The Relationship Between Daily Stress and Chronic Disease (Prevention Guide)
Chronic daily stress is a major contributor to inflammation, heart disease, metabolic disorders, and mental health conditions.
Chronic daily stress is a major contributor to inflammation, heart disease, metabolic disorders, and mental health conditions.
You wake up to a blaring alarm, your mind already racing with the day’s deadlines before your feet hit the floor. Your commute is a tense navigation of traffic and notifications. At work, your inbox is a relentless source of demands, and at home, the responsibilities of life continue to pile up. This isn’t just a “busy day”—it’s a chronic state of low-grade emergency, a simmering pot of stress that never truly turns off.
What if this relentless pressure is doing more than just ruining your mood? Emerging science reveals a startling truth: the daily stress we’ve learned to accept as normal is not a harmless side effect of modern life. It is a potent, biologically disruptive force that systematically dysregulates your body, laying the precise physiological groundwork for the chronic diseases that define 21st-century health crises: heart disease, type 2 diabetes, autoimmune disorders, depression, and neurodegenerative decline.
This article is not about telling you to “stress less”—an impossible platitude. It is a deep, evidence-based exploration into the hidden mechanisms connecting your daily anxieties to long-term illness. More importantly, it is a proactive prevention guide. We will demystify the complex cascade from a stressful thought to cellular dysfunction, and equip you with a modern, actionable framework for building resilience. By understanding the link and leveraging today’s technology, like the nuanced biometric insights provided by devices such as the Oxyzen smart ring, you can move from being a passive victim of stress to an active architect of your long-term health.
The journey to prevention starts with knowledge. Let’s begin by unraveling the most fundamental question: what is stress, truly, from your body’s perspective?
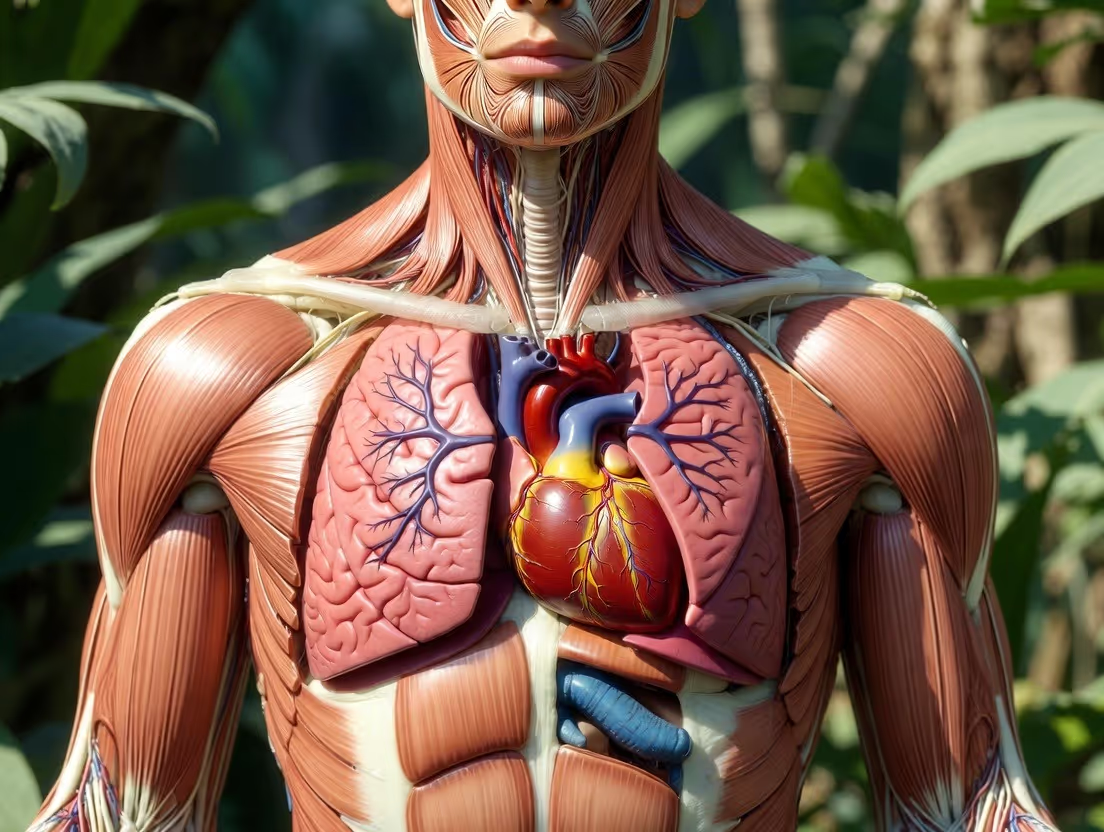
To understand why daily stress is so damaging, we must first appreciate its original, life-saving purpose. The stress response, often termed “fight-or-flight,” is not a flaw in our design. It is our evolutionary masterpiece—a brilliantly fast, whole-body communication system designed for acute, physical survival.
