How to Measure Sleep Health Without Fancy Devices
Measure it subjectively through daytime alertness and mood, and objectively through consistency of your sleep schedule.
Measure it subjectively through daytime alertness and mood, and objectively through consistency of your sleep schedule.
Sleep. It’s the silent, invisible foundation upon which every aspect of our health is built. Yet, for something so fundamental, it remains one of life’s great mysteries. We spend roughly one-third of our lives doing it, but how many of us truly understand the quality of that time? In our tech-saturated world, the answer seems to lie in more gadgets: smart rings, sleep trackers, under-mattress sensors, and wearable bands that promise a data-driven peek into our nocturnal lives. But what if the key to understanding your sleep isn’t locked behind a $300 device and a confusing app dashboard? What if you already possess the most sophisticated tools for sleep analysis you’ll ever need?
This article is a deep exploration into the art and science of measuring sleep health without relying on fancy technology. We’re going back to the basics—to the observational, intuitive, and evidence-based methods that humans have used for centuries to gauge rest. This isn’t a rejection of modern tools; in fact, companies like Oxyzen are creating elegant solutions that harmonize technology with holistic understanding. It’s an empowerment guide. By learning to listen to your own body’s signals, you become the primary expert on your sleep. You’ll learn to distinguish between genuinely restorative rest and the deceptive lure of simply being unconscious. This foundational knowledge makes you a smarter consumer of any technology you later choose to adopt and allows you to validate its data against your lived experience.
We’ll journey through simple morning check-ins, classic pen-and-paper tracking, environmental audits, and body literacy exercises. You’ll discover how to measure sleep latency, continuity, and satisfaction using nothing more than awareness and a clock. This knowledge is liberating. It places the power of your well-being back into your hands, creating a resilient understanding of sleep that no battery drain or software glitch can ever take away. Let’s begin reconnecting with the innate wisdom of your own rest.

Before you can measure anything, you must know what you’re looking for. Sleep health is not a single number like a credit score; it’s a multidimensional construct. Fancy devices often present a simplified score (e.g., "Sleep Score: 82"), which can be useful but also reductive. Without devices, we expand our definition to encompass both objective signs and subjective feelings. By understanding these pillars, you create a framework for your own assessment.
The Core Objective Pillars (What You Can Observe):
The Core Subjective Pillars (What You Can Feel):
The goal of measuring sleep health without devices is to become a skilled observer of these pillars in your own life. You are collecting a rich, nuanced dataset of lived experience, which is often more valuable than a generic algorithm’s interpretation of your movement and heart rate. For those curious about how modern technology like smart rings attempt to quantify these pillars, you can learn more about smart ring technology and its approach.
Your first moments of consciousness are a goldmine of sleep data. Before you check your phone, before your feet hit the floor, practice this quick, mindful audit. This habit transforms vague morning feelings into concrete, actionable observations.
Step 1: The Immediate Sensory Scan.
Lie still for 60 seconds and ask yourself:
Step 2: The Recall Test.
Try to remember the night. Was it a blank void, or can you recall dreams? Even vague fragments of dreams can indicate you reached the important REM sleep stage. Conversely, remembering multiple awakenings (to use the bathroom, because of noise, etc.) is crucial data on continuity.
Step 3: The "Could I Fall Back Asleep?" Question.
This is a powerful litmus test for sleep drive. If your alarm went off and you instantly felt you could easily fall back into a deep sleep for hours, you likely have a sleep debt. If you feel reasonably alert and that returning to sleep would be difficult, your sleep drive has been adequately satisfied.
Step 4: The Mirror Check (Literal and Figurative).
Once you’re up, take a genuine look in the mirror. Look beyond the messy hair. Do you have pronounced under-eye circles or puffiness? Is your skin pale or lacking its usual glow? These can be external markers of poor sleep quality or inflammation. Then, take a figurative look at your energy. Rate your alertness on a scale of 1-10 within the first 30 minutes of waking. Log this number mentally or on paper.
By conducting this daily audit, you train your brain to connect cause and effect. You’ll start to notice, "When I eat late, I wake up feeling heavy," or "When I unwind without screens, my morning mind is clearer." This is the bedrock of personal sleep science.

Long before apps, sleep researchers used the gold-standard tool: the sleep diary. It remains one of the most effective and clinically recommended methods for assessing sleep patterns. Your diary is a non-judgmental log that reveals patterns invisible over a single night.
