danger" to "My nervous system is having a disproportionate reaction"—is the first and most powerful step in breaking the cycle. It creates the mental space needed to apply the techniques that can calm the storm.
Panic disorder is the ultimate testament to the inseparable link between the mind and the body. It is a condition where psychological fear triggers a violent physiological revolt, and physiological sensations then feed back into catastrophic psychological thoughts. This feedback loop is the engine of a panic attack.
At the heart of this connection is the autonomic nervous system (ANS), your body's automatic control center. The ANS has two main branches:
In panic disorder, the SNS is hypersensitive and prone to slamming the gas pedal in response to minor stressors or even internal bodily sensations that would otherwise go unnoticed (like a slight heart palpitation). The PNS, responsible for applying the brakes and returning the body to calm, is often underactive or slow to respond.
This dysregulation manifests in key measurable physiological signs:
The groundbreaking insight from modern research is that these physiological markers are not just symptoms; they are accessible entry points for intervention. By using technology to become aware of our rising heart rate or declining HRV, we can intervene with a breathing exercise before a full-blown panic attack takes hold. By tracking our sleep, we can see the direct impact of a relaxing bedtime ritual. This turns the once-mysterious, terrifying bodily sensations into quantifiable data—and data is the foundation for understanding and change. For a deeper look at how cutting-edge devices translate this data into actionable insights, you can explore the science behind our approach at Oxyzen.ai.
