How Sleep Quality Determines Recovery Effectiveness
Sleep quality—uninterrupted cycles—determines recovery effectiveness more than just total sleep duration alone.
Sleep quality—uninterrupted cycles—determines recovery effectiveness more than just total sleep duration alone.
You've crushed your workout. You've meal-prepped like a champion. You're hydrating religiously. Yet, you're still plateauing, perpetually sore, and running on fumes. What if the single most powerful lever for your recovery—and by extension, your performance, health, and vitality—isn't something you do at all, but something you stop doing for eight hours a night? We live in a culture obsessed with optimization, yet we routinely sabotage the body's primary, non-negotiable repair cycle: sleep.
Recovery isn't merely the absence of activity; it's an active, intricate, and biologically mandated process of restoration. And its headquarters is the silent, dark theater of the night. This isn't about logging "hours in bed." This is about the quality of the sleep architecture within those hours—the precise sequencing of brain waves, the hormonal symphony, the cellular cleanup—that determines whether you merely rest or genuinely rebuild.
Modern technology, like advanced wellness wearables, now allows us to move beyond guesswork. Devices such as the Oxyzen smart ring peel back the curtain on the night, translating the cryptic language of your sleep into actionable data on readiness, recovery, and long-term resilience. For a deeper look at how this technology personalizes your health insights, you can explore our complete guide on how Oxyzen works.
In this exploration, we will dissect the profound, non-linear relationship between sleep quality and recovery effectiveness. We will journey into the neurobiology of the sleeping brain, the endocrinology of the nightly repair crew, and the practical strategies that transform sleep from a passive state into the most potent performance-enhancing "tool" in your arsenal. The road to peak performance, it turns out, is paved with good sleep.

Recovery is a term thrown around in gyms, boardrooms, and wellness circles, but its full meaning is often diluted. In a physiological sense, true recovery is the process by which your body returns to homeostasis—a state of stable, optimal functioning—after the stress of exertion, whether that stress is physical, cognitive, or emotional.
When you lift weights, you create microscopic tears in muscle fibers. When you solve complex problems, you deplete neurotransmitters and metabolic fuel in the brain. When you navigate a stressful day, you elevate cortisol and sympathetic nervous system activity. All of these states represent a controlled departure from baseline. Recovery is the journey back, but with a crucial twist: adaptation. The goal is not just to return to where you started, but to overcompensate, to rebuild stronger, smarter, and more resilient than before. This principle is called supercompensation.
Think of it like this: Stress (training, work, life) is the input that breaks you down. Recovery is the essential process that builds you back up. Without adequate recovery, the stress simply accumulates, leading to plateaus, burnout, injury, and illness—a state often referred to as overtraining syndrome or allostatic overload.
In our modern context, recovery is multidimensional:
While modalities like nutrition, hydration, massage, and mindfulness play supportive roles, they are largely facilitating the main event. The vast majority of the literal, structural repair and systemic reset happens during one specific biological state: deep, high-quality sleep. To ignore sleep quality is to ignore the very engine of recovery itself. Understanding this holistic view of health is central to our mission at Oxyzen, which you can read more about in our story here.
If you believe sleep is a uniform state of unconsciousness, you're missing the entire plot. Sleep is a dynamically structured, highly active process composed of distinct stages that cycle throughout the night in a precise pattern known as sleep architecture. This architecture is the blueprint for recovery, and its integrity—the depth, proportion, and continuity of each stage—is what defines true sleep quality.
Sleep is divided into two broad types: NREM (Non-Rapid Eye Movement) and REM (Rapid Eye Movement) sleep. NREM is further broken down into three stages (N1, N2, N3), with N3 representing the holy grail of physical restoration: Slow-Wave Sleep (SWS), or deep sleep.
The Sleep Cycle Unpacked:
A full sleep cycle (N1 → N2 → N3 → N2 → REM) lasts about 90-110 minutes and repeats 4-6 times per night. The composition of each cycle changes as the night progresses: early cycles are rich in deep N3 sleep, while later cycles feature longer periods of REM.
