Emotional Balance During Hormonal Transitions: Pregnancy, Menopause, Andropause
Journaling helps achieve balance by externalizing and processing emotions, identifying patterns, and gaining perspective.
Journaling helps achieve balance by externalizing and processing emotions, identifying patterns, and gaining perspective.
Our bodies are symphonies of chemical messengers, with hormones conducting the intricate rhythms of life. From the exhilarating crescendo of new beginnings to the profound, quieter movements of maturity, hormonal transitions define our most significant life chapters. Yet, for all their biological necessity, periods like pregnancy, menopause, and andropause can feel like emotional tempests. The very chemicals that guide growth, reproduction, and aging also hold immense sway over our moods, mental clarity, and sense of inner peace.
Achieving emotional balance during these times is not about suppressing natural changes or striving for a constant, placid state. It’s about navigating the waves with understanding, tools, and resilience. It’s about transforming a period of potential turmoil into one of profound insight and growth. This journey requires a new kind of awareness—a deep, data-informed connection to the body's subtle signals that often whisper before they shout.
In an age where we can track everything from our steps to our sleep, a critical piece of the wellness puzzle has remained elusive: the objective, continuous measurement of our nervous system's state, which is the very foundation of emotional regulation. This is where modern technology, like the advanced sensors in a smart ring from Oxyzen, is beginning to bridge the gap. By providing real-time insights into stress, recovery, and physiological readiness, these tools offer a compass for the uncharted emotional landscapes of hormonal change.
This article will serve as your comprehensive guide. We will explore the hormonal and emotional realities of pregnancy, menopause, and andropause not as medical pathologies, but as natural life phases. We will delve into the science of the mind-body connection, and provide actionable strategies—from nutrition and movement to mindfulness and tech-enabled biofeedback—to help you cultivate unshakeable emotional balance. Consider this a roadmap back to yourself, equipped with both ancient wisdom and cutting-edge understanding.
To navigate the emotional waves of hormonal transition, we must first understand the conductors of this complex symphony. Hormones are far more than biological switches for reproduction; they are potent neuro-modulators that directly influence brain chemistry, neural pathways, and, consequently, our every feeling.
Estrogen: The Mood-Stabilizing Maestro
Often labeled the "female" hormone, estrogen's role is vast and vital for all genders. In the brain, estrogen promotes the production and activity of serotonin, the neurotransmitter most associated with feelings of well-being and happiness. It also enhances the effects of endorphins, our natural painkillers and mood elevators, and supports the health of brain cells themselves. When estrogen levels rise and fall dramatically—as they do premenstrually, postpartum, and during perimenopause—the brain's serotonin supply can become erratic. This directly undermines emotional stability, leading to increased susceptibility to anxiety, irritability, and sadness. Understanding this link is the first step in depersonalizing the emotion; it's not "you," it's a biochemical shift that you can learn to manage.
Progesterone: The Natural Calming Agent
If estrogen is the energizing conductor, progesterone is the soothing one. It has a natural calming, almost sedative effect on the brain by interacting with GABA receptors—the same receptors targeted by anti-anxiety medications. High levels during pregnancy contribute to that characteristic fatigue and emotional placidity for some. However, its rapid decline after childbirth or during the luteal phase of the menstrual cycle can create a pronounced withdrawal effect, leading to tension, sleeplessness, and a heightened stress response. The ratio of estrogen to progesterone is often more critical than their absolute levels, and imbalances in this delicate dance are at the heart of many emotional disturbances.
Testosterone: The Fuel for Motivation and Well-Being
Testosterone's influence on emotion is frequently overlooked. Beyond its role in libido and muscle mass, it significantly impacts motivation, confidence, and overall zest for life. It helps regulate dopamine, the "reward and drive" neurotransmitter. Declining testosterone in andropause (or due to chronic stress at any age) can therefore manifest not as rage, but as a flattening of affect—a loss of passion, increased fatigue, brain fog, and a subtle, pervasive melancholy. This "grumpy old man" stereotype is less about irritability and more about a dwindling internal spark.