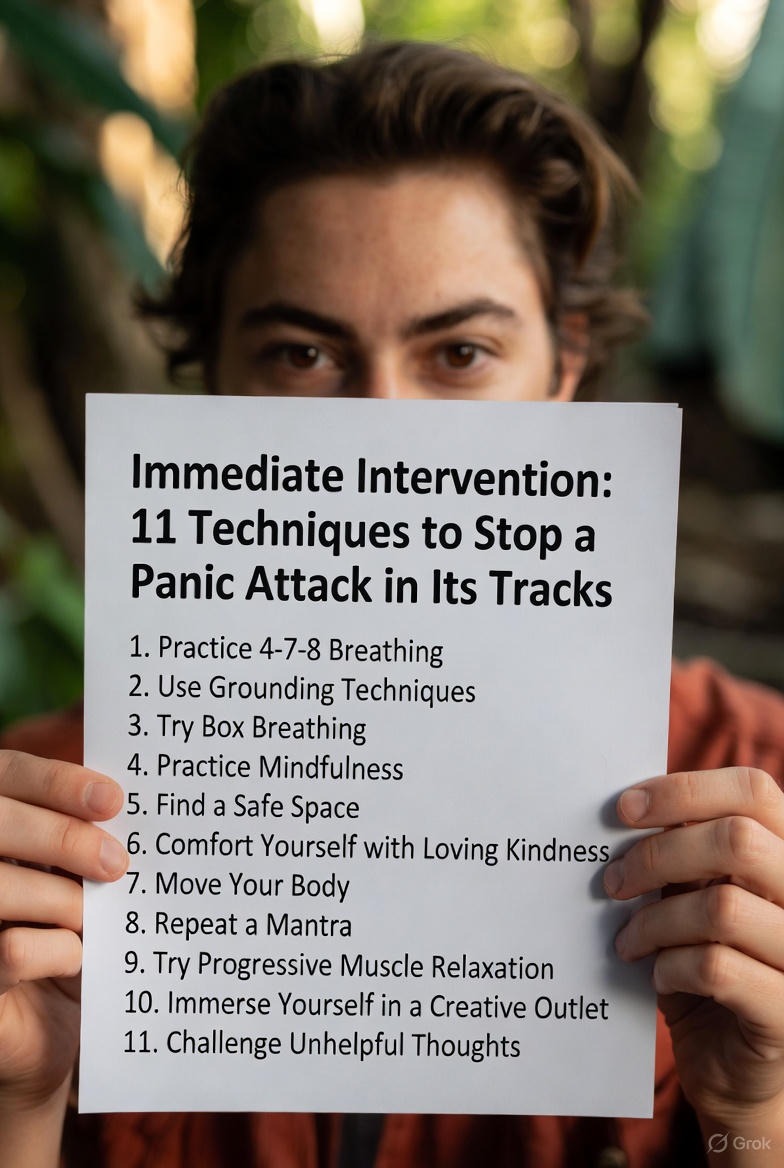
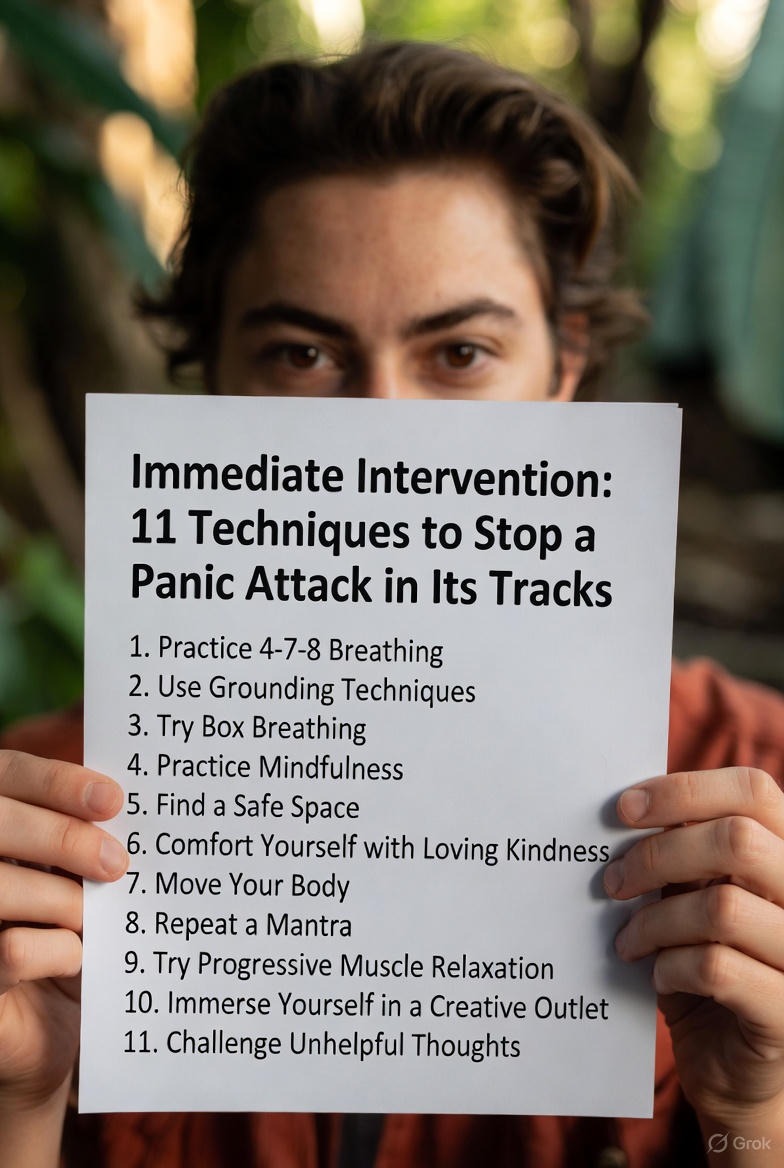
When a panic attack strikes, time distorts. Minutes feel like hours, and the urge to flee or fight is overwhelming. In these moments, having a pre-rehearsed plan of action is your lifeline. The goal is not to "fight" the panic, which often intensifies it, but to ground yourself, regulate your physiology, and ride out the wave until your nervous system recalibrates. Here are 11 evidence-based techniques to deploy when you feel the first signs of an attack.
Rapid breathing fuels panic. Deep, slow breathing activates the parasympathetic nervous system—your biological brake pedal. Don't just take a big gulp of air. Focus on diaphragmatic breathing: place a hand on your belly, inhale slowly through your nose for a count of 4, feel your belly rise, hold for a second, then exhale slowly through pursed lips for a count of 6 or 8. The extended exhale is key. Try the 4-7-8 method: inhale for 4, hold for 7, exhale for 8.
Panic pulls you into internal catastrophe. Grounding techniques force your brain to engage with the present, safe external world. Slowly and deliberately:
Fear creates widespread muscle tension, which signals "danger" back to the brain. PMR breaks this loop. Starting with your feet, tense a muscle group as hard as you can for 5 seconds, then completely release for 30 seconds, noting the feeling of relaxation. Work systematically up your body—calves, thighs, glutes, abdomen, hands, arms, shoulders, neck, and face.