The process begins in your brain’s hypothalamus, the command center for homeostasis. Upon perceiving a threat (be it a saber-toothed tiger or an angry email), it sends a chemical signal (corticotropin-releasing hormone, or CRH) to the pituitary gland. This gland then releases adrenocorticotropic hormone (ACTH) into the bloodstream, which travels to your adrenal glands, perched atop your kidneys. The adrenals are the executioners of the response, secreting the primary stress hormones: cortisol and adrenaline (epinephrine).
This HPA axis activation triggers a breathtaking symphony of changes:
This system is meant to be a sprint. You confront the threat, escape it, and then your body returns to a state of calm “rest-and-digest,” governed by the parasympathetic nervous system. The problem in modern life is that our threats are rarely physical, but psychological and chronic—a looming project, financial worry, social conflict. These triggers don’t have a clear endpoint. The “tiger” is now a perpetual presence in your mind, and the HPA axis is forced to run a marathon it was never designed for.
In an acute crisis, cortisol is a hero. It mobilizes energy, modulates inflammation, and helps regulate fluid balance. However, when secreted persistently due to chronic stress, cortisol’s effects become pathological. It begins to:
The transition from this acute, life-saving biology to a state of chronic dysregulation is the critical pivot point where stress transitions from a temporary state to a disease catalyst. To see how, we must look deeper at the concept of allostatic load—the wear and tear on the body that accumulates when this emergency system is never fully switched off.
If homeostasis is the body’s ideal balance point, allostasis is the process of achieving stability through change. It’s the active, dynamic process of adjusting your heart rate, hormones, and immune activity to meet life’s demands. The allostatic load is the cumulative cost of this constant adjustment. Think of it not as a single moment of stress, but as the physiological “debt” accrued from repeated cycles of stress response, especially when there is inadequate recovery.
Renowned neuroendocrinologist Bruce McEwen, who pioneered this concept, described it as the price the body pays for being forced to adapt to adverse psychosocial or physical situations. When the allostatic load exceeds your body’s capacity to compensate, systems begin to break down. This is not a theoretical concept; it is quantifiable through biomarkers.
Research has identified key markers that, when elevated over time, signify a high allostatic load and a significantly increased risk for disease. These often include:
This last point, HRV, is particularly telling. It measures the subtle variation in time between each heartbeat. A higher, more variable HRV indicates a resilient, adaptable nervous system that can smoothly transition between stress and relaxation. A low, rigid HRV is a powerful predictor of high allostatic load and future cardiac events. Monitoring HRV is now a cornerstone of modern wellness technology, providing a real-time window into your autonomic nervous system balance. Devices like the Oxyzen smart ring track HRV continuously during sleep, offering an unparalleled, objective measure of your recovery status and allostatic load, far beyond how you simply "feel."
The danger of a high allostatic load is that it doesn’t just make you tired; it directly corrodes the body’s most fundamental systems. It’s the common soil in which the seeds of diverse chronic diseases take root. To understand this, we must follow the path of inflammation—the body’s double-edged sword turned against itself.

If allostatic load is the accumulating debt, then systemic inflammation is the high-interest rate that accelerates the damage. Acute inflammation is, like the stress response itself, a vital protective mechanism—the redness, heat, and swelling that surrounds a wound, marshaling immune cells to heal and defend. Chronic, low-grade inflammation is a silent, smoldering fire that burns throughout the body, damaging healthy tissues over decades.