Cortisol: The Stress Spoiler
While not a sex hormone, cortisol is the critical wildcard in any hormonal transition. Chronic stress elevates cortisol, which directly disrupts the production and balance of estrogen, progesterone, and testosterone. It can create a state of "pregnenolone steal," where the precursor hormone for sex hormones is diverted to make more cortisol. This means that during life phases already taxing the hormonal system, unmanaged stress can dramatically worsen the emotional fallout. Learning to measure and manage cortisol through its physiological proxies—like heart rate variability (HRV)—is a non-negotiable skill for modern emotional resilience. Devices like the Oxyzen ring can provide invaluable feedback here, helping you see which activities truly lower your stress load versus those that merely feel relaxing.
The takeaway is profound: our emotions during these transitions are not character flaws or weaknesses. They are intelligent, albeit sometimes overwhelming, signals from a body undergoing a profound metamorphosis. By understanding the players, we can move from feeling victimized by our chemistry to becoming its informed steward.

Pregnancy is often portrayed as a time of radiant joy and serene anticipation. While it certainly contains those moments, the emotional reality is a far richer, more complex tapestry. It is a nine-month odyssey of creation where a woman's hormonal landscape undergoes changes more dramatic than at any other time in her life, directly sculpting her emotional experience.
The Trimester Rollercoaster: Hormones in Motion
The first trimester is frequently dominated by surging levels of human chorionic gonadotropin (hCG) and estrogen, which can lead to profound nausea ("morning sickness") and intense fatigue. The emotional correlate is often a confusing mix of excitement and a sense of being overwhelmed or unwell. The second trimester, as hormones plateau somewhat, brings the famous "glow"—a period of increased energy, emotional stability, and the joyous first flutters of movement. The third trimester, however, introduces new challenges. Soaring levels of estrogen and progesterone prepare the body for birth but can also lead to heightened anxiety about delivery, nesting instincts, physical discomfort, and sleep disruptions that fray emotional resilience.
Beyond "Baby Blues": Understanding Perinatal Mood States
The postpartum period is a hormonal cliff dive. Within 24-48 hours of delivery, estrogen and progesterone levels plummet to pre-pregnancy levels. This sudden withdrawal, combined with sleep deprivation, physical recovery, and identity shift, creates the perfect storm for emotional disturbance.
Cultivating Balance While Building a Human
Navigating this odyssey requires a proactive, multi-faceted approach to support emotional well-being.
Pregnancy teaches that emotional balance is not a static destination but a dynamic practice of self-awareness and support, honoring both the profound joy and the legitimate challenges of creating new life.
If pregnancy is an odyssey of creation, menopause is a profound metamorphosis. It is not merely an "end" of fertility, but a complex, multi-year transition—perimenopause—that reshapes a woman's biology and, potentially, her sense of self. The emotional experience of this phase is deeply intertwined with the most significant hormonal recalibration since adolescence.
Perimenopause: The Unpredictable Prelude
Perimenopause, which can begin up to a decade before the final period, is often the most emotionally tumultuous phase. It is characterized not by low hormones, but by wild, unpredictable fluctuations in estrogen and progesterone. One day, levels may be surging (causing anxiety, irritability, or heavy periods); the next, they may plummet (triggering tearfulness, night sweats, and brain fog). This hormonal rollercoaster directly impacts the brain's limbic system, the seat of emotion. The result can be a feeling of losing one's emotional footing—unexpected rage over minor inconveniences, sudden waves of grief, or anxiety that appears out of nowhere. Many women report, "I don't feel like myself," a statement that is neurologically accurate as their brain chemistry undergoes irregular shifts.
Menopause: The Neurological Recalibration
After the final period (menopause), estrogen settles at a permanently low level. The brain, which has depended on estrogen for serotonin support and neuronal health, must now adapt to a new normal. For some, this stabilization brings emotional relief from the rollercoaster of perimenopause. For others, the loss of estrogen's neuroprotective effects can contribute to a higher vulnerability to low mood, anxiety, and cognitive changes like memory lapses. The emotional impact is also inseparable from the physical symptoms—chronic sleep disruption from night sweats, joint pain, and changes in body composition—which can erode resilience and quality of life over time.
Reframing the Narrative: From Decline to Ascension
The cultural narrative around menopause has often been one of loss and decline. A modern, empowering reframe is to see it as an ascension—a transition into a phase of life characterized by greater wisdom, clarity, and freedom. Hormonally, the end of the fertile cycle can mean an end to the monthly emotional tides governed by the menstrual cycle. Many women discover a new, more stable internal rhythm. This period can be an invitation to shed old roles and expectations and redefine life on one's own terms. Emotional balance here is not about recapturing youthful hormonal states, but about building a new, robust foundation of well-being suited for the decades ahead.