Choose a single object in your immediate environment and study it with intense focus. If you have a "grounding object" you carry (a smooth stone, a ring, a keychain), hold it. Describe its details to yourself: "This pen is blue, metallic, with a clicker at the top. It has a small scratch here. The clip is slightly bent." This forces cognitive resources away from catastrophic thoughts.
Internally repeat a short, soothing phrase. It should be simple, present-tense, and believable. "This is a panic attack. It is not dangerous. It will pass." Or, "I am safe. My body is calming down. This is temporary." The repetition provides a cognitive anchor.
Paradoxically, resistance fuels panic. Try a mindset of curious acceptance. Say to yourself, "Okay, here it is. This is adrenaline. These are panic sensations. I don't like it, but I can let it be here until it passes." Imagine the anxiety as a wave you're floating on, not one you're drowning under.
A sudden temperature change can disrupt the panic loop. If possible, hold an ice cube in your hand or against your wrist. Splash cold water on your face. The "dive reflex" triggered by cold on the face can instantly slow heart rate. Alternatively, hold a warm cup of tea and focus on the heat spreading through your hands.
If you're not frozen, gentle movement can help burn off adrenaline and provide a rhythmic focus. Slowly pace in a small space, or simply shift your weight from foot to foot. Be cautious with vigorous exercise at the peak of an attack, as it may initially increase heart rate further.
Remind yourself of the facts: "I have had panic attacks before. They always end. No one has ever died from a panic attack. I am experiencing intense discomfort, not true danger." This counters the false narratives of doom your mind is creating.
If you're in a bright, loud, or crowded space, this sensory input can feel assaultive. If it's safe and possible, move to a quieter, more dimly lit place. Even leaning against a wall in a hallway can create a sense of stability and reduced sensory load.
Tell someone you're having a panic attack. Simply saying, "I'm having a wave of anxiety right now," can break the isolation and shame. A trusted person can help by speaking calmly, reminding you to breathe, or just being a grounded presence.
Remember: Not every technique will work every time. The crucial step is to have this toolkit ready and to practice these techniques when you are calm. This builds muscle memory, so when panic hits, your body and mind know what to do. It’s less about finding a magic "off switch" and more about skillfully navigating the storm until it naturally subsides, which it always does.

While immediate techniques are essential for crisis management, true freedom from panic disorder comes from long-term, daily practices that increase your resilience and lower your overall anxiety baseline. Think of it as building a levee so high and strong that even a large storm surge doesn't breach it. These strategies work slowly but fundamentally to re-regulate your nervous system and change your relationship with anxiety.
CBT is the most empirically supported psychotherapy for panic disorder. It operates on the core principle that our thoughts, feelings, and behaviors are interconnected. For panic, it involves two key components:
A seminal 1992 study published in the American Journal of Psychiatry found that a mindfulness-based stress reduction program significantly reduced anxiety and panic symptoms, with benefits maintained at follow-up. Mindfulness is not about emptying your mind or feeling blissful. It is the practice of paying attention to the present moment, on purpose, and without judgment.
For panic, this is revolutionary. Instead of reacting to a pang of anxiety with, "Oh no, here it comes! I can't handle this!" mindfulness teaches you to observe: "Hmm. There's tightness in my chest. There's a thought that says I'm in danger." This creates a critical space between you and your experience. You are not the panic; you are the awareness witnessing it. Regular meditation practice, even 10 minutes a day, strengthens the prefrontal cortex (the brain's rational center) and weakens the amygdala's (the fear center) reactive grip. It cultivates the "relaxation response," the physiological opposite of fight-or-flight.
"Exercise is medicine" is especially true for anxiety. Physical activity is a natural anxiety regulator for several reasons:
The key is consistency over intensity. A daily 30-minute brisk walk can be more beneficial for anxiety management than an exhausting, sporadic gym session. Exercise also functions as a natural form of interoceptive exposure, allowing you to experience an elevated heart rate and heavy breathing in a positive, controlled context.