What to Record Each Morning:
What to Record Each Evening (Crucial for Context):
The Magic of Pattern Recognition:
After two weeks of consistent logging, put the pages side-by-side. Look for correlations without a device ever touching your wrist. Do you see that on nights you recorded "wine with dinner," you also logged "2+ awakenings" and "3/5 sleep quality"? Do you see that your "time to fall asleep" creeps above 30 minutes on Sundays, perhaps due to anxiety about the week ahead? This pattern recognition is transformative. It moves you from feeling like a victim of "bad sleep" to being a detective uncovering its specific, addressable causes. For more structured guidance and printable templates, you can always explore our blog for more wellness tips and resources.
Your body broadcasts clear physiological signals related to sleep, and you can learn to tune into this innate radio station. You don’t need a photoplethysmography (PPG) sensor to understand the basics; you just need a bit of attention.
The Heart Rate Clue:
Your resting heart rate (RHR) is a brilliant barometer of recovery and stress. While a tracker gives you a precise number, you can gauge it manually. First thing in the morning, before sitting up, find your pulse on your wrist or neck. Count the beats for 30 seconds and multiply by 2. Do this for a week to find your personal baseline. Notice: Is your RHR noticeably higher than your baseline? This can indicate your body is under stress—perhaps from poor sleep, an oncoming illness, dehydration, or lingering workout fatigue. A lower-than-baseline RHR upon waking can signal excellent recovery.
The Temperature Rhythm:
Core body temperature is central to the sleep-wake cycle. It drops to initiate sleep and rises to promote wakefulness. You can observe this without a continuous monitor.
Listening to Your Breathing:
Sleep-disordered breathing, like sleep apnea, often goes undiagnosed for years. While a full diagnosis requires a sleep study, you can note potential red flags. Do you often wake up with a very dry mouth or sore throat? Does a partner complain of loud, irregular snoring or gasping sounds? Do you suffer from crushing daytime fatigue despite spending 8+ hours in bed? These are signals worth discussing with a doctor. Observing these bodily cues creates a profound body literacy, making you an active participant in your health rather than a passive recipient of data. To understand how advanced devices integrate these physiological signals, you can discover how Oxyzen works to synthesize this data.

Your sleep environment is the stage upon which the drama of the night plays out. Measuring its suitability requires no technology, just your senses and a critical eye. A poor environment can sabotage even the most perfect sleep habits.
The Darkness Deep Dive:
True darkness is non-negotiable for melatonin production. To audit your room, lie in your bed at night with the lights off. Allow your eyes to adjust for 5 minutes.
The Soundscape Analysis:
Silence is golden, but consistency is king. Sudden, intermittent noises (a dripping tap, a dog barking, a partner’s snore) are far more disruptive than a constant, low hum of white noise. Listen intently. What do you hear? The intermittent refrigerator compressor? Distant traffic? Identify the disruptive changes in sound, not just the volume.
The Thermostat Truth:
The science is clear: most people sleep best in a cool room, around 65-68°F (18-20°C). Is your bedroom within this range? Don’t guess—use a simple, inexpensive room thermometer. Remember, it’s about the temperature of the air around you, not just your bedding.
The "Clutter & Chaos" Factor:
This is a psychological measure. Is your bedroom a sanctuary for sleep and intimacy, or is it a home office/gym/storage unit? Visual clutter creates cognitive clutter, which can raise subconscious stress levels. Does your room feel calm, ordered, and relaxing? Your immediate emotional response when you walk in at bedtime is your answer. This environmental audit empowers you to become the architect of your own sleep sanctuary, making tangible changes that yield immediate improvements.
Sleep is not an isolated event. It is the direct result of how you lived the preceding 16 hours. By measuring key behaviors during the day, you can accurately predict—and improve—your night.
Measuring Light Exposure: The Master Zeitgeber.
Light is the most powerful regulator of your circadian clock. Your goal is bright light in the morning, dim light in the evening. Audit your day:
Measuring Movement & Timing of Exercise:
Exercise dramatically improves sleep quality, but its timing matters. Vigorous exercise raises core body temperature and stimulates cortisol release. If done too close to bedtime, this can interfere with the wind-down process. Note: When did you exercise yesterday? How intense was it? How did you sleep that night? You might find a 7pm HIIT class correlates with longer sleep latency, while a 5pm gym session correlates with deeper sleep.