Strategies for a Sovereign Transition
Menopause, approached with knowledge and proactive care, is not an end but a gateway to one of the most authentic, powerful, and emotionally balanced chapters of a woman's life.

While lacking the clear biological marker of menopause, andropause—or age-related decline in testosterone—is a very real hormonal transition affecting men, typically beginning in their 40s and 50s. Its emotional signature, however, is often subtle, slow, and misattributed, earning it the label "the silent shift." Unlike the fluctuating storms of perimenopause, andropause is more like a gradual ebbing tide, with profound implications for emotional and mental well-being.
Testosterone's Emotional Portfolio
Testosterone's influence on the male psyche is profound yet underappreciated. It is a key regulator of:
When testosterone declines gradually by about 1% per year after 30, the effects are insidious. A man might not feel "sad" in a classic sense, but he may feel a growing sense of apathy, a loss of enthusiasm for hobbies and work he once loved, and chronic, unexplained fatigue. Irritability can stem from this deep-seated depletion rather than anger. This constellation of symptoms is too often written off as "just getting old" or the pressures of midlife, leaving the underlying hormonal component unaddressed.
The Vicious Cycle: Stress, Belly Fat, and Low T
Andropause is frequently exacerbated by modern lifestyle factors, creating a vicious cycle. Chronic stress elevates cortisol, which directly suppresses testosterone production and tells the body to store visceral (belly) fat. This fat tissue contains an enzyme called aromatase, which converts the remaining testosterone into estrogen. Thus, a man with low T can paradoxically have higher estrogen levels, which can further disrupt mood, contribute to weight gain, and create tender or enlarged breast tissue. Breaking this cycle requires targeted intervention on stress, diet, and exercise simultaneously.
Diagnosis & the Treatment Conversation
Diagnosing andropause requires a blood test measuring total and, crucially, free testosterone (the bioavailable form), ideally taken in the morning when levels are highest. Symptoms are the primary indicator; lab ranges are broad and often debated. Treatment options, primarily Testosterone Replacement Therapy (TRT), are medical decisions with significant benefits and potential risks that must be carefully weighed with an endocrinologist or urologist. The goal is not to achieve the levels of an 18-year-old, but to restore optimal function and relieve symptoms that impair quality of life.
Reclaiming Vitality: A Proactive Blueprint
Emotional balance during andropause is about reclaiming a sense of agency and vitality.
Andropause, when named and addressed, transforms from a silent decline into a navigable transition—an opportunity to optimize health, redefine strength, and build an emotionally rich second half of life.
The emotional turmoil of hormonal transitions is not "all in your head" in the dismissive sense; it is, in fact, a deeply rooted conversation between your glands and your brain. Understanding this bidirectional highway—the endocrine-nervous system connection—is the key to moving from passive victim to active participant in your emotional health.
The HPA Axis: The Central Stress Circuit
At the heart of this conversation is the Hypothalamic-Pituitary-Adrenal (HPA) axis, the body's central stress response system.
Under acute stress, this is life-saving. However, during prolonged hormonal transitions, the HPA axis can become dysregulated. For example, the estrogen withdrawal of perimenopause can make the hypothalamus more sensitive, leading to an exaggerated stress response (more hot flashes, more anxiety). Conversely, high chronic cortisol from life stress can suppress the HPA axis and disrupt sex hormone production, worsening transition symptoms. It's a vicious feedback loop.