Sleep and anxiety exist in a vicious cycle: anxiety causes poor sleep, and sleep deprivation dramatically lowers your threshold for anxiety and panic. Prioritizing sleep is non-negotiable. Good sleep hygiene includes:
By systematically investing in these long-term practices—CBT, mindfulness, exercise, and sleep—you are not just managing symptoms. You are actively constructing a more resilient, less reactive nervous system. You are changing the very soil in which panic seeds try to grow, making it far less fertile for them to take root. To see how these principles are integrated with daily technology for support, you can read about our philosophy and user experiences on the Oxyzen.ai blog.
For many seeking to manage anxiety, the world of herbal and natural remedies offers a compelling, complementary path alongside conventional treatment. It's a realm of ancient wisdom now being scrutinized by modern science. The appeal is clear: a desire for more "natural" interventions and a sense of personal agency over one's wellness. However, navigating this landscape requires both curiosity and caution—the term "natural" does not automatically mean "safe" or "effective for everyone".
Several herbs have shown promise in clinical studies for reducing symptoms of anxiety, though the body of evidence varies in strength, and more research is often needed.
Crucial Considerations Before Use:
Nature's pharmacy holds valuable tools, but they should be used with respect, knowledge, and professional guidance as part of a comprehensive, modern approach to mental wellness.
We are witnessing a paradigm shift in mental healthcare, moving from reactive, episodic care to proactive, continuous monitoring—and wearable technology is at the forefront of this revolution. For those managing panic disorder, these devices offer something previously unimaginable: an objective, real-time window into the hidden physiological landscape of their anxiety. This is more than just tracking steps; it's about decoding the body's subtle distress signals long before they erupt into a full-blown panic attack.
Smart rings, like the Oura Ring, and advanced smartwatches have evolved into sophisticated health monitors. They continuously track a suite of biometrics directly relevant to anxiety:
The true power, however, lies in the convergence of this data with Artificial Intelligence (AI). Researchers are now developing algorithms that can analyze the streams of data from wearables to actually predict and detect anxious states. A 2023 systematic review and meta-analysis in the Journal of Medical Internet Research found that wearable AI could detect anxiety with a pooled mean accuracy of 82%. Imagine your device sensing a rise in resting heart rate and a drop in HRV—patterns that have preceded past panic attacks for you—and sending you a gentle alert: "Your body is showing signs of stress. Consider a 5-minute breathing exercise?"
This is the promise of personalized, just-in-time intervention. Instead of trying to remember coping skills in the maelstrom of panic, your device can prompt you to use them during the early, manageable build-up phase. It transforms anxiety management from a purely cognitive effort into a data-informed practice. You can run experiments: "Does my HRV improve on days I meditate?" "How does a stressful work meeting affect my physiological metrics?" This feedback loop fosters self-efficacy and provides concrete evidence of what works for your unique biology.
Of course, this field is still emerging. The same review notes that while promising, wearable AI is "not yet advanced enough for clinical use" alone and should complement, not replace, professional assessment. Privacy and data security are also paramount considerations. Yet, the direction is clear: technology is becoming an empathetic partner in mental wellness, offering insights that empower individuals to understand and care for their minds through the lens of their bodies. For those interested in how this technology translates into a wearable product designed for holistic wellness, you can learn more about the Oxyzen smart ring and its mission.
Knowledge is power, but consistent action creates change. With an understanding of the techniques and tools available, the final, most critical step is to synthesize them into a Personalized Panic Prevention Plan (PPP). This is not a rigid set of rules, but a flexible, living strategy that you design, own, and refine. It moves you from a passive victim of panic to an active architect of your own calm.
Your PPP should have three core pillars: Daily Foundation, Early Intervention, and Crisis Management.
These are the non-negotiable habits you practice every day, regardless of how you feel, to build resilience and lower your baseline anxiety.
This is for when you notice the first subtle signs of increased anxiety—irritability, muscle tension, repetitive worrying, or a slight rise in resting heart rate on your wearable.
This is your drilled response for the onset of acute panic symptoms. It should be simple, memorized, and physical.
Creating Your Plan:
This Personalized Panic Prevention Plan is your declaration of agency. It acknowledges that while you may not control the first spark of anxiety, you have a well-rehearsed, multi-layered system to prevent it from becoming a devastating fire. It combines the wisdom of therapy, the calm of mindfulness, the strength of your body, and the insight of technology into a unified front against panic. The journey toward lasting calm is built one intentional, data-informed, compassionate choice at a time.