Sleep Quality vs. Sleep Quantity: You can be in bed for 9 hours and still have poor sleep quality if your architecture is fragmented. Frequent awakenings (even micro-awakenings you don't recall), insufficient time in deep or REM sleep, or a misaligned circadian rhythm that disrupts the normal cycling all degrade the blueprint. The result? You wake up unrefreshed because the essential "construction work" of recovery was interrupted. Tracking these nuanced stages is where modern wellness technology shines, providing insights far beyond simple duration. For more resources on interpreting your own sleep data, our blog offers a wealth of related articles.
While you sleep, your endocrine system conducts a precise, time-released symphony of hormones. This chemical cascade is the direct mechanism through which sleep quality dictates recovery effectiveness. Disrupt the sleep, and you disrupt the music, leading to a cacophony that promotes breakdown over buildup.
The Anabolic (Building) Hormones:
The Catabolic (Stress) Hormone:
The Metabolic Regulators:
The Practical Implication: When sleep quality is high, the hormonal symphony plays as written: HGH and testosterone surge to repair muscles, melatonin quiets inflammation, cortisol stays low, and appetite hormones remain balanced. When sleep is fragmented or short, the symphony falls apart: cortisol rises, growth hormone plummets, and hunger signals go haywire. Your body literally shifts from a state of repair to a state of stress storage. Understanding these internal rhythms is the first step to harmonizing with them, a principle that guides the development of tools designed to provide this clarity.
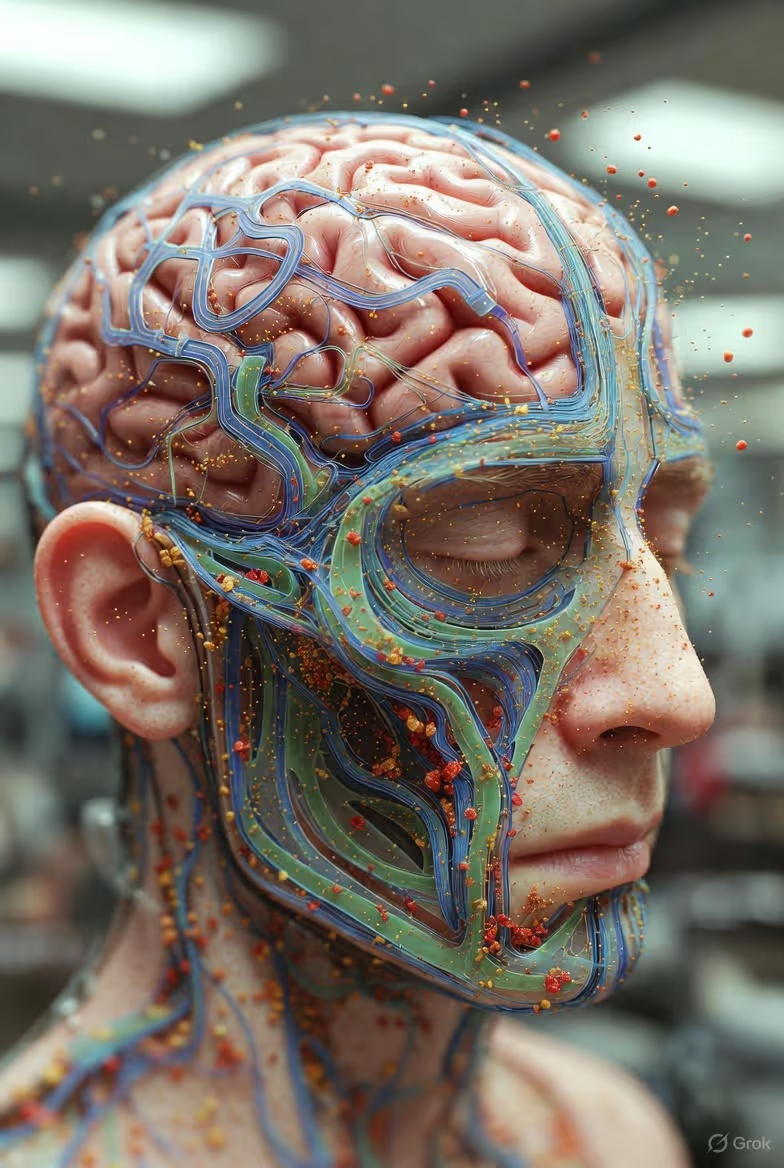
One of the most groundbreaking discoveries in neuroscience this past decade has unveiled a critical recovery process that occurs exclusively during deep, quality sleep: the activation of the glymphatic system.