The link between stress and inflammation is direct and biochemical. When the HPA axis is activated, cortisol should, in theory, act as a potent anti-inflammatory. But under chronic stress, cells can become "glucocorticoid resistant"—they stop "listening" to cortisol’s anti-inflammatory signals. This is akin to the insulin resistance seen in type 2 diabetes.
Simultaneously, stress activates the sympathetic nervous system, which sends signals via nerve fibers to immune cell-producing organs like the spleen and bone marrow, prompting the release of pro-inflammatory cytokines—immune system messenger molecules like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α).
Furthermore, the constant energy mobilization and metabolic havoc of chronic stress can lead to the release of damage-associated molecular patterns (DAMPs) from distressed cells. These DAMPs are interpreted by the immune system as signals of injury or infection, further stoking the inflammatory flames.
This pervasive inflammatory state is the keystone pathological process in almost every major chronic illness:
By keeping the inflammatory response perpetually engaged, chronic stress erodes the body's functional integrity at the most basic level. It’s a universal solvent for health. And one of the first and most critical systems it dissolves is our sleep.
Sleep is the cornerstone of restoration. It is when the brain clears metabolic waste via the glymphatic system, memories are consolidated, hormones are balanced, and tissues are repaired. Chronic stress is the arch-nemesis of restorative sleep, creating a self-perpetuating vortex that dramatically accelerates disease risk.

Stress doesn’t just make it hard to fall asleep; it fundamentally corrupts the quality of sleep. Elevated evening cortisol and adrenaline keep the nervous system in a state of hyper-arousal. This leads to:
The damage is not one-way. Poor sleep then amplifies the stress response the next day. Studies show that even one night of partial sleep deprivation leads to:
Thus, you wake up more emotionally volatile, less cognitively sharp, more hungry for junk food, and physiologically primed for a stronger stress response to the day’s challenges. The cycle intensifies. Breaking this cycle is paramount, and it starts with objective measurement. You cannot manage what you do not measure. This is where modern technology becomes indispensable. By using a device that tracks your sleep stages, resting heart rate, and HRV—like you can with detailed analytics from Oxyzen.ai—you move from guessing about your sleep quality to having concrete, actionable data. You can see the direct impact of a stressful day on your deep sleep score or correlate an evening of poor sleep with a plummeting next-day HRV.
Understanding this destructive vortex naturally leads us to ask: where in our bodies does this stress-sleep-inflammation axis strike first and most measurably? Often, it’s our metabolic engine.
Your metabolism is a finely tuned system for converting food into energy. Chronic stress throws a wrench into every gear of this system, directly promoting weight gain, insulin resistance, and the cluster of conditions known as metabolic syndrome—a primary gateway to heart disease and diabetes.
Under stress, cortisol’s primary job is to ensure the brain has enough glucose (its preferred fuel) to handle the perceived emergency. It does this by:
In the short term, this is brilliant. In the long term, it’s disastrous. Chronically high blood glucose forces the pancreas to pump out more and more insulin. Eventually, muscle and fat cells become numb to insulin’s signal—this is insulin resistance. The pancreas becomes exhausted, leading to type 2 diabetes.
Cortisol doesn’t just affect blood sugar; it specifically instructs the body to store fat, and not just any fat. It promotes the storage of visceral adipose tissue (VAT)—the deep, toxic fat that wraps around your abdominal organs. Unlike subcutaneous fat (the kind under your skin), visceral fat is metabolically active, acting like an endocrine organ that secretes its own pro-inflammatory cytokines and free fatty acids directly into the portal circulation to the liver, further driving inflammation and insulin resistance.
This creates a perfect storm: Stress → High Cortisol → Insulin Resistance & Visceral Fat Gain → Inflammation → More Insulin Resistance. It’s a closed, self-accelerating loop. Recognizing the early signs of this metabolic shift is critical for prevention. Beyond standard blood tests, tracking trends in your resting metabolic rate and observing how your body responds to different foods and stressors can provide early warnings. While not a diagnostic tool, comprehensive wellness tracking from a device like the Oxyzen ring can help you connect lifestyle dots—showing, for instance, how a week of high stress correlates with a rising resting heart rate and subjective feelings of bloating or energy crashes.