In the first part of our guide, we laid the essential groundwork: understanding the panic cycle, mastering immediate interventions, and building a personalized prevention plan with modern tools. This knowledge empowers you to manage the storms. Now, we move deeper. True, lasting mastery over panic disorder involves more than crisis management; it requires transforming your relationship with fear itself, healing the underlying systems that contribute to dysregulation, and building a life so rich and connected that anxiety no longer holds the central narrative.
This section explores the advanced psychological frameworks, the often-overlooked physical contributors, and the profound power of community that together forge unshakable resilience. We will look at how to not just survive panic attacks, but to fundamentally thrive beyond them.
To advance in your recovery, it helps to understand the biological machinery of fear. At the heart of every panic attack is the amygdala, two small, almond-shaped clusters in the brain's temporal lobes. Think of it as your brain's ancient, hypersensitive smoke alarm. Its job is to scan for threat and, when detected, instantly activate the fight-or-flight response—bypassing the slower, rational prefrontal cortex.
In panic disorder, this smoke alarm is calibrated incorrectly. It's as if it mistakes the scent of burnt toast for a five-alarm fire. This amygdalar hypersensitivity means it reacts to benign internal cues (a skipped heartbeat, a slight dizziness) or minor stressors with a full-throttle emergency response. Furthermore, the prefrontal cortex (PFC), which should rationally assess the threat and help calm the amygdala, often has weakened communication with it. This is the neural basis of feeling "hijacked" by panic.
The brilliant news of modern neuroscience is neuroplasticity—the brain's ability to reorganize itself by forming new neural connections throughout life. You are not stuck with a hypersensitive amygdala. Every time you successfully apply a coping technique, you are engaging in "top-down" regulation, strengthening the pathways from your rational PFC to your emotional amygdala. More specifically, you are bolstering the ventromedial prefrontal cortex (vmPFC), a region critical for inhibiting the amygdala and extinguishing fear responses.
How to Actively Encourage Neuroplastic Change:
Understanding this science transforms your practice. When you do a breathing exercise, you're not just "calming down"—you are performing targeted neurosurgery, consciously reshaping your brain's architecture toward greater peace and resilience.
While Cognitive Behavioral Therapy (CBT) excels at changing the content of anxious thoughts ("This sensation is dangerous" → "This sensation is uncomfortable but safe"), Acceptance and Commitment Therapy (ACT) offers a paradigm-shifting alternative. Instead of challenging thoughts, ACT teaches you to change your relationship with them. Its core philosophy is that psychological suffering is often caused by experiential avoidance—the exhausting struggle to control or eliminate unwanted thoughts and feelings.
For panic, this struggle is the essence of anticipatory anxiety: "I must avoid panic at all costs." ACT posits that this very struggle gives panic its power. The goal of ACT is not to reduce symptoms, but to build psychological flexibility—the ability to be present, open up, and do what matters, even when anxiety is in the passenger seat.
ACT is built on six core processes, often visualized as the points of a hexagon:
An ACT Exercise for Panic: "Leaves on a Stream"
When you feel panic rising, close your eyes. Imagine a gentle stream. Now, imagine placing each anxious thought, each catastrophic prediction, and each physical sensation onto a leaf. One by one, place them on the stream and watch them float by. Don't analyze the leaves. Don't stop them. Just let them come and go. Your task is not to empty the stream, but to watch the leaves with detachment. This practice embodies defusion and acceptance.
ACT is profoundly liberating because it decouples your life's direction from your internal weather. It teaches you that you can have a panic attack and still be living a meaningful life. The anxiety doesn't have to disappear for you to move forward.
One of the most significant advancements in understanding anxiety is the recognition of the gut-brain axis—the intimate, bidirectional communication network linking your central nervous system with your enteric nervous system (the "second brain" in your gut). This connection is why you feel "butterflies" when nervous and why chronic stress can upset your stomach. For panic disorder, this axis may be a critical piece of the puzzle.
The path forward is not about the eradication of anxiety—a normal human emotion—but about the demotion of panic from a tyrannical ruler to a sometimes-annoying background signal. It is about building a self that is so much larger, stronger, and more interesting than any single symptom could ever be.