Think of your brain as a complex, 24/7 metropolis. During the day, neuronal activity generates metabolic waste products, including toxic proteins like beta-amyloid (associated with Alzheimer's disease) and tau. If this waste accumulates, it impairs cognitive function, clouds thinking, and contributes to long-term neurodegeneration.
The glymphatic system is the brain's dedicated sanitation department, and it only works the night shift. During deep NREM sleep, glial cells in the brain actually shrink in size, increasing the interstitial space by over 60%. This allows cerebrospinal fluid (CSF) to rush through these newly expanded channels, flushing out the accumulated metabolic debris and transporting it to the body's circulatory system for disposal.
This nightly "brainwash" is non-negotiable for cognitive recovery. It clears the fog of mental fatigue, restores processing speed, and is essential for long-term brain health. Poor sleep quality, particularly a lack of sustained deep sleep, severely impairs this cleansing process. You wake up not only tired but with a "dirty" brain—cluttered, slow, and inefficient.
This concept extends beyond the brain. On a systemic level, sleep is when the body prioritizes detoxification pathways in the liver, repairs cellular damage through autophagy (the recycling of old cellular components), and reduces systemic inflammation. The antioxidant activity of melatonin further supports this nightly cleanup. In essence, high-quality sleep is the master reset button for your entire biological system, clearing the decks for a new day of optimal function.
For anyone engaged in physical training—from elite athletes to weekend warriors—this is the most tangible connection between sleep and recovery. The soreness you feel after a hard workout (Delayed Onset Muscle Soreness, or DOMS) is the inflammatory response to microscopic muscle damage. Sleep is the construction site where that damage is rebuilt into stronger tissue.
The process is elegantly direct:
Sleep quality directly modulates this entire process:
Simply put, you can have the perfect post-workout protein shake, but if you don't enter the deep sleep "repair zone," you are denying your body the hormonal environment it needs to use those building blocks effectively. The workout provides the stimulus, but sleep is the adaptation. Many of our users at Oxyzen have tracked this direct correlation, sharing how sleep metrics predict their physical readiness—see their real-world experiences in our testimonials.
Physical repair is only half the story. Your brain, arguably your most important organ for navigating daily life, undergoes its own intensive recovery program each night. Sleep quality is the determinant of whether you wake up with a sharp, agile, and emotionally stable mind or a foggy, reactive, and forgetful one.
Memory Consolidation & Learning: Sleep is not a time of mental inactivity; it's a period of intense filing and integration. The hippocampus (the brain's short-term memory buffer) and the neocortex (long-term storage) engage in a dynamic dialogue.
Synaptic Homeostasis: The "Synaptic Homeostasis Hypothesis" proposes that wakefulness strengthens synaptic connections throughout the brain, which increases energy needs and cellular stress. Slow-wave sleep (N3) acts as a global downscaler, selectively weakening less important connections to restore balance, improve efficiency, and make space for new learning the next day. Poor sleep leaves your neural networks in a state of noisy, saturated overload.
Emotional and Psychological Recovery: The amygdala, the brain's emotional center, is highly regulated by sleep, particularly REM. During REM, the brain processes emotional experiences in a neurochemical environment low in norepinephrine (a stress neurotransmitter), allowing us to "file away" the emotional charge of events. Sleep deprivation hyper-activates the amygdala and weakens its connection to the prefrontal cortex (the rational regulator), leading to heightened emotional reactivity, anxiety, and poor stress management.