With our metabolism under siege, it’s no surprise that the system responsible for literally moving this metabolic fuel—our cardiovascular system—takes a direct and devastating hit.
The cardiovascular system is on the front lines of every stress response. The constant "revving" of this system under chronic stress leads to structural and functional changes that are a direct prelude to heart attack, stroke, and heart failure.
Repeated episodes of stress-induced hypertension (high blood pressure) cause wear and tear on the delicate endothelial lining of arteries. This damage initiates the process of atherosclerosis. Inflammatory cells (LDL cholesterol) infiltrate the damaged area, forming plaque. Stress hormones also make platelets stickier, increasing the risk of a clot that can block a narrowed artery.
Furthermore, chronic sympathetic nervous system activation can lead to left ventricular hypertrophy—a thickening of the heart’s main pumping chamber. This is the heart muscle adapting to constantly pumping against high pressure, much like any muscle grows when worked. But a thickened heart wall becomes stiff and inefficient, a major risk factor for heart failure.
We return to the critical metric of HRV. A stressed, sympathetic-dominant nervous system produces a steady, metronomic heart rate—low HRV. This lack of flexibility is a powerful independent predictor of sudden cardiac death and arrhythmias. It signifies a heart and nervous system that have lost their adaptive resilience, operating in a rigid, high-alert state. Conversely, high HRV reflects a strong, adaptable system with robust parasympathetic (rest-and-digest) tone.
Monitoring HRV is thus one of the most powerful actions you can take for cardiovascular prevention. It gives you daily, non-invasive feedback on your autonomic nervous system balance. By reviewing trends on a platform like Oxyzen.ai, you can see how lifestyle choices—a hard workout, a meditation session, a late night, or a difficult conversation—directly impact this fundamental biomarker of cardiac and systemic health. It transforms an abstract concept like "stress" into a tangible, manageable data point.
As we trace the path of destruction from the heart upward, we arrive at the command center itself—the brain. The impact of stress here is not merely "feeling worried"; it is a process of literal remodeling with profound consequences for mental and cognitive health.

Your brain is the ultimate target and originator of the stress response. Chronic stress doesn't just create anxious thoughts; it physically alters brain structure and function, increasing vulnerability to mood disorders and accelerating cognitive decline.
Two brain regions are disproportionately affected:
Stress depletes key neurotransmitters. It can exhaust supplies of serotonin (regulating mood, sleep, appetite) and dopamine (motivation, pleasure), contributing directly to symptoms of depression and anhedonia (inability to feel pleasure).
As discussed, pro-inflammatory cytokines can cross the blood-brain barrier. In the brain, they can alter the metabolism of neurotransmitters and activate microglia (the brain’s immune cells). This neuroinflammation is now recognized as a key driver in the pathogenesis of major depressive disorder and is a significant contributor to the neurodegenerative processes in Alzheimer’s disease.
The brain, however, is also the source of our greatest hope: neuroplasticity. The brain's ability to change means that interventions can reverse some of this damage. Meditation, cognitive-behavioral therapy, and regular exercise have all been shown to increase hippocampal volume and modulate amygdala activity. The first step is awareness of your own patterns, which is why many users find that pairing mindfulness practice with biometric feedback from a device that tracks physiological calm creates a powerful loop of self-regulation. Reading about others' journeys with this integration, such as those shared on the Oxyzen testimonials page, can provide both inspiration and practical social proof.
If the brain is the command center, then the gut is often the canary in the coal mine—a sensitive, early warning system where stress manifests in painfully tangible ways.
Your gastrointestinal system is so densely innervated and connected to the brain that it’s often called the "second brain." This gut-brain axis is a bidirectional superhighway of communication, and stress is a major disruptor of its traffic.
The "fight-or-flight" response diverts energy and blood flow away from digestion. Chronic stress leads to:
Approximately 70-80% of your immune tissue resides in and around the gut. Therefore, stress-induced gut dysfunction has direct and massive implications for systemic immunity. The resulting inflammation and immune dysregulation are, as we've seen, foundational to autoimmune disease and general susceptibility to illness. This gut-immune-stress connection explains why periods of high stress so often coincide with gut flare-ups, colds, or worsened allergy and autoimmune symptoms.
