The Neurobiology of Emotional Regulation: How Your Brain Manages Feelings
Balance means feeling and processing emotions; suppression means pushing them away, which leads to later dysregulation and health issues.
Balance means feeling and processing emotions; suppression means pushing them away, which leads to later dysregulation and health issues.
In the silent theater of your mind, a breathtaking drama unfolds every second of your life. A surge of frustration in traffic, the warm glow of a friend’s compliment, the cold grip of anxiety before a big meeting—these are not mere fleeting experiences. They are the output of an immensely complex biological system, a symphony of electrical impulses and chemical messengers that constitutes the very essence of your human experience. This is the world of emotional regulation, the brain’s sophisticated process of generating, perceiving, and modulating feelings.
For centuries, emotions were the domain of poets and philosophers. Today, they are mapped in the intricate circuitry of the human brain, a frontier where neuroscience is rewriting our understanding of mental health, resilience, and well-being. We are no longer passive passengers to our emotional tides. By understanding the neurobiology of how our brain manages feelings—from the primal alarm of the amygdala to the reasoned control of the prefrontal cortex—we gain a powerful manual for our own inner workings.
This knowledge is no longer confined to research labs. With the advent of personal biometric technology, like the advanced smart rings from innovators such as Oxyzen, we can now observe the physiological signatures of our emotions—heart rate variability (HRV), skin temperature, and sleep patterns—in real-time. This creates an unprecedented feedback loop between subjective feeling and objective data, empowering us to move from simply experiencing emotions to consciously engaging with our brain's regulatory machinery. Understanding this science is the first, crucial step toward mastering it, transforming our relationship with stress, enhancing our focus, and building unshakable emotional resilience. For a deeper dive into how technology bridges this gap between biology and awareness, you can explore our blog for more wellness insights.
To understand emotional regulation, we must first appreciate the brain's emotional architecture—a layered system built over millions of years of evolution. Our most fundamental emotional responses are orchestrated by deep, subcortical structures often called the "limbic system," a term coined in the 1950s that, while somewhat simplified, usefully describes a network of interrelated regions.
At the heart of this network sits the amygdala, two almond-shaped clusters of neurons that act as the brain’s emotional sentinel. Its primary, evolutionarily ancient job is threat detection. Before your conscious mind has even registered a blur in your peripheral vision, your amygdala has already assessed it, triggered a cascade of stress hormones, and prepared your body to fight, flee, or freeze. This is the essence of the fear response, a lightning-fast system that kept our ancestors alive.
But the emotional brain is more than just an alarm. The hippocampus, a seahorse-shaped structure, works intimately with the amygdala. It’s the brain’s librarian, contextualizing emotional memories. While the amygdala shouts "Danger!," the hippocampus provides the file: "This is similar to that time in a safe situation, let’s double-check." Right next door, the hypothalamus serves as the command center for the body, translating emotional signals from the amygdala into physical reactions: a racing heart, sweaty palms, or a surge of adrenaline. It’s the crucial link between feeling and physiology.
This ancient survival kit, however, now operates in a world of existential deadlines, social media comparisons, and information overload. The amygdala cannot distinguish between a physical threat (a predator) and a psychosocial one (an angry email). It triggers the same physiological stress response. This mismatch between our evolutionary hardware and our modern environment is at the root of much chronic stress and dysregulated emotion. The good news is that evolution also equipped us with a remarkable moderator: the prefrontal cortex. Our journey into emotional regulation is, in many ways, the story of how this newer brain region dialogues with, and attempts to govern, these ancient emotional centers. To see how modern tools are designed to help with this modern challenge, learn more about Oxyzen's approach.
If the limbic system is the powerful, instinctive orchestra of emotion, the prefrontal cortex (PFC) is the conductor. Located directly behind your forehead, this region is the most evolved part of the human brain, responsible for executive functions: planning, decision-making, impulse control, and, crucially, the cognitive regulation of emotion.
The PFC doesn't eliminate feelings; it interprets, evaluates, and moderates them. It allows you to feel the surge of anger from a colleague's remark but choose a measured response instead of a shouted insult. It enables you to feel the pull of anxiety before a presentation but use focused breathing to steady yourself. This process is called top-down regulation, where higher-order cognitive processes exert control over lower-order emotional reactions.