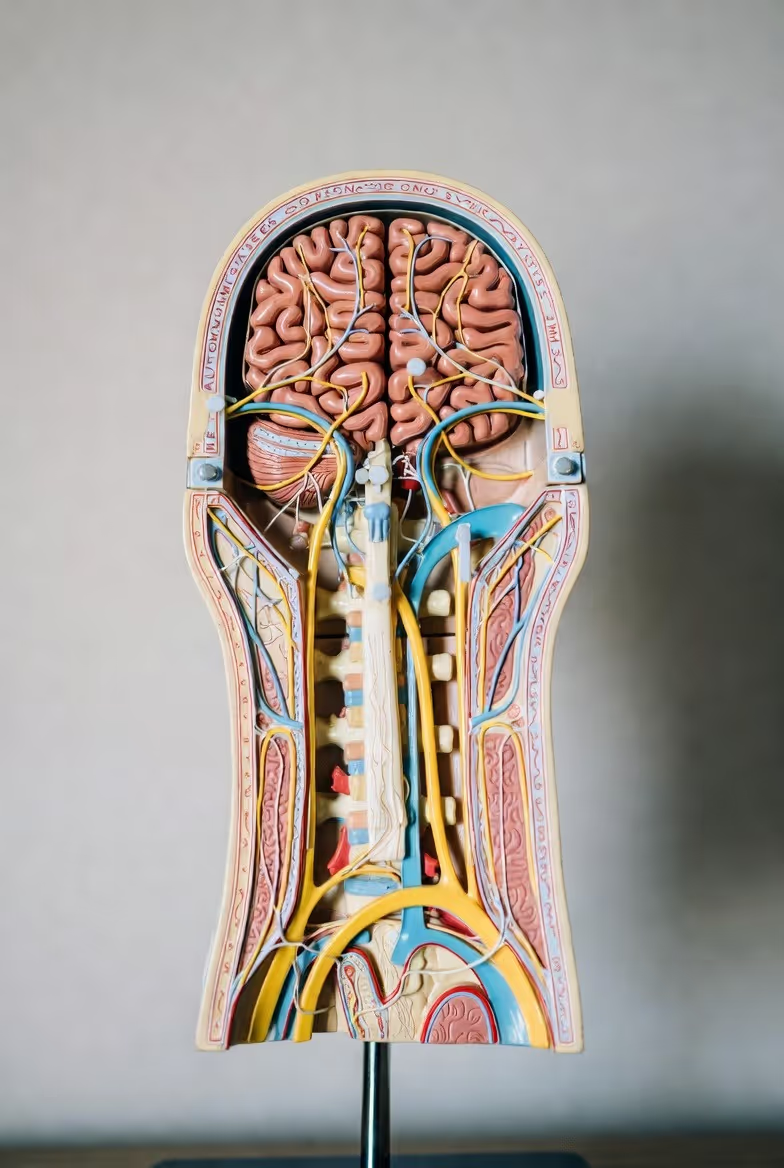
The Vagus Nerve: Your Calming Superhighway
While the HPA axis is the gas pedal for stress, the Vagus Nerve is the brake. This longest cranial nerve is the commander of the Parasympathetic Nervous System (PNS)—the "rest and digest" state. A high "vagal tone" means your body can efficiently switch off the stress response, leading to better emotional regulation, lower inflammation, and improved resilience. Hormones directly influence vagal tone. For instance, estrogen has been shown to support vagal activity, which is one reason why its decline can make calming down feel harder.
Neuroplasticity: Your Brain's Ability to Adapt
The great news is that your brain is not a static organ. It possesses neuroplasticity—the ability to rewire itself based on experience and behavior. This means that even as hormones shift, you can actively train your brain for better emotional balance. Consistent practices like mindfulness meditation have been shown to physically thicken the prefrontal cortex (the rational, calming part of the brain) and shrink the amygdala (the fear center). You are not stuck with the brain chemistry you have today.
Leveraging the Bridge for Balance
How do we apply this science? We intervene on both sides of the bridge.
You are not at the mercy of your hormones. By understanding the mind-body bridge, you can cultivate practices that soothe your nervous system, support your endocrine system, and build an emotionally resilient brain, regardless of the hormonal weather.

Before exploring advanced techniques, we must cement the non-negotiable trilogy of emotional resilience: sleep, nutrition, and movement. During hormonal transitions, these are not just lifestyle choices; they are foundational medicines that directly modulate hormone production, sensitivity, and metabolism. Ignoring them is like trying to build a castle on sand.
Sleep: The Nightly Hormone Rebalancing Act
Sleep is when your body performs critical endocrine maintenance. Growth hormone (vital for repair and metabolism) is released. Cortisol is dialed down. The balance of hunger hormones (ghrelin and leptin) is reset. For women in perimenopause, night sweats and insomnia directly sabotage this process, creating a cycle where poor sleep worsens hormonal imbalance, which in turn worsens sleep. Prioritizing "sleep hygiene" is essential: a cool, dark room; a consistent bedtime; a wind-down routine free from blue light. Here, technology can be an ally, not an enemy. A smart ring that tracks sleep stages, disturbances, and overall quality—like the one offered by Oxyzen—provishes objective data. You can see the direct impact of that late-night glass of wine or evening meditation on your deep sleep percentage, moving from guesswork to informed strategy.