Managing stress, therefore, is not just about mental calm; it’s a direct intervention for gut health and immune resilience. Strategies that support the gut-brain axis—like probiotics, prebiotic fiber, and stress-reduction techniques—are a core part of a modern prevention protocol. For a deeper dive into these supporting lifestyle strategies, resources like the Oxyzen blog often explore the intersection of technology, nutrition, and nervous system regulation.
After examining these eight distinct yet interconnected systems under siege, a critical question emerges: why do some people crumble under pressure while others seem to thrive? The answer lies in the hidden, internal variable of resilience.
Resilience is not the absence of stress; it is the capacity to withstand, adapt to, and recover from adversity. It is what determines whether a given allostatic load leads to disease or is successfully managed. This capacity is not merely psychological; it is deeply biological, encoded in the very responsiveness of your HPA axis and the flexibility of your nervous system.
A resilient stress response is characterized by three key features:
In non-resilient individuals, the response is either exaggerated (too much hormone release) or prolonged (slow to return to baseline). This pattern is often established early in life. The seminal Adverse Childhood Experiences (ACE) Study demonstrated a powerful, dose-dependent relationship between childhood trauma (abuse, neglect, household dysfunction) and the risk of chronic disease in adulthood. Early life stress can "calibrate" the HPA axis to be hyper-reactive for life, setting a higher baseline allostatic load.
The hopeful news is that resilience is malleable. It can be built through specific, evidence-based practices:
Building resilience is the ultimate prevention. It’s about upgrading your body’s operating system to handle life’s inevitable stressors without crashing. To do this effectively, you need objective feedback. This is the cornerstone of the modern approach: quantified self-awareness.
For generations, our understanding of personal stress was purely subjective—a feeling of being "wound up" or "burned out." This is insufficient for prevention. Feelings can be misleading; data reveals truth. The rise of personal biometric tracking represents a paradigm shift in proactive health management, moving us from reactive symptom-chasing to proactive system optimization.
We are notoriously bad at judging our own physiological state. You might feel "fine" while your HRV has been trending downward for weeks, indicating creeping allostatic load. You might think you slept "okay," but your sleep tracker reveals you got only 12 minutes of deep sleep. This disconnect is why so many people are caught off guard by a diagnosis—the internal warning signals were either muted or ignored.
Key, trackable biomarkers for stress and resilience include:
Wearing a device that continuously and accurately captures this data—particularly during sleep, when your body is in its most honest state of repair—provides an unparalleled personal dashboard. You are no longer guessing. You can see, in clear graphs, that the late-night work session crashed your deep sleep, or that the morning meditation practice boosted your afternoon HRV.
This is the promise of modern wellness technology. By partnering a sophisticated sensor like the Oxyzen smart ring with an intuitive analytics platform, you gain a personal biolab. You can run experiments: *Does cutting off caffeine after 2 PM improve my deep sleep? Does a 20-minute evening walk lower my nighttime heart rate? How does my body truly respond to that new workout routine?* For those curious about the technology that makes this possible, you can learn more about smart ring technology and its applications in daily health management. This data-driven empowerment is the first, critical step in a larger, personalized system of prevention, which we will now begin to construct.
Understanding the “why” is only half the battle. The true power lies in the “how.” With the science of the stress-disease link laid bare, we now pivot from knowledge to action. This section is your blueprint—a practical, personalized, and proactive framework for dismantling the mechanisms we’ve just explored and building formidable, lifelong resilience. Prevention is not a single action; it is a system. And every effective system begins with a clear, honest assessment of the starting point.
You cannot change what you do not measure. Before you can effectively intervene, you must map your personal stress landscape. This audit combines subjective reflection with objective data to create a full-spectrum view of your vulnerabilities and strengths.