Several key subregions of the PFC play specialized roles:
The communication between the amygdala and the PFC is a two-way street, a constant dialogue of brain regions vying for influence. When you successfully regulate an emotion, neuroimaging studies show increased activity in the PFC and decreased activity in the amygdala. The conductor has successfully quieted the overzealous brass section. However, under conditions of extreme stress, fatigue, or intoxication, the connection can break down. The amygdala hijacks the system, and the PFC's influence diminishes, leading to reactive, impulsive behavior. Strengthening this neural pathway is the cornerstone of building emotional resilience. Many users of biometric tracking note that observing their stress responses via data, like that provided by a smart ring, helps engage this very prefrontal circuitry, turning an automatic reaction into a conscious observation. You can read real customer reviews on how this plays out in daily life.

The conversation between brain regions is not carried by wires alone. It is spoken in a rich chemical language of neurotransmitters. These molecules are the messengers that leap across the tiny gaps between neurons (synapses), exciting or inhibiting electrical signals. Our emotional tone is profoundly shaped by the balance and flow of these key chemicals.
Dopamine is often mislabeled as the "pleasure chemical." More accurately, it is the molecule of motivation, reward prediction, and "wanting." It surges not when you receive a reward, but in anticipation of it, driving you to pursue goals. Dysregulation in dopamine pathways is linked to addiction, but also to anhedonia—the inability to feel pleasure—seen in depression.
Serotonin is the great stabilizer. It modulates mood, appetite, sleep, and a pervasive sense of well-being and contentment. Many antidepressant medications (SSRIs) work by increasing the availability of serotonin in the synaptic cleft. Optimal serotonin function is associated with emotional resilience and the ability to bounce back from negative events.
GABA (Gamma-Aminobutyric Acid) is the brain's primary inhibitory neurotransmitter. It's the central nervous system's brake pedal. By calming neuronal excitability, GABA reduces anxiety, stress, and fear. Anti-anxiety medications like benzodiazepines work by enhancing GABA's effects. Activities like meditation and deep breathing are believed to naturally boost GABA activity.
Norepinephrine (also called noradrenaline) is the alertness and arousal molecule. It is central to the body's stress response, increasing heart rate, blood pressure, and vigilance. In balance, it supports focus and energy. In excess, it fuels anxiety, panic, and hypervigilance.
Glutamate is the brain's primary excitatory neurotransmitter, the gas pedal. It's essential for learning, memory, and neural plasticity. However, excessive glutamate release is neurotoxic and implicated in the neural "storms" associated with severe stress and trauma.