Nutrition: Food as Information for Your Endocrine System
Every meal is a packet of instructions sent to your hormones.
Movement: The Dose-Dependent Hormone Modulator
Exercise is a potent endocrine modulator, but the type and intensity matter greatly.
This foundational trilogy works synergistically. Good sleep improves willpower for healthy food choices. Proper nutrition fuels effective workouts. Movement promotes deeper sleep. When this cycle is virtuous, you build a fortress of physiological resilience that can withstand the hormonal winds of change.
In the quest for emotional balance, subjective feelings can be misleading. You might feel calm while your heart rate is elevated, or feel rested after a night of fragmented sleep. This is where modern technology performs its magic: it translates the invisible language of your autonomic nervous system into objective, actionable data. This field, known as biofeedback or Quantified Self, is revolutionizing personal wellness, especially during unstable hormonal periods.
Heart Rate Variability (HRV): The Gold Standard of Resilience
HRV is not your heart rate, but the subtle variation in time between each heartbeat. A higher, more variable HRV generally indicates a healthy, adaptable autonomic nervous system with strong vagal tone—meaning you can efficiently switch from stress (sympathetic) to calm (parasympathetic). A low, less variable HRV suggests a system stuck in a stressed or fatigued state.
Resting Heart Rate (RHR) & Respiratory Rate: Vital Signs of Recovery
Your resting heart rate, taken first thing in the morning, is a simple but powerful indicator. A sustained elevation often signals systemic stress, inflammation, or inadequate recovery. Similarly, an elevated respiratory rate during sleep can indicate stress, sleep apnea, or other disturbances. These metrics, tracked over time, provide a dashboard of your body's readiness for the day.
Sleep Architecture: Beyond Just Hours in Bed
Knowing you slept 7 hours is good. Knowing you spent 90 minutes in deep sleep (critical for physical repair) and 2 hours in REM sleep (critical for emotional processing and memory) is transformative. Hormonal transitions famously disrupt sleep architecture—stealing deep sleep or causing frequent awakenings. By tracking sleep stages, you can see the direct efficacy of interventions: does magnesium glycinate increase my deep sleep? Does avoiding food 3 hours before bed reduce my wake-ups?
From Data to Wisdom: The Biofeedback Loop
The true power lies in closing the loop. This is active biofeedback:
This process demystifies self-care. You're no longer just "trying to relax"; you're training your nervous system, with proof of progress. For anyone navigating the fuzzy, emotional terrain of a hormonal transition, this clarity is empowering. It shifts the narrative from "What's wrong with me?" to "Here's what my body needs today." To understand how this is applied in a wearable format, you can explore the science behind Oxyzen's approach, which is built on making this complex data accessible and meaningful.
Technology does not replace intuition; it refines it. It provides a mirror to your inner state, allowing you to become the expert on your own body during its most profound changes.
When hormones fluctuate, the mind often follows, pulled into whirlpools of rumination, anxiety, or reactive emotion. Mindfulness and meditation are the ancient, now scientifically-validated anchors in this storm. They don't stop the waves, but they teach you how to surf them. More importantly, they actively rewire the brain, strengthening the circuits for calm, clarity, and compassion precisely when they are most needed.
The Neuroscience of Stillness
Functional MRI studies show that consistent meditation practice:
Practical Practices for Transitional Phases
You don't need to sit for an hour. Micro-practices woven into your day are incredibly effective.
The Synergy with Biofeedback
This is where mindfulness meets modern science. Using a device that tracks HRV, you can engage in a biofeedback-enhanced meditation. You watch in real-time as your coherent breathing and focused attention cause your HRV to rise and your heart rate to slow. This is not theoretical; it's immediate, visual proof that your mind is directly regulating your body. It reinforces the practice and provides undeniable motivation. Many users find that this synergy accelerates their progress, as detailed in real-world experiences shared by our community.
Mindfulness is the ultimate inner technology. It provides the software update your brain needs to run smoothly on a new hormonal operating system, fostering an emotional equilibrium that is responsive, not reactive.