Begin by journaling your answers to these questions for one week:
This is where technology transforms guesswork into strategy. For a minimum of two weeks, use a reliable biometric tracker to establish your baseline. Key metrics to observe:
Crucially, correlate the subjective and objective. Did a day filled with your noted triggers lead to a poor sleep score that night? Did a spontaneous dinner with friends (a recovery practice) correlate with a higher next-morning HRV? This connection is your most powerful insight. For those beginning this journey, the Oxyzen FAQ is an excellent resource for understanding how to interpret these specific metrics and get the most from your data.
This audit is not about judging yourself; it’s about diagnosing your personal stress signature. With this map in hand, you can now deploy targeted, high-efficacy interventions. We start with the most immediate lever you have: your nervous system.
Your autonomic nervous system isn’t meant to be a passive spectator; you can actively steer it. These techniques provide direct "manual override" to shift from stressed (sympathetic) to calm (parasympathetic) dominance, lowering cortisol and inflammation in real-time.
Breathing is the only autonomic function you can easily control, and it directly influences your heart and brain. Two potent techniques:
Chronic stress thrives on autopilot. Strategic pauses break the cycle.
Deliberate, acute cold exposure (e.g., 30-90 seconds in a cold shower at the end of your normal routine) is a powerful hormetic stressor. It triggers a massive sympathetic response followed by a robust, enduring parasympathetic rebound. It trains your system to handle stress and recover efficiently, increases norepinephrine (improving focus and mood), and reduces inflammatory cytokines. Start gradually and consult a doctor if you have cardiovascular concerns.
These techniques are your first-aid kit. But to build lasting resilience, you must also address the foundational pillars of health: how you move, what you eat, and how you sleep. We begin with the most potent medicine of all—physical activity.
Exercise is not just for fitness; it’s fundamental neurochemical and anti-inflammatory therapy. However, not all exercise is equal in the context of stress management. The goal is to apply the right “dose” at the right time, without adding to your allostatic load.
When under high stress, more intense exercise is often the wrong answer. Overtraining is a significant source of allostatic load.
Movement should leave you feeling energized, not depleted. It’s a tool for building capacity, not burning out. To support this new, intentional approach to activity, technology can be a guide. Using a device that provides accurate heart rate zoning and recovery feedback helps you stay in the therapeutic Zone 2 range and honors your body’s need for rest, turning exercise from a blind grind into a precise prescription. For more on tailoring movement to your unique physiology, you can explore related topics on the Oxyzen blog.
What you put into your body is equally potent. Food is not just calories; it’s information that directly influences inflammation, gut health, and hormonal balance.
Your diet can either fuel the inflammatory fire or extinguish it. An anti-stress diet focuses on stabilizing blood sugar, supporting the gut-brain axis, and providing the raw materials for neurotransmitter and hormone production.
Hydration is also key; even mild dehydration increases cortisol. This nutritional approach isn’t about restriction; it’s about strategic nourishment to armor your biology against stress. The ultimate form of nourishment, however, happens not at the table, but in bed. The quality of your sleep determines your next day’s resilience.
Sleep is non-negotiable for stress resilience. It’s when your brain cleans house, your hormones rebalance, and memories are processed. You must protect it fiercely. This goes beyond “getting 8 hours” to engineering the quality of those hours.
Your body needs a signal that the day is ending. A 60-minute wind-down ritual is essential.
This is where tracking provides its most immediate value. By reviewing your sleep data, you can move beyond generic advice to personalized troubleshooting.
By treating sleep as a sacred, measurable pillar of health, you directly lower allostatic load and enhance every other intervention. To see how others have transformed their recovery through data, the real-world experiences shared on Oxyzen testimonials can be a powerful motivator.
In our hyper-connected world, our environment extends far beyond the bedroom. Our digital ecosystem is a constant, often unmanaged, source of cognitive and emotional stress.
Your smartphone and computer are not just tools; they are environments you inhabit. The constant pings, infinite scroll, and comparison culture of social media constitute a profound and novel stressor on the human nervous system. Managing this digital environment is a non-negotiable aspect of modern prevention.
Each notification—a text, email, or social media like—triggers a micro-dose of dopamine, the “craving” neurotransmitter. This conditions your brain to seek out the distraction, fragmenting your attention. This state of continuous partial attention keeps your nervous system in a low-grade alert, elevating cortisol and preventing deep focus or relaxation.