Emotional regulation, at a chemical level, involves maintaining a dynamic equilibrium within this symphony of neurotransmitters. Lifestyle factors—sleep, nutrition, exercise, sunlight—directly influence their production and balance. This is why tracking biometrics like sleep patterns and resting heart rate can offer indirect clues about your neurochemical state, a principle central to the design of comprehensive wellness wearables. For those curious about the science behind these measurements, our FAQ section offers detailed explanations.
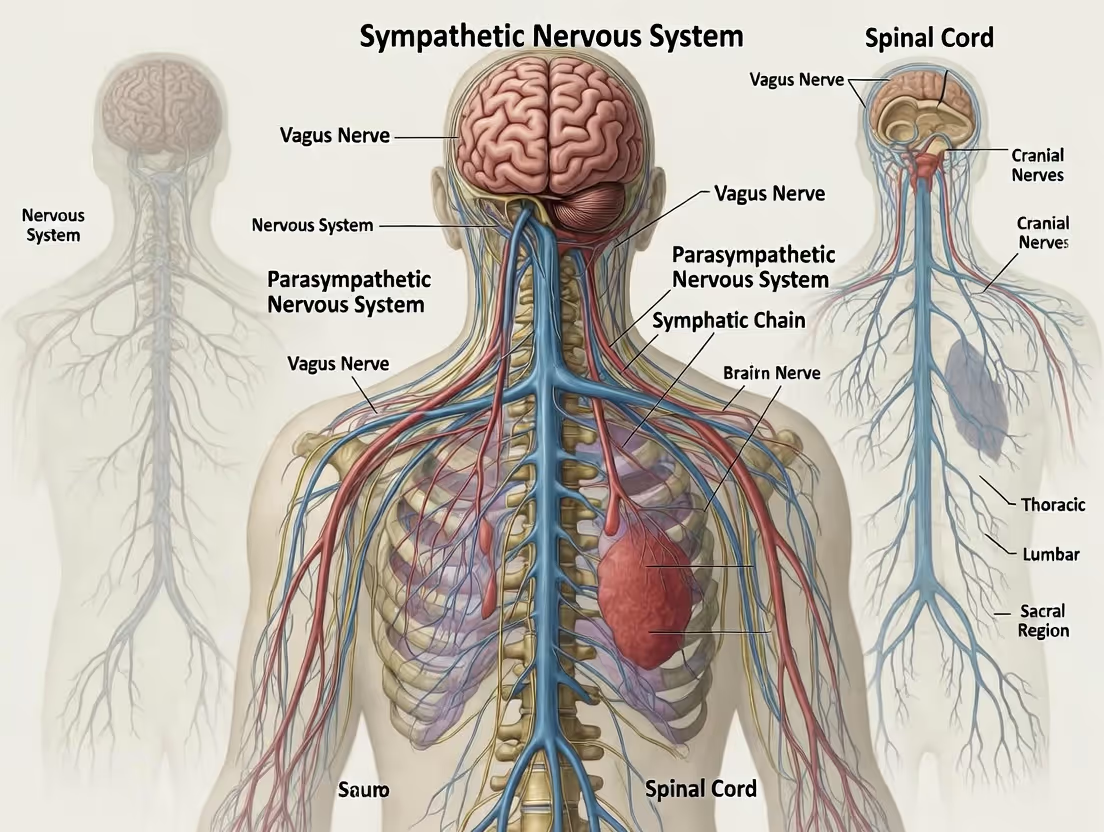
Every emotion you feel has an immediate physical echo. That knot in your stomach during fear, the warmth in your chest with love, the tense shoulders of stress—these are not metaphors. They are the work of the autonomic nervous system (ANS), the involuntary control system for your organs, glands, and blood vessels.
The ANS has two primary branches that act in a delicate, dynamic balance, much like a seesaw:
The Sympathetic Nervous System (SNS) is your "fight-or-flight" system. Activated by the amygdala and hypothalamus in response to perceived threat or challenge, it:
The Parasympathetic Nervous System (PNS) is your "rest-and-digest" system. Orchestrated largely by the vagus nerve, it promotes:
Emotional dysregulation is often reflected in an ANS that is stuck in a SNS-dominant state—a state of chronic high alert. The key to physiological and emotional regulation lies not in suppressing the SNS, but in strengthening the "braking" power of the PNS, specifically through vagal tone.
Heart Rate Variability (HRV) has emerged as a critical, non-invasive window into this balance. HRV is the subtle variation in time between each heartbeat. A high HRV indicates a healthy, responsive ANS that can swiftly adapt to changing demands—a sign of good vagal tone and emotional resilience. A low, rigid HRV suggests a system stuck in a stressed or fatigued state and is a known risk factor for anxiety and cardiovascular issues. Modern wellness technology, including the advanced sensors in devices like the Oxyzen ring, places HRV tracking at the forefront, giving users a direct, quantitative readout of their autonomic nervous system's state and their capacity for emotional regulation.

Perhaps the most revolutionary discovery in modern neuroscience is that of neuroplasticity—the brain's lifelong ability to reorganize itself by forming new neural connections. The old adage of the brain being "hardwired" after childhood is definitively false. Your emotional brain is not a fixed circuit board; it is a living, adaptable garden. The pathways you use most become stronger and more efficient; those you neglect gradually weaken. This is summed up in the phrase "neurons that fire together, wire together."
This principle is the biological basis for both the problem and the solution in emotional regulation. Chronic anxiety strengthens the amygdala's fear pathways and weakens the PFC's control pathways. Conversely, consistently practicing a calming technique like mindfulness physically thickens the prefrontal cortex and shrinks the amygdala's reactivity.
The primary mechanism behind this change is the strengthening of synapses through Long-Term Potentiation (LTP). When two neurons are activated simultaneously repeatedly, the connection between them is chemically and structurally reinforced, making future communication easier. This is how habits, both cognitive and emotional, are etched into the brain's architecture.