In summary, cognitive recovery through sleep means wiping the mental slate clean, organizing the day's information, defragging the hard drive, and recalibrating your emotional compass. It is the ultimate biohack for mental performance and resilience.

The link between "catching a cold" after poor sleep is not an old wives' tale; it's hard immunology. Sleep is a fundamental pillar of immune function, and its quality directly determines your body's ability to defend itself, reduce inflammation, and respond to vaccines.
Sleep and Innate Immunity: During deep sleep, the production of cytokines—a type of protein that targets infection and inflammation—is increased. These molecules are both warriors and signals, coordinating the body's defense. Sleep deprivation reduces the production of these protective cytokines and infection-fighting antibodies.
Sleep and Adaptive Immunity: Sleep enhances the function of T-cells, the white blood cells that are critical for adaptive immunity. When you sleep, the levels of stress hormones like adrenaline and noradrenaline (which can inhibit T-cell function) drop, giving your immune system a window to operate at full strength. Research shows that people who sleep less than 7 hours are nearly three times more likely to develop a cold than those who sleep 8 hours or more when exposed to the rhinovirus.
Inflammatory Regulation: Chronic, systemic inflammation is a root cause of numerous diseases and a major barrier to recovery. Sleep, particularly deep sleep, acts as a powerful anti-inflammatory. It suppresses the production of pro-inflammatory cytokines like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). Poor sleep quality creates a state of low-grade chronic inflammation, impairing muscle repair, increasing perception of pain, and raising the risk for long-term health issues.
Vaccine Response: Studies on flu, hepatitis, and other vaccines consistently show that individuals with shorter or poorer sleep in the days surrounding vaccination produce a significantly weaker antibody response. Your body needs the restorative sleep state to properly "learn" from the vaccine and build durable immunity.
By prioritizing sleep quality, you are effectively running a nightly scan and update on your immune system, ensuring your defenses are patched, vigilant, and ready. This aspect of holistic wellness is a key focus in the insights provided by comprehensive health tracking.
Understanding the isolated benefits of sleep is one thing. Seeing how poor sleep actively unravels your other recovery efforts is where the picture becomes truly alarming. It creates a vicious, self-reinforcing cycle that is difficult to escape.
1. Nutrition & Metabolism: As mentioned, sleep disruption dysregulates leptin and ghrelin. This leads to increased hunger, cravings for sugary and fatty foods, and a tendency to consume more calories overall. Furthermore, sleep loss induces insulin resistance. Your cells become less responsive to insulin, meaning glucose stays in the bloodstream longer, promoting fat storage and energy crashes. So, despite eating with recovery intent, your body is hormonally primed to store fat and struggle to use nutrients efficiently.
2. Exercise Performance & Safety: Sleep-deprived individuals have slower reaction times, reduced accuracy, decreased strength and endurance, and impaired decision-making. This not only leads to subpar workouts but significantly increases the risk of injury. Your motivation to train also plummets, as perceived exertion feels much higher. You're less likely to engage in the very activity that drives adaptation.
3. Stress & Mindset: Poor sleep elevates baseline cortisol and amplifies the stress response to daily challenges. This creates a feedback loop: stress disrupts sleep, and poor sleep increases stress susceptibility. Your psychological resilience erodes, making you less likely to stick to healthy routines and more likely to seek quick, dopamine-driven rewards (like junk food or scrolling).
4. Pain Perception: Sleep loss lowers pain thresholds. That nagging ache or soreness becomes more pronounced, further discouraging movement and activity, which are themselves often part of the recovery solution (e.g., active recovery).
The cycle is clear: Bad sleep → Poor food choices + Sluggish workouts + Higher stress + More pain → Worse recovery → Even worse sleep. Breaking this cycle requires a deliberate, data-informed intervention, starting with honoring the sleep recovery process. For those navigating this challenge, our FAQ page addresses common questions on optimizing sleep and recovery.