Measuring Stress & Cognitive Load:
The mental "to-do list" is the enemy of sleep onset. How "full" was your mind when you attempted to sleep? Were you mentally rehearsing a conversation or solving work problems in bed? This is known as "cognitive hyperarousal." Practice measuring your mental shut-down process. Can you institute a "worry journal" session 1-2 hours before bed to download thoughts onto paper, effectively taking them out of your brain’s rehearsal loop? Tracking this practice and its impact on sleep latency is a powerful non-device metric. Understanding these daily rhythms is part of a holistic wellness philosophy, something we delve into on our page about our vision and values.
You cannot effectively measure your sleep health if you are measuring it against the wrong yardstick. Your chronotype—your natural predisposition for sleeping and waking at certain times—is biologically determined, not a lifestyle choice. Are you a morning lark, a night owl, or somewhere in between? Forcing a night owl to live on a lark’s schedule creates perpetual jet lag.
The Munich Chronotype Questionnaire (MCTQ) Insights (Simplified):
You can discover your tendency without a quiz by observing your natural rhythms on vacation or free days. After 3 days without alarms or social obligations:
Measuring Social Jetlag:
This is the disconnect between your biological clock (your chronotype) and your social clock (work, school, family schedules). Calculate it: On work days, you wake up at 6:00 AM. On free days, you naturally wake at 8:30 AM. That’s a 2.5-hour difference. That is 2.5 hours of social jetlag, a chronic stressor linked to weight gain, mood issues, and poor metabolic health. Simply becoming aware of this gap is a massive step. It may not be possible to eliminate it, but you can measure its size and then work to minimize it (e.g., by not staying up quite so late on weekends, or by negotiating a slightly later work start time).
Honoring your chronotype is about working with your biology, not against it. It explains why "early morning workouts" are soul-crushing for some and life-giving for others. It reframes "laziness" as a mismatch between biology and schedule. This self-knowledge is perhaps the most profound measurement you can make.
Your pre-sleep ritual is the bridge from the wakeful world to the restful one. A weak, inconsistent bridge leads to a rocky transition. You can measure the effectiveness of this ritual by its consistency and its sensory composition.
The Consistency Metric:
Do you start a similar sequence of calming activities at roughly the same time each night? The brain thrives on predictability. A erratic routine sends no clear signal that sleep is approaching. Track for a week: What time did you start your wind-down? Was it within a 30-minute window each night? Consistency itself lowers anxiety about sleep.
The Sensory Inventory:
An effective wind-down should gently engage the "rest and digest" (parasympathetic) nervous system. Rate your ritual on these sensory dimensions:
By reviewing your ritual through this lens, you can identify weak spots. Maybe your ritual is consistent but too visually stimulating (scrolling in bed). Perhaps it’s calm but starts too late to be effective. This review turns an abstract "wind-down" into a measurable, optimizable process. For ideas on building better evening routines, our community often shares their experiences; you can read real customer reviews and routines for inspiration.
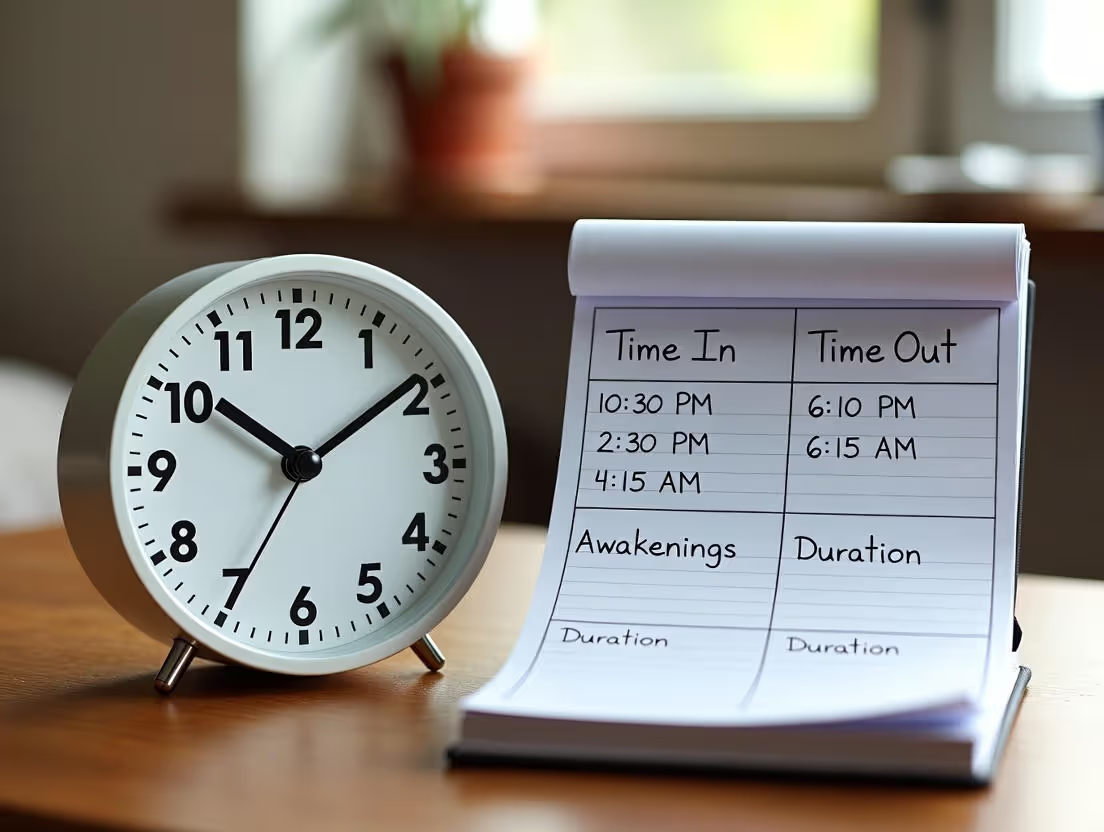
This is where we get practical and observational with classic sleep metrics. You need two tools: a dimly lit clock (or your phone face-down, checked only when needed) and a notepad by the bed.