Myelination is another key process. Frequently used neural pathways become insulated with a fatty substance called myelin, which speeds up electrical transmission. A well-myelinated pathway is like a neural superhighway. This is why practiced emotional regulation strategies become faster and more automatic over time—they literally become a more efficient physical part of your brain.
This science transforms emotional regulation from a vague concept of "willpower" into a tangible, physiological training regimen. Every time you consciously pause before reacting, every time you reframe a negative thought, every time you engage in deep breathing to calm your physiology, you are not just "calming down." You are performing targeted neurosurgery on your own brain, sculpting the very structures that will determine your future emotional life. Understanding this empowers a proactive approach to mental fitness, a journey that many begin with the objective feedback from a wellness tracker. Discover more about the vision behind creating technology to support this journey.
To understand emotional dysregulation, we must examine the body's central stress axis in detail. The Hypothalamic-Pituitary-Adrenal (HPA) axis is a neuroendocrine cascade that represents the slow-burning counterpart to the amygdala's quick SNS trigger.
Here’s how it works:
Cortisol's job is to mobilize energy (increasing blood sugar), suppress non-essential functions (like digestion and reproduction), and modulate the immune system. In a short-term, acute stress scenario—like escaping danger—this is life-saving. The problem arises when the stressor is chronic: a toxic job, financial worry, or relational conflict.
Chronic HPA axis activation leads to:
This creates a vicious cycle: chronic stress impairs the PFC and hippocampus, weakening the brain's ability to regulate the stress response, which in turn leads to more stress. Breaking this cycle requires interventions that target both the neurobiology (through techniques that strengthen the PFC) and the physiology (by directly calming the HPA axis and SNS). Tracking metrics like nighttime HRV and sleep quality on a device like the Oxyzen ring can provide early warnings of a dysregulated stress system, allowing for intervention before burnout sets in.
Where do feelings feel like they happen? We locate emotions in the body: a "heartache," "gut feeling," or "lump in the throat." This is not just poetic language. It is the perception of interoception—your brain's sense of the internal state of your body.
Interoceptive signals—heartbeat, breath, stomach tension, muscle tone, temperature—are constantly relayed to the brain via neural pathways, most notably the vagus nerve. These signals converge in a brain region called the insula, which acts as the brain's interoceptive cortex. The insula creates a dynamic "map" of bodily sensation, which is then integrated with emotional and cognitive information in the anterior cingulate cortex and prefrontal regions.
This process is fundamental to emotional experience. Renowned neuroscientist Antonio Damasio's Somatic Marker Hypothesis posits that emotions are, at their core, changes in bodily state. When you see an angry face, your amygdala triggers a subtle increase in heart rate and muscle tension. Your insula reads this bodily change, and your brain interprets this interoceptive signal as the feeling of "being threatened" or "anxious."
Therefore, interoceptive awareness—the ability to accurately perceive these subtle internal cues—is the bedrock of emotional intelligence. Poor interoception is linked to alexithymia (difficulty identifying and describing emotions) and many psychiatric disorders. Conversely, high interoceptive accuracy is associated with better emotional regulation and resilience.
Training interoception is a primary goal of mindfulness, yoga, and biofeedback. By learning to feel your heartbeat, notice the quality of your breath, or sense tension in your shoulders, you strengthen the insula's resolution and your brain's ability to process emotional states with clarity and granularity. This turns vague, overwhelming feelings into identifiable, manageable sensations. Wearable technology that provides real-time physiological data acts as an external interoceptive aid, training your internal awareness by giving you an external, objective mirror to your body's state.
Human beings are fundamentally social creatures, and our emotional regulation systems did not evolve in isolation. They are designed to be calibrated and co-regulated through relationships. This is the domain of the social brain, a network involving the PFC, amygdala, insula, and specialized regions like the temporoparietal junction.
Mirror neurons, discovered in the premotor cortex, are thought to play a role in empathy by firing both when we perform an action and when we see someone else perform it. This creates a neural basis for understanding others' intentions and emotions, forming a bridge between self and other.
But regulation goes deeper than understanding. Co-regulation is the process by which one person's nervous system influences another's to achieve a stable state. A calm, attuned parent can soothe a distressed infant's ANS through touch, voice, and heartbeat—a process that physically shapes the infant's developing stress response systems. This dynamic continues into adulthood. A supportive conversation with a friend, a hug from a partner, or even the presence of a calm colleague can downregulate our own amygdala and HPA axis activity.