For decades, sleep and recovery were black boxes. We relied on subjective feelings of "tiredness" or "soreness." The advent of advanced, user-friendly biometric tracking has revolutionized our ability to quantify the unseen and move from guessing to knowing.
This is where devices like the Oxyzen smart ring come into play. Worn continuously, it moves beyond the step-counting paradigm of wrist-based fitness trackers to measure the biomarkers most relevant to recovery:
By synthesizing this data, a smart ring doesn't just tell you how long you slept; it provides a Readiness or Recovery Score. This score is a composite metric (often incorporating HRV, RHR, sleep data, and activity balance) that answers the critical question: "Is my body prepared for stress today, or does it need more restoration?"
This objective feedback loop is transformative. It allows you to:
Technology demystifies the process, turning sleep quality from an abstract concept into a manageable, optimizable variable in your overall health equation. To discover how this approach is applied in a real-world product, you can learn more about the Oxyzen smart ring technology here.

Armed with the why, we now arrive at the actionable how. Optimizing sleep quality for maximal recovery is not about a single magic trick; it's about building consistent, supportive habits around what sleep scientists call "sleep hygiene." These are the non-negotiable pillars.
1. Light: Master Your Circadian Rhythm
Your body's master clock, the suprachiasmatic nucleus (SCN), is exquisitely sensitive to light.
2. Temperature: The Goldilocks Zone
Core body temperature must drop to initiate and maintain sleep. A cool room (around 65-68°F or 18-20°C) is ideal. Take a warm bath or shower 90 minutes before bed; the subsequent drop in core temperature as you leave the bath signals sleepiness.
3. Routine: Signal Safety to Your Nervous System
A consistent, wind-down routine acts as a behavioral cue for sleep. This could include light stretching, meditation, reading a physical book, or journaling. The key is consistency and avoiding stimulating activities.
4. The Sleep Sanctuary
Your bedroom should have one primary function: sleep. Optimize it:
5. Nutrition & Substance Timing
6. Consistency is King
Go to bed and wake up at the same time every day, even on weekends. This is perhaps the most powerful tool for reinforcing a robust circadian rhythm and improving sleep quality.
Implementing these pillars creates the optimal external and internal environment for the hormonal symphony, glymphatic cleanup, and musculoskeletal repair to proceed without interruption. It is the deliberate cultivation of the conditions in which recovery can thrive. For ongoing tips and deeper dives into each of these pillars, our blog is regularly updated with expert insights.
Mastering the foundational pillars of sleep hygiene is like building a stable, solid house. The advanced strategies we explore now are akin to fine-tuning that house’s internal systems—optimizing airflow, perfecting the lighting, and ensuring the structure supports peak performance. These methods go beyond general advice, targeting the specific architecture of your sleep to maximize the time spent in the crucial deep (N3) and REM stages.
Sleep Cycle Syncing and Wake-Time Management
Your sleep cycles are roughly 90 minutes long. Waking up at the end of a cycle, during light N1 or N2 sleep, results in far greater alertness than being jolted from deep N3 or REM sleep (a phenomenon known as sleep inertia). You can leverage this by planning your wake-up time to coincide with the end of a cycle.
Strategic Nutrient Timing for Neurotransmitter Support
The biochemistry of sleep is driven by neurotransmitters. You can support their production through specific nutrients consumed at strategic times.
Temperature Manipulation Protocols
We know a cool room is vital, but we can be more proactive.
Mindfulness & Cognitive Techniques for Sleep Onset
A racing mind is one of the biggest thieves of sleep quality. Techniques that quiet the prefrontal cortex are essential.
By layering these advanced strategies onto a solid foundation, you transition from simply getting sleep to actively engineering your sleep for superior recovery outcomes. The goal is to create the perfect internal milieu for your body’s innate repair processes to operate at full capacity.
When nighttime sleep is insufficient or when extraordinary physical or mental demands are placed on the body, a strategically timed nap can serve as a powerful tool to bolster recovery. However, not all naps are created equal. The timing and duration of a nap determine its cognitive and physical benefits—and its potential drawbacks.