Reclaim your cognitive capacity. When working, use full-screen mode and close unnecessary tabs. When eating, just eat. When talking to someone, make eye contact. Single-tasking reduces cognitive load, lowers stress, and increases the quality and efficiency of everything you do.
By taking control of your digital environment, you reclaim your attention and reduce a massive, silent source of allostatic load. This act of reclaiming agency is itself empowering. And empowerment is bolstered by one of humanity’s oldest and most potent buffers against stress: community.
Humans are a social species. Our connections aren't just pleasant; they are biologically protective. Loneliness and social isolation are now recognized as risk factors for mortality on par with smoking and obesity. Conversely, strong social bonds act as a “social immune system,” dampening the harmful physiological effects of stress.
Positive social interaction and physical touch (a hug, a pat on the back) trigger the release of oxytocin, often called the “bonding hormone” or “cuddle chemical.” Oxytocin directly counteracts stress by:
It’s not about the number of friends, but the quality of a few key relationships.
In an age of digital connection, prioritize face-to-face or voice-to-voice interaction whenever possible. The nonverbal cues and shared presence are irreplaceable for our nervous systems. The story of human wellness is, at its heart, a story of community. At Oxyzen, this belief in connection and shared growth is part of the foundational vision, which you can learn more about by exploring our story.
With these eight strategic pillars in place—from breathwork to nutrition, sleep to social connection—you have a robust toolkit. But a toolkit is only as good as the system that organizes it. The final, and most critical, step is weaving these threads into a sustainable, personalized, and adaptive life practice.
A burst of motivation leads to short-term change. A system leads to lifelong resilience. The goal is not perfection, but consistent practice and intelligent adaptation. Your protocol must be personal, flexible, and reinforced by feedback.
Aim for consistency, not perfection. If you nail your sleep routine, nutrition, and movement 80% of the time, the 20% of life’s inevitable deviations (travel, holidays, crises) will not derail you. This mindset reduces the “stress about being stressed” that comes from an all-or-nothing approach.
Synthesize your subjective and objective data into a simple weekly review. This could be a Sunday evening 15-minute ritual where you:
Your biometric device is not a judge; it’s a coach and a mirror. Its purpose is to provide objective feedback, reveal hidden patterns, and celebrate progress. It turns the invisible—your nervous system state—into something visible and manageable. When you see your HRV climb over months of consistent practice, it’s not just a number; it’s quantifiable proof of your growing resilience.
This journey of prevention is one of the most profound investments you can make in yourself. It’s a shift from being a passenger in your health to becoming the pilot, with a full instrument panel to guide you. It’s about building a life not defined by the avoidance of disease, but by the active cultivation of vitality, clarity, and enduring strength.
You now possess a comprehensive blueprint—the fundamental science and the core practices for building resilience. This knowledge positions you far ahead of the curve. But life is not a controlled laboratory; it presents unique phases, professions, and personal predispositions that demand a more nuanced approach. This final section is for the advanced practitioner: it’s about refinement, personalization, and navigating the complex realities of a lifelong commitment to prevention. We move from building a strong foundation to mastering the art of adaptation.
Not all stress is created equal, and neither should be your response. A surgeon, a software engineer, a teacher, and a caregiver all face distinct stress profiles. Furthermore, your innate personality—whether you’re a natural worrier or a thrill-seeker—shapes your biological reaction. Identifying your archetype allows for hyper-targeted interventions.
Understanding your archetype removes the guilt of a "one-size-fits-all" approach not working. It empowers you to customize your toolkit. For many, this customization is aided by professional guidance, which serves as the master key to unlocking deeper patterns.
Your personal protocol is powerful, but it has limits. There are times when the guidance of a professional is not a sign of failure, but the ultimate act of proactive self-care. Knowing when and who to turn to is a critical skill.
Investing in professional support is investing in expert leverage for your health. It accelerates progress and ensures you’re addressing issues at the right level. Part of a sophisticated approach also involves understanding your unique genetic blueprint.
While lifestyle is the dominant factor, your genes load the gun; your environment pulls the trigger. Understanding key genetic polymorphisms can help you personalize your protocol with even greater precision. Note: This is for educational purposes. Always consult a healthcare professional for genetic testing and interpretation.