Our hormones do not exist in a vacuum, and neither do our emotions. They are constantly shaped and reflected in our social and relational ecosystems—our partnerships, families, friendships, and communities. During hormonal transitions, which can make us feel isolated in our experience, the quality of these connections becomes either a potent buffer against emotional distress or a significant amplifier of it.
Communication: Translating Your Inner Experience
One of the greatest challenges is communicating what you're going through when you may not fully understand it yourself. "I'm just so irritable" or "I have no energy" can be misinterpreted by partners, children, or colleagues as disinterest or hostility.
Partnership Dynamics Under Hormonal Pressure
Intimate relationships are often ground zero for emotional fallout.
Finding Your Tribe: The Power of Shared Experience
There is immense therapeutic power in being with people who "get it." This could be:
Professional Support: Therapy and Coaching
Sometimes, the best support is professional. A therapist trained in Cognitive Behavioral Therapy (CBT) or Acceptance and Commitment Therapy (ACT) can provide powerful tools for managing anxiety and depressive thoughts. A health coach or a functional medicine practitioner can help navigate the labyrinth of lifestyle and supplement choices. Reaching out for this help is a sign of strength and commitment to your well-being, not a failure.
Your emotional balance is a shared project. By intentionally cultivating a supportive ecosystem—through clear communication, educated loved ones, empathetic communities, and professional guidance—you build a safety net that allows you to navigate the inevitable dips with far greater grace and security.
Hormonal transitions are not merely biological events; they are profound existential passages. Pregnancy is a confrontation with creation, mortality, and legacy. Menopause is a passage from a fertility-centric identity into a new, undefined chapter. Andropause often coincides with a reevaluation of one's achievements and legacy. The emotional turbulence, therefore, isn't just about chemistry—it's also about the soul's search for meaning amidst change. Addressing this dimension is critical for deep, lasting emotional balance.
The "Why" as an Emotional Anchor
Victor Frankl, the neurologist and Holocaust survivor, wrote in Man's Search for Meaning that those who could find a purpose could endure almost any "how." During the disorienting "how" of hot flashes, sleepless nights, or crushing fatigue, reconnecting to your "why" provides an immovable anchor.
Spiritual Practices for Grounding and Surrender
Spirituality, in a non-dogmatic sense, refers to practices that connect us to something larger than our individual selves and our immediate problems.
The Gift of the Second Half: Post-Transitional Potential
Many cultures venerate the post-reproductive years as a time of heightened spiritual power and social leadership. Without the demands of fertility and often intense career-building, there is potential for unparalleled creativity, insight, and contribution. The emotional balance found here is not the precarious balance of juggling many roles, but the deep, solid balance of a tree with widespread roots—grounded in a strong sense of self and purpose.
This journey of meaning is deeply personal. At Oxyzen, we believe technology should support not just the body, but the holistic human journey. Our mission, which you can read more about here, is to provide the self-awareness tools that create the mental and emotional space for this deeper work to unfold. When you are not constantly battling the raw symptoms of dysregulation, you have the energy to ask the bigger questions and build a life of profound alignment.
While a whole-food, nutrient-dense diet is the irreplaceable cornerstone, hormonal transitions can create demands that are difficult to meet through food alone. Stress, altered digestion, and the sheer increased need for certain cofactors can create functional deficiencies. Targeted supplementation acts as a strategic support system, but it is not a substitute for a poor lifestyle. The principle here is "test, don't guess," and always consult with a knowledgeable healthcare provider.
Adaptogens: The Stress-Response Modulators
Adaptogenic herbs help the body adapt to stress by modulating the HPA axis. They are not stimulants nor sedatives but bring balance (homeostasis).
Hormonal Pathway Supporters
These nutrients directly support the body's own hormone production, metabolism, and detoxification.
Botanical Support for Specific Transitions
The Gut-Hormone Connection: Probiotics
Given the gut's role in metabolizing and clearing hormones (the estrobolome) and producing neurotransmitters, a high-quality, multi-strain probiotic is a wise foundational supplement. It supports gut barrier integrity, reducing inflammation that can dysregulate the HPA axis.