Your gut is home to trillions of microbes (the gut microbiome) that produce a vast array of neurochemicals. In fact, about 90% of your body's serotonin, a key neurotransmitter for mood regulation and a common target of SSRI medications, is produced in the gut. An imbalance in gut bacteria (dysbiosis) can disrupt this production and contribute to systemic inflammation.
Chronic, low-grade inflammation is now a major focus of anxiety research. Inflammatory markers like C-reactive protein (CRP) and cytokines can cross the blood-brain barrier and interact with neural circuits. This "sickness behavior"—fatigue, social withdrawal, anxiety—is an evolutionary response to infection, but when inflammation becomes chronic due to diet, stress, or illness, it can create a persistent state of neural alarm and hypervigilance, lowering the threshold for panic.
Dietary and Lifestyle Strategies to Support the Gut-Brain Axis:
Addressing gut health is not a standalone cure for panic disorder, but it is a powerful adjunctive strategy. By creating a healthier internal environment, you remove a potential physiological driver of anxiety and give your nervous system a more stable foundation from which to operate. It’s a powerful example of treating the whole person, not just the mind.
Panic disorder is an intensely isolating experience. The shame and fear of having an attack in public can drive people into social withdrawal, creating a lonely feedback loop where isolation fuels depression, which in turn exacerbates anxiety. Breaking this cycle by intentionally cultivating social connection is not just helpful; it is therapeutic.
Social support acts as a powerful buffer against stress. Positive social interactions:
How to Build Your Anxiety Support System:
Remember, seeking connection is a sign of strength, not weakness. As you build your community, you dismantle the fortress of isolation that panic disorder tries to build around you. For stories of how others have navigated this journey and found support, you can find shared experiences and community insights on the Oxyzen.ai testimonials page.
Effective management of panic disorder often requires a team approach. Knowing how to navigate the healthcare system and assemble the right professionals is a crucial skill for your long-term well-being.
Your Core Treatment Team May Include:
How to Be an Empowered Patient:
Assembling the right team is an investment in your health. These professionals are your guides and allies, providing the expert support as you do the brave work of recovery.
Medication can be a highly effective component of a comprehensive treatment plan for panic disorder. It's important to view it realistically: as a tool to reduce symptom severity and create the neurological stability needed to fully engage in therapy and lifestyle changes.
Common Medication Classes for Panic Disorder:
Crucial Considerations:
The decision to use medication is a personal one, to be made in close consultation with a psychiatrist. It is not a sign of failure, but a potential step toward creating the biological calm necessary for deep psychological work.
As we look ahead, the frontier of anxiety treatment is being reshaped by remarkable technological innovations that promise more immersive, precise, and personalized interventions.
These technologies are not meant to replace human therapists but to augment and extend care into daily life. They offer the promise of making effective treatment more scalable, engaging, and precisely tailored to the individual's unique physiological and psychological signature.
The journey with panic disorder is undeniably challenging, but the landscape of hope and help has never been richer. From the ancient practices of mindfulness to the futuristic tools of biometric AI, you have an unprecedented arsenal at your disposal. Recovery is not the absence of anxiety, but the expansion of your life around it. It is the courageous process of building a self that is more resilient, more flexible, and more committed to valued living than any single symptom could ever destroy.
In the final part of this comprehensive guide, we confront the realities of long-term management. True mastery of panic disorder is not a linear journey to a permanent "cure," but the cultivation of a resilient, adaptive system for life. It involves learning to navigate inevitable setbacks without self-judgment, solidifying your gains into an unshakeable foundation, and perhaps most powerfully, discovering how the struggle itself can forge a deeper, more meaningful existence.
This section provides the roadmap for the long haul—transforming recovery from a fight against symptoms into a lifelong practice of compassionate strength.
A surge of panic after a period of calm can feel like a devastating failure. This moment is critical. The narrative you attach to this experience—"I've lost all my progress" versus "This is a temporary challenge"—will determine its long-term impact.
First, let's abolish the word "relapse" with its connotations of total collapse. Instead, adopt the framework of a setback or an exacerbation. In chronic condition management, from diabetes to anxiety, flare-ups are a normal part of the process, not an erasure of learned skills. They are often triggered by predictable factors: periods of intense stress, illness, sleep deprivation, hormonal shifts, or even the gradual neglect of daily maintenance practices during good times.