Measuring Sleep Onset Latency:
Logging Nocturnal Awakenings:
The goal is not to panic about awakenings (brief ones are normal) but to identify patterns.
This method removes the mystery. You are no longer just "a bad sleeper." You are someone who takes 45 minutes to fall asleep on nights after late caffeine consumption, or who wakes at 3 AM when the bedroom is above 70°F. This is actionable intelligence gathered with zero fancy devices.
Ultimately, the purpose of sleep is to enable a vibrant, alert, and healthy waking life. Therefore, your daytime functioning is the most important report card for your sleep. These metrics are purely subjective but incredibly powerful.
The Energy Dip Map:
Track your energy levels at 3-4 set times during the day (e.g., 10 AM, 2 PM, 5 PM). Use a simple 1-10 scale. Where are the predictable crashes? A major post-lunch dip (2-3 PM) is circadian and normal, but its severity can be mitigated by good sleep. A mid-morning crash often points to poor sleep quality or unstable blood sugar.
The Focus and Mood Gauge:
At the end of the day, reflect:
The Caffeine Dependency Index:
This is a brilliant proxy measurement. Are you dependent on caffeine to function normally? Or is it a pleasant ritual? Ask yourself: "If I missed my morning coffee, would I get a debilitating headache and be unable to focus by noon?" If the answer is yes, it strongly suggests your natural sleep-driven alertness systems are impaired, and you are using a stimulant to mask a significant sleep debt.
By correlating your subjective nighttime observations (from your diary and audits) with these daytime metrics, you build an irrefutable case for what works and what doesn’t. You might see that on nights you score your sleep a "4" or higher, your 2 PM energy is a "6" instead of a "3," and you don’t crave a 3 PM candy bar. This connection between night and day is the holy grail of sleep health measurement. For common questions on interpreting these signals and next steps, our FAQ page offers detailed support.
After 2-4 weeks of consistent observation across these ten areas, you will be sitting on a wealth of personal data. The final step is synthesis—moving from a collection of notes to a coherent action plan. This is where you become your own sleep coach.
Step 1: Triangulate the Evidence.
Look for the same culprit appearing across multiple metrics. For example:
Another example:
Step 2: Prioritize One Keystone Change.
Don’t try to fix everything at once. Based on your synthesized data, choose the ONE intervention that seems likely to have the biggest impact. If light is your biggest disruptor, commit to a strict "no screens in bed" and "dim lights at 9 PM" rule for two weeks. If consistency is your issue, focus solely on fixing your wake-up time to within 30 minutes every single day.
Step 3: Measure the Impact of Your Intervention.
Continue your simple tracking. After two weeks of your keystone change, review your data. Has your subjective sleep quality score improved? Has your morning fog decreased? Has your sleep latency shortened? This is the scientific method applied to your own life. If it worked, the data will show it. If it didn’t, you can pivot and test a new hypothesis (e.g., maybe temperature was the bigger issue).
This self-directed process builds immense self-efficacy. You are not waiting for a gadget to tell you what to do; you are using self-knowledge to drive change. And when you do choose to incorporate technology later, you will do so from a position of knowledge, using the device to refine what you already understand, not to discover it from scratch. You become the expert, and the device becomes a useful tool in your already capable hands. To see how a thoughtful technological tool can complement this kind of deep self-knowledge, you can learn more about the Oxyzen approach and philosophy.