A Critical Note on Quality and Testing
The supplement industry is poorly regulated. Choose brands that are third-party tested for purity and potency (look for NSF, USP, or Informed-Sport seals). It’s highly advisable to work with a functional medicine practitioner or naturopath who can order comprehensive nutrient and hormone testing to identify your specific deficiencies and needs, creating a protocol that is both safe and effective. For more insights on integrating data with wellness choices, our blog features deep dives on specific nutrients.
When lifestyle, dietary, and supplemental strategies are insufficient to restore quality of life, medical interventions become a critical conversation. This is a deeply personal decision that must be based on current evidence, individual risk profile, and severity of symptoms. Being an informed advocate for your own health is paramount.
Hormone Therapy (HT) for Menopause: A Nuanced Renaissance
The narrative around HT has evolved dramatically since the early 2000s. The current understanding is more nuanced, emphasizing timing, type, and individualization.
Testosterone Replacement Therapy (TRT) for Men
For men with clinically diagnosed hypogonadism (symptoms + consistently low blood tests), TRT can be transformative.
SSRIs/SNRIs: Not Just for Depression
Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) are commonly prescribed for the mood and anxiety symptoms of hormonal transitions. They are also, interestingly, a first-line non-hormonal treatment for menopausal hot flashes. Low doses of certain SSRIs like paroxetine or the SNRI venlafaxine can significantly reduce the frequency and severity of vasomotor symptoms. They can be a viable option for women who cannot or choose not to use HT, or as an adjunct to HT for mood-specific issues.
Integrative Mindset: "And," Not "Or"
The most effective approach is often integrative. A person might use:
This layered strategy treats the whole person. It’s crucial to have a healthcare team that respects this integrative model. For questions on how data from wearables can inform conversations with your doctor, our FAQ resource can be a helpful starting point.
Knowledge is only power when applied. The final step is synthesizing all this information into a living, breathing, personalized plan that fits your unique life, preferences, and symptoms. This is not about perfection, but about progressive, consistent adaptation.
Step 1: Establish Your Baselines
You cannot manage what you do not measure. Before making sweeping changes, take a 1-2 week "observation period."
Step 2: Prioritize and Sequence Interventions
Trying to change everything at once is a recipe for burnout. Use the "crowding out" principle and the hierarchy of needs.
Step 3: Create Your "Toolkit" for Acute Moments
Have pre-planned responses for when emotional or physical symptoms flare.
Step 4: Cultivate the "Observer" Mindset
This is the meta-skill. It’s the ability to step back and say, "Ah, my progesterone has dropped this week, and my HRV is lower. That’s why I’m feeling this tearfulness. It’s a phase, not my truth." This depersonalizes the symptom, reduces secondary suffering (the anxiety about the anxiety), and allows you to calmly deploy your toolkit. Your wearable data is the ultimate tool for fostering this observer mindset, providing an impartial report on your state. Seeing how others have used this data to transform their self-awareness can provide powerful inspiration.
The ultimate goal of navigating hormonal transitions is not merely to survive them, but to emerge on the other side with a refined blueprint for lasting vitality. This requires shifting our perspective from viewing these phases as isolated problems to be "fixed," toward seeing them as the body’s profound invitation to upgrade our entire approach to health for the decades to come. It’s about redefining what "normal" aging can look like when we are active participants.
From Symptom Management to Systems Optimization
The early stages of a transition are often crisis-driven, focused on quelling the most disruptive symptoms. The long game, however, is about proactive, systemic optimization. The same practices that soothe hot flashes or boost low mood—stress resilience, quality sleep, strength training, anti-inflammatory nutrition—are also the primary drivers of "healthspan": the number of years we live in good health.
In this light, the hormonal transition is not a derailment but a catalyst, forcing a necessary and beneficial upgrade to your lifestyle operating system.
Redefining the Narrative of Midlife and Beyond
Our culture often frames aging as a story of decline, loss, and irrelevance. The hormonal transitions of midlife challenge us to write a new narrative—one of ascension, integration, and power.
This new narrative isn't about denying the very real challenges, but about placing them in a larger, more empowering context. It’s about seeing yourself not as a collection of declining parts, but as an integrated, wise, and resilient system entering a distinct and potent new season. This philosophy is core to the vision behind tools designed for lifelong wellness, a vision you can explore in our company's story.