How to Navigate a Setback with Wisdom:
A setback is not a reset button. It is a bend in the road, offering a chance to check your map, tighten your laces, and reaffirm your direction with even greater clarity.
When the acute storms of panic become less frequent, the work subtly shifts from "crisis management" to "fortress building." The goal is to integrate your hard-won skills so deeply into your life that they become part of your identity—not as a "person with panic disorder," but as a person who values and practices mindfulness, self-awareness, and holistic health.
Key Elements of a Resilient Lifestyle:
This maintenance phase is where life truly begins to open up. The energy once consumed by fighting panic is gradually freed and redirected toward creativity, connection, and contribution.
The most profound potential outcome of grappling with panic disorder is not merely a reduction in symptoms, but Post-Traumatic Growth (PTG). Psychologists Richard Tedeschi and Lawrence Calhoun coined this term to describe the positive psychological change that can emerge from the struggle with highly challenging life crises.
PTG does not imply the trauma was good, but that the individual, through their effort to rebuild, can develop in ways that might not have occurred otherwise. For those who have faced the terror of panic, growth often manifests in five key areas:
Cultivating Post-Traumatic Growth:
This growth is the ultimate destination of the journey. It represents not a return to a pre-panic "normal," but an evolution into a wiser, more integrated, and more compassionate human being.
Panic disorder does not exist in a vacuum; it intersects with other life stages and conditions, requiring nuanced understanding.
In all cases, a collaborative, holistic healthcare team is essential to navigate these complex intersections safely and effectively.
Your journey is supported by a community of resources. Here is a curated list to empower your ongoing path:
Professional Organizations & Helplines:
Recommended Reading & Programs:
Finding the Right Professional:
Remember, the mission and vision behind the tools you use matter. Understanding the why behind a product can deepen your trust and engagement with it. To learn about the core philosophy driving the integration of this kind of technology into daily wellness, you can explore the story behind Oxyzen.
As we conclude this definitive guide, return to the core truth stated at the very beginning: a life not dominated by fear is within your reach. You now possess a map that spans from the neurobiology of fear to the philosophy of meaningful living, from immediate physiological hacks to the long-term architecture of a resilient life.
The path forward is not about the eradication of anxiety—a normal human emotion—but about the demotion of panic from a tyrannical ruler to a sometimes-annoying background signal. It is about building a self that is so much larger, stronger, and more interesting than any single symptom could ever be.
Your journey will have its rhythms—periods of smooth sailing and challenging swells. When the swells come, you will no longer be a ship at their mercy. You will be the skilled captain, with a detailed map (your PPP), a trusted crew (your support system), advanced navigational instruments (your knowledge and technology), and the hard-earned wisdom to know that storms always, always pass.
You have the tools. You have the understanding. You have the capacity for profound growth. The work now is to live it—one mindful breath, one valued action, one compassionate moment at a time. Your life of greater freedom, connection, and purpose awaits.
Your Trusted Sleep Advocate (Sleep Foundation — https://www.sleepfoundation.org/)
Discover a digital archive of scholarly articles (NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature (PubMed — https://pubmed.ncbi.nlm.nih.gov/)
experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/)
Every life deserves world class care (Cleveland Clinic -
https://my.clevelandclinic.org/health)
Wearable technology and the future of predictive health monitoring. (MIT Technology Review — https://www.technologyreview.com/)
Dedicated to the well-being of all people and guided by science (World Health Organization — https://www.who.int/news-room/)
Psychological science and knowledge to benefit society and improve lives. (APA — https://www.apa.org/monitor/)
Cutting-edge insights on human longevity and peak performance
(Lifespan Research — https://www.lifespan.io/)
Global authority on exercise physiology, sports performance, and human recovery
(American College of Sports Medicine — https://www.acsm.org/)
Neuroscience-driven guidance for better focus, sleep, and mental clarity
(Stanford Human Performance Lab — https://humanperformance.stanford.edu/)
Evidence-based psychology and mind–body wellness resources
(Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/)
Data-backed research on emotional wellbeing, stress biology, and resilience
(American Institute of Stress — https://www.stress.org/)