The Science of Nap Sleep Stages:
Just like at night, your nap will progress through sleep stages if it’s long enough. The key is to target specific stages for specific outcomes without entering others that cause grogginess.
The "No Man's Land" Nap (30-50 minutes): This is generally the worst duration. You are likely to be woken from deep N3 sleep, leading to significant sleep inertia—that groggy, disoriented feeling that can last over an hour.
Strategic Implementation for Recovery:
For individuals using recovery-tracking technology, observing how a nap impacts your afternoon or evening Heart Rate Variability (HRV) and Resting Heart Rate (RHR) can provide objective feedback on its effectiveness. Did your metrics improve, indicating genuine recovery, or did a poorly timed nap disrupt your rhythm? This data-driven approach turns napping from a guessing game into a precision tool, a concept many explore in the broader wellness content on our blog.
Despite impeccable sleep hygiene and advanced strategies, some individuals will continue to struggle with unrefreshing sleep and poor recovery. This is a critical red flag that may indicate an underlying sleep disorder. These are medical conditions that fragment sleep architecture and prevent deep, restorative sleep, no matter how long you are in bed. Recognizing the signs is the first step toward seeking professional help and reclaiming your recovery.
Common Sleep Disorders That Thwart Recovery:
The Recovery Impact & The Path to Diagnosis:
These disorders create a state of constant physiological stress. With OSA, for example, the nightly battle to breathe spikes cortisol and adrenaline, while the brain is starved of oxygen and deep sleep. The body remains in a catabolic, pro-inflammatory state, making physical and cognitive recovery nearly impossible. It also dramatically increases long-term health risks.
What to Do If You Suspect a Disorder:
Ignoring a potential sleep disorder means fighting for recovery with one hand tied behind your back. Effective treatment can be the single most impactful intervention for restoring sleep quality and, by extension, all downstream recovery processes. If you're gathering data and need to understand what certain signals might mean, our FAQ section can be a helpful starting point for common questions.
The architecture of sleep and its role in recovery is not static. It undergoes profound changes from childhood through old age, altering our requirements and vulnerabilities. Understanding these shifts allows for age-appropriate expectations and strategies.
Childhood & Adolescence: The Construction Phase
Early & Mid-Adulthood: The Performance and Maintenance Phase
Later Adulthood & The Senior Years: The Preservation Phase
Key Takeaway: While the amount of deep, restorative sleep we can generate may change, its non-negotiable role in recovery does not. The strategies must adapt—from supporting massive growth in youth, to enabling high performance in mid-life, to preserving critical function in later years. Honoring sleep is a lifelong commitment to recovery and health.
Viewing sleep solely through the lens of next-day recovery misses the larger, more ominous picture. Chronic poor sleep quality is not a badge of honor; it is a slow-acting metabolic poison and a primary driver of the most prevalent non-communicable diseases in the modern world. The long-term recovery we should be most concerned about is the body's ability to recover from and resist chronic illness.
The Pathophysiology of Sleep-Linked Disease:
The Recovery Perspective: Every night of high-quality sleep is an investment in your long-term health capital. It is a proactive, preventative measure that reduces all-cause mortality risk. When we talk about recovery effectiveness, we must expand the timeline. It’s not just about being ready for tomorrow’s workout; it’s about ensuring your body’s systems are recovering from the microscopic insults of daily life in a way that doesn’t accumulate into pathology. This profound connection between nightly repair and lifelong health is a core part of our vision and the reason Oxyzen was created.
We have journeyed through the science, the strategies, and the stakes. Now, we arrive at the synthesis: building a dynamic, personalized protocol that uses data and self-awareness to inextricably link your sleep quality to your recovery outcomes. This is not a rigid set of rules, but a flexible framework for intelligent adaptation.
Step 1: Establish Your Baselines (The Discovery Phase)
You cannot optimize what you do not measure. For 2-4 weeks, focus on consistency with the foundational pillars while gathering data.
Step 2: Identify Levers and Patterns (The Analysis Phase)
After a few weeks, look for correlations. This is where insight becomes power.