Building a Legacy of Health
The long game is also intergenerational. How you navigate your transition becomes a model for your children, your partner, your friends, and your community. By approaching it with curiosity, proactive care, and a refusal to accept unnecessary suffering, you normalize a new path. You demonstrate that aging can be met with agency, that vitality is not the sole province of the young, and that emotional balance is a skill honed over a lifetime. This legacy—of empowered, informed, and vibrant aging—may be one of your most significant contributions.
We are on the cusp of a revolution in how we understand and manage hormonal health. The convergence of continuous biometric sensing, artificial intelligence, and advanced diagnostics promises a future where hormonal balance is not a mystery but a dynamically managed aspect of our daily lives.
Beyond the Snapshot: Continuous Hormonal Biomarker Sensing
The future lies in moving beyond the static, stressful blood draw—a single snapshot in time—to continuous, non-invasive monitoring. Imagine:
The Role of AI and Predictive Analytics
With continuous data streams, artificial intelligence becomes a powerful co-pilot for your health.
The Empowered Patient and the Collaborative Care Model
This technology shifts the paradigm from a passive patient receiving instructions to an empowered human owning their health data. You become the expert on your own body’s patterns. The role of the doctor, therapist, or coach evolves into that of a guide who helps you interpret the data, navigate complex decisions (like HT or TRT), and provide the human touch, wisdom, and accountability that machines cannot.
Ethical Considerations and the Human Touch
This exciting future comes with important caveats. Data privacy and security are paramount. The "quantified self" must not become a source of obsessive anxiety or a new standard for perfectionism. The goal of all this technology is to support human flourishing—to create more mental space, more physical vitality, and more emotional freedom, not to become another taskmaster. The core practices of mindfulness, connection, and purpose will always remain the bedrock; technology is merely a sophisticated tool to help us engage with them more effectively. For a deeper look at how we balance cutting-edge tech with human-centric design, our about page details our core philosophy.
This future is not distant. Devices like the Oxyzen ring, which already provide sophisticated nervous system insights, are the foundational step into this new era of bio-awareness, paving the way for the even more granular hormonal insights to come.
In navigating hormonal transitions, common questions and concerns arise. Here, we address some of the most frequent queries with evidence-based, compassionate clarity.
1. "Is what I'm feeling normal, or is it something more serious?"
This is the fundamental question. A good rule of thumb: Duration, Intensity, and Interference.
2. "Can I balance my hormones naturally without medication?"
For many, yes—especially when symptoms are mild to moderate. The "natural" path is the comprehensive foundation we’ve built: stress mastery (via tools like biofeedback wearables), sleep optimization, anti-inflammatory nutrition, targeted supplementation, and consistent movement. This approach addresses root causes like inflammation and HPA axis dysregulation. For others with more severe symptoms or specific medical histories, a combination of natural supports and medication (HT, SSRIs) is the most effective, integrative path. It’s not a binary choice.
3. "How do I talk to my doctor about this without being dismissed?"
Come prepared. This shifts the dynamic from "I’m complaining" to "I’m presenting data."
4. "Will hormone therapy make me gain weight / cause cancer?"
These are the most common fears.
5. "My partner is going through this and it’s affecting us. How can I help?"
Your support is invaluable. The best way to help is to:
For more detailed answers to technical or product-specific questions, a great resource is our comprehensive FAQ page.
The path through pregnancy, menopause, andropause, and any hormonal transition is a hero’s journey. It begins in the known world of your former physiological balance, calls you into the unfamiliar and often frightening forest of fluctuating emotions and changing identity, and, if navigated with courage and awareness, returns you to yourself—not the old self, but a wiser, more resilient, and more authentically integrated version.
The Core Truths to Carry Forward:
The First Step Begins Now
You do not need to implement everything at once. Start with one thing. Perhaps it’s committing to a consistent bedtime. Maybe it’s adding 10 minutes of mindful walking to your day. Or, it could be deciding to gather more information about your own body through tracking or testing.
The goal of this entire exploration is to empower you to move from a place of confusion and reaction to one of clarity and proactive creation. To see your hormonal transition not as an ending, but as a beginning—the beginning of a deeper relationship with your body, a more compassionate dialogue with your mind, and a more intentional design for the vibrant, emotionally rich life that awaits on the other side.
Your journey to unshakeable balance is yours to chart. We are here to provide the maps, the tools, and the community to support you along the way. To learn more about how a data-informed approach can illuminate your unique path, we invite you to explore what’s possible.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/