You have now gathered data across eleven critical dimensions of sleep—from your morning fog to your evening light, from your heart's rhythm to your room's darkness. This collection of observations isn't just notes; it’s the blueprint of your unique sleep architecture. The final, crucial step is to synthesize this information into a coherent, actionable personal baseline. This baseline is your “normal.” It is the reference point against which all future changes—whether from a new habit, a period of stress, or even a new device—will be measured.
Creating Your Sleep Health Profile:
Take a fresh page in your journal or a new digital document. Create sections that mirror the pillars you’ve been measuring. Under each, write your personal average or most common state based on your 2-4 weeks of observation.
This profile is not a judgment. It is a clear-eyed, compassionate assessment of your current reality. It is the most valuable thing you own in your quest for better sleep because it is undeniably, uniquely yours.
Identifying Your Primary Lever:
Within your profile, one or two items will stand out as the most significant barriers or the most promising opportunities. This is your "primary lever"—the single change that will yield the greatest improvement. For many, it is consistency of wake time to combat social jetlag. For others, it is the hard stop on evening screen time or the rigorous enforcement of a dark, cool bedroom. Your data will point directly to it. Your action plan for the next month should focus exclusively on pulling this one lever. This focused approach prevents overwhelm and allows you to cleanly measure the impact of a single variable.
The self-measurement journey empowers you, but it also has boundaries. A critical part of being a good self-observer is knowing when your observations indicate a need for expert help. Your non-device tracking can provide compelling evidence to bring to a healthcare professional, making your consultation far more productive.
The Red Flags in Your Data:
Consistently logging any of the following patterns warrants a discussion with your doctor or a sleep specialist:
How to Present Your Findings: Walking into a doctor's office with a detailed 4-week sleep diary and a summary of your observed red flags is powerful. Instead of saying, "I'm tired," you can say, "I've been tracking, and I average 8.5 hours in bed but subjectively rate my sleep as 2/5. I log waking up 5 times per night, and my partner reports loud snoring. My daytime energy score is consistently a 3/10 by 2 PM." This factual, data-driven approach (even without tech) facilitates a faster path to diagnosis, which may involve a professional sleep study. For those navigating the journey from observation to seeking solutions, our blog features articles on next steps and professional collaboration.
If nighttime sleep is your main financial account, a nap is a strategic, high-interest short-term investment. Done correctly, it can reboot alertness and performance. Done poorly, it can bankrupt your next night's sleep. Measuring nap effectiveness is a key skill in holistic sleep health.
The Two Measurable Nap Types:
The Nap Audit: To Assess Your Nap's Impact:
Creating a Personal Nap Protocol: Based on your audit, create a rule. For example: "If desperately tired, I may take a 15-minute power nap before 3 PM. I will set an alarm. I will not nap if I have had adequate sleep the night before." This turns napping from a guilty, uncontrolled crash into a deliberate, measured recovery tool.

What you consume is a direct chemical intervention in your sleep system. Tracking the relationship between intake and sleep is one of the most straightforward and impactful correlations you can make without any gadget.
The Caffeine Timeline:
Caffeine has a half-life of 5-6 hours. To measure its effect, log the time of your last caffeine serving (coffee, tea, soda, dark chocolate). Then, track your sleep latency that night. Do you see a pattern? For many, caffeine after 2 PM pushes sleep onset later. Your personal tolerance is your key metric.
The Alcohol Paradox:
Alcohol is a sedative but a terrible sleep aid. It reliably disrupts the second half of the night. Log: Number of drinks and time of last drink. Correlate with your log of nocturnal awakenings and morning refreshment score. You will likely find that even 1-2 drinks in the evening lead to more awakenings after 2-3 AM and a lower subjective sleep quality, despite faster initial sleep onset.
The Heavy Meal Effect:
Digestion raises core temperature and requires energy. Log your last meal size and timing. A large, rich meal within 3 hours of bed often correlates with longer sleep latency, more restless sleep, and even vivid or unpleasant dreams. Your body’s energy is directed to your gut, not restoration.
The Hydration Balance:
Dehydration can cause nighttime leg cramps and awakenings. Overhydration close to bedtime guarantees disruptive bathroom trips. Note your evening fluid intake and number of nocturnal awakenings for urination. Find your personal cutoff time where the benefit of hydration doesn't incur a continuity cost.