This gene produces an enzyme that clears dopamine, norepinephrine, and estrogen from the prefrontal cortex.
This gene is crucial for methylation, a billion-times-a-second biochemical process vital for DNA repair, neurotransmitter production, detoxification, and managing inflammation.
Understanding these predispositions isn't about determinism; it's about empowerment. It explains why your friend thrives on three coffees while you get jittery from one, allowing you to craft a diet and supplement strategy that supports your unique biochemistry. The narrative of your health is a combination of this genetic script and the lifelong story you write with your daily choices. As that story unfolds, your needs will evolve.
Resilience is not a static achievement; it's a dynamic process. Your body and life circumstances change—through hormonal shifts, career transitions, family dynamics, and aging. Your prevention protocol must be a living document, evolving with you.
Your biometrics are your early-warning system. A gradual, sustained downward trend in HRV over months, despite a consistent routine, is a signal that something needs to change—perhaps your training is too intense, a hidden stressor is at play, or your nutritional needs have shifted. Conversely, positive trends validate what’s working. This long-term relationship with your own data cultivates a profound kind of self-knowledge: not just how you feel, but how you function. To see how a commitment to this long-term view shapes a brand’s mission, you can explore the vision behind Oxyzen and its focus on lifelong wellness.
Weaving together genetics, life stages, professional guidance, and daily data creates a truly personalized medicine approach. It leads us to the final, holistic synthesis: a philosophy of prevention that transcends mere disease avoidance.
At its apex, the journey from understanding the stress-disease link to building a personalized protocol culminates in something greater than the sum of its parts. It evolves into a fundamental philosophy of living—a shift in identity from a passive patient to an active, empowered architect of your own vitality.
This philosophy rejects the notion that chronic disease is an inevitable lottery or simple genetic fate. It embraces the empowering, evidence-based truth that your daily choices have a profound and predictable influence on your long-term health trajectory. You are not helpless. The science of psychoneuroimmunology has shown that your mind, your nervous system, and your immune system are in constant, dynamic conversation. You have access to the dials in that conversation through your breath, your thoughts, your movement, and your nourishment.
In this framework, success is measured not only by the absence of illness but by the presence of positive states:
Your biometric data, from HRV to sleep stages, becomes a quantifiable proxy for these qualities. A high, variable HRV isn't just a "good number"; it's a biomarker of resilience and adaptability. A night of rich deep sleep is a biomarker of cellular repair and cognitive readiness.
Embracing this philosophy has a ripple effect that extends beyond the individual. When you become calmer, more resilient, and more energized, you show up differently in the world—as a more present partner, a more patient parent, a more focused colleague, and a more compassionate member of your community. You break the cycle of stress that can be transmitted through families and workplaces. Your personal prevention becomes a subtle but powerful form of social contribution.
We began by exploring a dangerous, invisible link: the causal pathway from the daily pressures of modern life to the chronic diseases that define our age. We followed the biology from a stressful thought to hormonal cascade, to inflammation, to cellular dysfunction. It was a story of hidden danger.
But we have ended with a story of profound hope and agency. That same biology is malleable. The HPA axis can be recalibrated. Inflammation can be quelled. Neuroplasticity allows the brain to rewire itself away from anxiety and towards calm. The gut can heal. And we now have the tools—both ancient and cutting-edge—to measure, manage, and direct this process.
The relationship between daily stress and chronic disease is not a sentence. It is a map. And with this map in hand, you are no longer wandering. You are navigating.
You now have the foundational science, the practical toolkit, and the advanced frameworks for personalization. You understand the value of auditing your stress, regulating your nervous system, moving and eating with purpose, optimizing your sleep, curating your digital world, leaning into connection, and seeking expert guidance when needed. You see this not as a chore list, but as a synergistic system—a personalized prevention protocol that you own and adapt for life.
This is the promise of modern wellness: not just living longer, but living better. With more vigor, more clarity, more peace, and more resilience in the face of whatever life brings. It starts with a single, intentional breath. It is sustained by the daily, conscious choices that, over time, write the story of your health. The next chapter is yours to write.