Step 3: Implement Targeted Interventions (The Experimentation Phase)
Based on your analysis, run single-variable experiments for 1-2 weeks each.
Step 4: Create Your Dynamic Decision Matrix (The Personalization Phase)
This is the culmination: a set of personalized, data-informed guidelines.
The Living Protocol: Your protocol is never finished. It evolves with your age, fitness level, stress load, and goals. The technology that provides your data is the feedback loop that keeps it honest. By engaging in this process, you move from being a passive recipient of your recovery to an active architect of it. You begin to make decisions not based on arbitrary schedules or ego, but on the objective language of your own physiology. For those ready to begin this journey of personalized insight, you can learn more about starting with Oxyzen here.
Sleep is the undisputed cornerstone of recovery, but it does not operate in a vacuum. It exists within a holistic ecosystem of wellness practices. When strategically aligned, these practices create a powerful synergy, each amplifying the effects of the other. Think of sleep as the master contractor; nutrition, hydration, and movement are the specialized subcontractors that show up to do their best work when the job site (your body) is properly prepared and managed.
Nutrition: Fueling the Nightly Repair Crew
What you eat, and when you eat it, provides the raw materials for the repair processes that occur during sleep. Without the right building blocks, even perfect sleep architecture can only achieve partial recovery.
Hydration: The River of Recovery
Water is the medium in which every metabolic process, including cellular repair and detoxification, occurs. Dehydration thickens the blood, strains the cardiovascular system, and can lead to muscle cramps that disrupt sleep.
Active Recovery: Movement as a Sleep Enhancer
The relationship between movement and sleep is bidirectional and profoundly positive when managed correctly.
The Integrated Protocol: A day designed for optimal recovery might look like this: A morning workout followed by a protein-rich breakfast; consistent hydration throughout the day; a balanced lunch and dinner with complex carbs and healthy fats; a 20-minute walk after dinner; a casein-based snack or magnesium supplement 90 minutes before bed; and finally, a lights-out ritual in a cool, dark room. Each element supports the next, creating a virtuous cycle culminating in profound, high-quality sleep. For more on crafting these synergistic daily routines, our blog features numerous guides and tips.
In the realm of sleep and recovery, misinformation abounds. These myths can lead to counterproductive habits that sabotage recovery efforts. Let’s dismantle the most pervasive ones with evidence-based science.
Myth 1: "You Can Catch Up on Sleep on the Weekend."
Myth 2: "Watching TV/Scrolling Helps Me Wind Down."
Myth 3: "If I Can't Sleep, I Should Just Lie in Bed Until I Do."
Myth 4: "Alcohol Helps You Sleep Better."
Myth 5: "Older Adults Need Less Sleep."
Myth 6: "Snoring is Normal and Harmless."
By replacing these myths with scientific facts, you empower yourself to make choices that genuinely support, rather than undermine, your sleep-based recovery. Clearing up confusion is a key part of our mission, which is why we maintain a robust FAQ section to address these and other common questions.
We are on the cusp of a revolution in how we understand, measure, and optimize sleep for recovery. The frontier is moving beyond tracking what happened to proactively influencing what will happen. Here are the most promising trends that will define the next decade of sleep science.
1. Closed-Loop Sleep Systems
Imagine a wearable device that doesn't just read your biometrics but responds to them in real-time to improve your sleep. Early prototypes are exploring this:
2. Precision Sleep Nutrition & Chronopharmacology
The future of sleep supplements is personalization. Rather than a generic melatonin pill, we’ll see:
3. Advanced Biomarkers and Predictive Analytics
Future wearables will move from descriptive to predictive and prescriptive.
4. Circadian Medicine and Light Optimization
We will see a greater integration of light as medicine.
5. Neurofeedback and Sleep Training
Direct training of the brain for better sleep is becoming more accessible.
The overarching theme is personalization and proactive intervention. The goal is a seamless integration of technology into the sleep environment, creating a true "recovery ecosystem" that works autonomously to foster the perfect night's sleep. This visionary approach to holistic health is what drives innovation in companies focused on this space, including the vision behind Oxyzen's development journey.