By treating food and drink as variables in your personal sleep experiment, you gain powerful, direct control. You move from vague advice like "avoid caffeine" to a personal, evidence-based rule: "For me, caffeine after 3 PM results in a 40+ minute sleep latency."
Stress and sleep exist in a vicious cycle: poor sleep lowers stress resilience, and high stress sabotages sleep. Breaking this cycle requires you to measure both sides of the equation.
Quantifying Pre-Sleep Cognitive Arousal:
This is the "monkey mind" metric. Each evening, rate your pre-sleep mental chatter on a scale of 1-10 (1 = calm, quiet mind; 10 = racing, anxious, problem-solving mind). Log this number. Then, correlate it with that night’s sleep latency and sleep quality score. The correlation is often stark and immediate.
The "Worry Journal" Efficacy Test:
A common intervention is to "download" your thoughts onto paper 1-2 hours before bed. To measure if this works for you:
Daytime Stress Carry-Over:
At the end of your day, briefly log your overall stress level (1-10) and the major stressors. Look for patterns over time: Do high-stress days (a score of 8+) predict poor sleep that night, or does good sleep on the prior night predict better stress handling? This reveals the directionality of your personal loop. Understanding this mind-body connection is at the heart of modern wellness, a principle that guides the mission at Oxyzen; you can read more about our commitment to this holistic approach.
You are the primary subject, but you are not the only possible source of data. Enlisting a trusted partner or even using simple audio recording can provide an "external review" that catches what self-observation misses.
The Partner Report:
If you share a bed, your partner is a invaluable sensor. Once a week, ask for calm, factual feedback. Key questions:
The Simple Audio Check:
Smartphone apps can record and analyze sleep sounds (snoring, talking, coughing). Used occasionally—not every night to avoid anxiety—this can be a diagnostic tool. A night of recorded, frequent snoring or gasps is tangible evidence to bring to a doctor. The key is to use this technology sparingly as a targeted audit, not as a nightly judge.
The "Bed Partner Impact" Metric:
Sleep is a shared ecosystem. Note how your sleep patterns affect your partner and vice versa. Do you have better continuity when sleeping alone? Does your partner’s later bedtime or different temperature preference disrupt your onset? Measuring this dynamic honestly can lead to practical solutions like separate blankets, mattress toppers, or even discussing different bedtimes.
This external audit moves you from a purely internal, subjective frame to a more rounded view. It adds a layer of objectivity to your personal dataset, making your overall assessment even more robust.
Your sleep baseline is not static. It shifts with seasons, age, and life stages. Measuring these long-wave changes prevents you from misdiagnosing a normal transition as a "sleep problem."
Seasonal Adjustments:
Track your sleep duration and morning alertness across the year. It is biologically normal to need slightly more sleep in the dark winter months and to find waking easier in the bright summer. Do your logs show a pattern of needing 30-60 more minutes of sleep in January versus July? This is normal circadian response to light, not laziness.
Hormonal Cycle Tracking (For Those Who Menstruate):
The menstrual cycle is a powerful sleep modulator. In your sleep diary, note your cycle phase. Many will see a clear pattern: improved sleep latency and quality in the follicular phase (after menstruation), and more frequent awakenings, lighter sleep, and fatigue in the luteal phase (before menstruation). Measuring this helps you attribute changes correctly—it's not "bad sleep hygiene," it's biology—and allows you to adjust expectations and self-care accordingly.
The Aging Metric:
As we age, sleep architecture changes naturally: it becomes more fragmented (more awakenings), lighter (less deep sleep), and circadian rhythms often shift earlier. If you are over 50 and logging more awakenings than you did at 30, this may be a normal change, not a disorder. The key metric is whether the daytime impairment is severe. If you wake up 3 times a night but fall back asleep easily and feel rested, that is likely age-normal. If the awakenings are long and daytime fatigue is high, it warrants investigation.
Taking the long view prevents unnecessary alarm and fosters self-compassion. You learn to differentiate between a fixable habit and a natural, manageable evolution of your sleep pattern.
You now have a baseline and have identified your primary lever. You are no longer just tracking; you are experimenting. This phase is where lasting change and deep understanding are forged.
Forming a Hypothesis:
Based on your data, state a clear, testable prediction. For example: "Hypothesis: If I stop all screen use after 9:30 PM and read a book under a warm lamp instead for 30 minutes, my average sleep latency will decrease from 30 minutes to under 20 minutes within two weeks."
Running the Experiment:
Commit to the new behavior (the "intervention") consistently for a minimum of 14 days. Maintain your core tracking—morning audit, sleep diary, daytime metrics. Keep everything else in your life as consistent as possible to isolate the variable.
Analyzing the Results:
After the period, compare your data from the experimental phase to your original baseline. Look at the specific metric you aimed to change. Did your average sleep latency drop? Did your subjective sleep quality score rise? Use both the numbers and your lived feeling as outcomes.
Iterating Your Protocol:
This iterative, self-directed approach is the essence of biohacking. It turns you from a passive patient into an active architect of your well-being. The sense of agency it creates is, in itself, a powerful sleep aid. For inspiration from others on their self-experimentation journeys, our community's testimonials often highlight these personal discoveries.
After this deep dive into self-measurement, the rationale for building this foundation before buying a gadget becomes crystal clear. You are now equipped to be a discerning, empowered user of technology, not a dependent one.
You Become Validation-Capable:
When you eventually use a sleep tracker, you can validate its data against your rich subjective dataset. If your ring says you had "great sleep" but your morning audit feels like a "2/10" and you have crushing daytime fatigue, you have the confidence to question the algorithm. You know your truth. The device becomes a secondary source to be interpreted, not an oracle to be obeyed.
You Ask Smarter Questions:
Instead of vaguely wanting to "track sleep," you will seek technology that can answer your specific, data-driven questions. "Can this device help me understand if my suspected early-morning awakenings are correlated with a rise in heart rate?" or "Can it measure the impact of my new 4 PM caffeine cutoff on my sleep stages?" You shop with intention.
You Avoid "Orthosomnia":
This is a clinical term describing the unhealthy obsession with perfecting sleep data from trackers. It creates performance anxiety around sleep, which is the antithesis of rest. With a strong foundation in subjective well-being, you are inoculated against this. You use the device to supplement your understanding, not to define your self-worth. Your primary metric remains: "Do I feel restored and function well during the day?"
You Appreciate Advanced Tech on a Deeper Level:
When you understand the struggle of manually tracking heart rate trends or guessing at sleep cycles, you can truly appreciate what a well-designed device can offer. You’ll value a tool that seamlessly tracks your temperature rhythm or provides a gentle, scientifically-timed wake-up light. You become the ideal user—one who understands the "why" behind the data. To see how a device is designed to complement this kind of foundational knowledge, you can discover how Oxyzen works from this informed perspective.
Beyond logs and checklists lies a profound measurement tool: your own mindful awareness. The Body Scan meditation, practiced in bed, is not just a relaxation technique—it’s a diagnostic powerhouse. It allows you to take a real-time inventory of physical tension and mental chatter, providing an immediate, subjective measure of your nervous system's readiness for sleep.
Executing the Diagnostic Body Scan:
Lie on your back in your sleep position. Starting at your toes and moving slowly to the crown of your head, spend 20-30 seconds on each body part. Your goal is not to fall asleep (though it may happen), but to observe without judgment.
Correlating Scan Data with Sleep Outcomes:
Log a simple note after your scan: "High tension in neck/jaw. Mind very busy." Then, correlate this with your morning audit. Do nights with "high tension/busy mind" scans lead to "poor sleep quality" ratings and "woke up stiff" notes? This correlation is powerful. It directly links your pre-sleep state to your sleep outcome, making abstract "stress" concrete and locatable in the body. Over time, the scan itself becomes the intervention, as the act of mindful observation begins to dissolve the very tension it measures.
We've touched on timing, but there is a deeper layer to measure: the strength and regularity of your sleep-wake rhythm, or its circadian amplitude. A strong rhythm promotes robust, consolidated sleep. A weak, erratic rhythm leads to fragmented sleep and daytime fog. You can measure the strength of your rhythm without a single lab test.
The Wake-Up Time Standard Deviation Test:
This sounds technical, but it's simple. Over two weeks, log your wake-up time each day (whether by alarm or naturally). At the end, calculate the variation.
The "Natural Wake-Up" Experiment:
If possible, for 3-4 days (on vacation or a quiet weekend), go to bed when you feel sleepy and wake without an alarm. Note the natural wake time. This is your body’s preferred phase. The gap between this and your socially required wake time is a precise measure of your circadian misalignment. Even being aware of this gap is a critical measurement.
Measuring Light Consistency:
Your rhythm is set by light. Therefore, the consistency of your light exposure is a proxy for rhythm strength. Audit: Do you get bright light within 30 minutes of waking every day? Do you dim lights at the same time each evening? Inconsistency in light exposure guarantees inconsistency in sleep timing and quality. Tracking your adherence to light hygiene becomes a predictive metric for sleep rhythm strength.