For too long, sleep deprivation has been worn as a badge of honor—a symbol of dedication, hustle, and toughness. We glorify the CEO who brags about 4-hour nights and the athlete who "outsleeps" the competition. This cultural narrative is not only backwards but actively harmful. The most profound recovery intervention we can make is not a new supplement or gadget; it’s a collective mindset shift that elevates sleep to the same non-negotiable status as nutrition and exercise.
Sleep as a Performance Multiplier, Not a Time Sink
The data is unequivocal: in domains requiring precision, creativity, and decision-making—from boardrooms to operating rooms to athletic fields—superior sleep quality is the ultimate performance enhancer. Studies on NBA players show a direct correlation between increased sleep time and improved sprint times, shooting accuracy, and mental well-being. Corporations like Google and Goldman Sachs have instituted sleep hygiene programs because they’ve quantified the cost of tired employees in errors, accidents, and lost innovation. We must reframe sleep not as lost productive time, but as an investment that yields compound interest in clarity, creativity, and efficiency.
The Economic and Healthcare Imperative
The societal cost of poor sleep is staggering. The RAND Corporation estimated that sleep deprivation costs the U.S. economy up to $411 billion annually in lost productivity. In healthcare, the costs of treating conditions directly caused or exacerbated by poor sleep—diabetes, heart disease, depression—are astronomical. Promoting sleep health is a public health imperative with a clear economic return on investment. Insurance companies are beginning to incentivize good sleep, and forward-thinking employers are offering sleep-tracking benefits alongside health insurance.
Creating Sleep-Supportive Environments
This shift must manifest in our policies and environments:
The Personal Ethos: Becoming a Steward of Your Recovery
On an individual level, this shift means giving yourself permission to prioritize sleep without guilt. It means:
When we, as a society, begin to view a well-slept individual not as lazy, but as disciplined, prepared, and investing in their long-term capacity, we will unlock a new tier of human potential and well-being. It is a quiet, powerful revolution that begins in the dark, in the profound and essential work of the night. This broader mission of empowering individuals through knowledge and tools is at the heart of our company's purpose.
We have traversed the intricate landscape where sleep quality and recovery effectiveness intersect—from the cellular cleanup of the glymphatic system and the hormonal symphony of the night, to the advanced strategies that engineer better sleep architecture and the societal structures that must change to support it. The evidence is overwhelming and the conclusion inescapable: If you are not recovering well, you are almost certainly not sleeping well.
Recovery is not a passive happenstance; it is an active, physiological process with a strict schedule, and its prime operating window is locked between the hours of 10 p.m. and 6 a.m. (or whatever your personal circadian rhythm dictates). You can have the most sophisticated training plan, the cleanest diet, and the best recovery tools available, but without providing your body with the undisturbed, high-quality sleep it requires to execute its repair protocols, you are building a palace on sand.
The journey to mastering your recovery begins with a fundamental respect for the power of the night. It requires moving beyond counting hours and toward cultivating the conditions for depth and continuity. It demands that you listen to the objective data of your body—your HRV, your sleep stages, your readiness scores—and have the wisdom to adjust your days based on the story your nights are telling.
This is not a call for perfection, but for intention. It’s about making incremental, consistent choices: choosing the book over the binge-watch, enforcing the caffeine curfew, dimming the lights, and honoring the wind-down routine. It’s about recognizing that the extra hour of sleep is a more potent performance booster than the extra hour of late-night work.
Embrace sleep not as a void, but as your most productive state of being. In its silent, dark theater, the real work is done: muscles are forged, memories are cemented, the immune system is fortified, and the mind is cleared. By mastering the night, you don't just recover from yesterday—you build a stronger, sharper, more resilient version of yourself for tomorrow.
Your greatest tool for health, performance, and longevity is already in your possession. It's time to start using it to its full potential. Let your recovery be deep, and let your days be limitless.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/