Understanding the difference between sleep debt (the accumulated deficit from insufficient sleep) and sleep drive (the increasing biological pressure to sleep) is crucial. You can measure both using simple observational experiments.
Measuring Sleep Drive (Homeostatic Sleep Pressure):
Sleep drive builds from the moment you wake up. You can estimate its strength by observing:
Estimating Sleep Debt:
Sleep debt is trickier but can be approximated through a sleep extension experiment.
By understanding this balance sheet, you make smarter decisions. A high sleep drive in the afternoon tells you a short nap might be beneficial. A large sleep debt tells you the priority is more sleep, not optimizing sleep stages with a fancy device.
In the quest for efficiency and duration, we often ignore the most human metric: the emotional and qualitative experience of sleep. Did it feel peaceful? Restorative? Or was it haunted by anxiety dreams? This subjective dimension is a valid and critical measure of health.
The Dream Journal as a Qualitative Gauge:
Keeping a brief dream log isn't about interpretation; it's about pattern recognition in your subconscious landscape.
The "Feeling Upon Waking" Deep Dive:
Move beyond a number score. Use descriptive language in your morning audit. "I woke up feeling resentful that the night was over" versus "I woke up feeling gentle anticipation for the day." The emotional texture of wakefulness is a direct reflection of your sleep's restorative quality for your psyche, not just your body. Tracking this emotional quality can reveal the impact of life stressors or the benefits of therapy or meditation in a way raw sleep duration cannot.
Measuring Sleep-Related Anxiety:
A crucial metric is: How much do you worry about sleep? Log any pre-sleep thoughts like "I hope I fall asleep tonight" or "If I don't sleep 8 hours, tomorrow will be ruined." The frequency and intensity of these thoughts are a measure of sleep performance anxiety, which is itself a primary cause of insomnia. Success in your sleep journey is not just better numbers, but a reduction in this anxiety—replacing dread with trust in your body's ability to rest.
Even with perfect habits, you will have bad nights. The measure of your sleep health is not the absence of bad nights, but how you contextualize and recover from them. This requires shifting your measurement lens from a single night to a rolling average and observing your resilience.
The 3-Night Rolling Average:
One night of poor sleep is a blip. Three consecutive poor nights suggest a trend. Instead of panicking day-to-day, track a simple rolling average of your sleep quality score. Calculate the average of the last three nights. This smooths out the noise and reveals the true signal. Is your 3-night average stable, or is it in decline? This is a more meaningful metric than any single data point.
The "Rebound" Metric:
After a poor night, measure this: How does your body respond the next night? Do you fall asleep faster (showing a healthy sleep drive rebound)? Or does the anxiety from the bad night cause another night of long latency (showing poor sleep resilience)? A healthy system will naturally generate higher sleep pressure to correct a deficit. Observing whether or not this happens is a key measure of your system's robustness.
Identifying Triggers vs. Noise:
When a bad night occurs, cross-reference it with your diary. Was there an obvious trigger (e.g., late espresso, heated argument, poor room temp)? If yes, log it as a trigger-induced disruption—a learning opportunity. If no clear trigger exists, log it as biological noise—your system's normal variation. This distinction prevents you from over-engineering your life in response to normal fluctuations. It teaches you to respond to patterns, not outliers. For support in navigating these normal fluctuations and setbacks, our FAQ section offers grounded advice.
You now have data across nearly twenty dimensions, from physiological signals to emotional quality. The final synthesis is to translate this from a diagnostic report into a living, breathing Personal Sleep Protocol—your owner's manual for rest.
Protocol Sections:
The Iterative Review Schedule: Your protocol is not set in stone. Schedule a quarterly "Sleep Protocol Review." Over one week, return to focused tracking. Has your baseline changed (e.g., due to age, season, new job)? Does your protocol need updating? This scheduled review turns sleep health into a lifelong practice of gentle optimization, not a frantic fix.
This protocol is your empowerment document. It means you are never starting from scratch, never at the mercy of the latest sleep fad. You have a system, built on your own data. When friends ask for advice, you can share your process, not just a product recommendation. When a doctor asks about your sleep, you can provide a concise history. This is the ultimate goal of non-device measurement: to become the acknowledged expert on your own rest, equipped with self-knowledge that no product can provide but that can make any product you choose to use infinitely more valuable. For those inspired to document their own journey or share their findings, our blog is a platform for community learning.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/