Conversely, social threat—rejection, exclusion, conflict—is one of the most potent activators of the brain's pain and stress circuits. The dorsal anterior cingulate cortex (dACC), involved in physical pain, also lights up during experiences of social pain.
Our social connections literally wire our capacity for self-regulation. Secure attachment in childhood builds a robust PFC and a resilient HPA axis. Toxic or absent relationships can do the opposite. The good news is that through reparative, healthy relationships and therapeutic alliances, this neural wiring can be revised in adulthood. The sense of connection and support fostered by a community, even one focused on shared wellness goals, can itself be a regulatory tool. Sharing and comparing wellness journey data in a supportive environment, as some users do through platforms connected to their devices, taps into this powerful social dimension of regulation. Discover the community and mission behind our approach to wellness.
Not all emotional experiences are created equal. Some people experience emotions in broad, sweeping strokes: "I feel bad." Others possess a rich, nuanced emotional vocabulary: "I feel a bittersweet nostalgia, edged with anticipatory anxiety." This ability to make fine-grained distinctions between emotional states is called emotional granularity, and it is a superpower for regulation.
Neuroscientist Lisa Feldman Barrett's Theory of Constructed Emotion argues that emotions are not pre-wired, universal states that are simply triggered. Instead, the brain constructs an emotion in the moment, using past experiences (conceptual knowledge) to make meaning of incoming sensory and interoceptive data. In this view, the concept you have for "anxiety" versus "excitement" (both high-arousal, uncertain states) guides how your brain organizes the physiological signals.
Higher emotional granularity is linked to:
The neural mechanism involves a tight coupling between the language centers of the brain (like the ventrolateral PFC) and the interoceptive/limbic regions. Putting feelings into words—a process called affect labeling—has been shown in fMRI studies to dampen amygdala activity. As the old psychotherapy adage goes, "Name it to tame it." This isn't just a metaphor; it’s a neurological intervention. Cultivating a richer emotional vocabulary through reflection, journaling, or therapy physically changes how your brain constructs and manages emotional experience. Integrating this practice with physiological awareness, such as noting what "frustration" feels like in your body and how it appears on your HRV graph, creates a powerful feedback loop for mastering your internal world.
Armed with the neurobiological map, we can now explore practical, evidence-based techniques that directly target the circuits and systems we've discussed. These are not quick fixes but training exercises for your brain.
1. Cognitive Reappraisal (Target: Prefrontal Cortex > Amygdala): This is the quintessential top-down strategy. It involves consciously reinterpreting the meaning of an emotional stimulus to alter its emotional impact. Example: Interpreting a racing heart before public speaking as "my body is energizing me to perform" rather than "I'm going to fail." This cognitive shift increases dlPFC and vmPFC activity while reducing amygdala activation. It’s a skill that strengthens with practice, literally building the neural highways for resilience.
2. Mindful Awareness (Target: Insula, Prefrontal Cortex, Amygdala): Mindfulness is the non-judgmental awareness of present-moment experience. Unlike reappraisal, it doesn't try to change the emotion. It involves stepping back and observing feelings and sensations as transient events in the mind and body. This "decentering" reduces identification with the emotion. Neuroimaging shows mindfulness practice increases gray matter density in the PFC and insula (improving regulation and interoception) and decreases amygdala volume. Simply noting, "There is tension in my chest," creates the space between stimulus and reaction where choice lives.
3. Physiological Sighing & Breathwork (Target: Autonomic Nervous System, Amygdala): Breathing is the only autonomic function we can easily voluntarily control, making it a direct lever on the ANS. The physiological sigh—a double inhale through the nose followed by a long exhale—is a potent, fast-acting tool discovered by Stanford researchers to boost oxygenation and rapidly reduce stress. It directly stimulates the PNS via the vagus nerve. Consistent breathwork practice increases HRV and improves the brain's ability to inhibit the startle response, a direct measure of amygdala regulation.
4. Regular Aerobic Exercise (Target: Hippocampus, Neurotransmitters, HPA Axis): Exercise is a potent neuroplasticity booster. It increases the production of Brain-Derived Neurotrophic Factor (BDNF), a "fertilizer" for the brain that promotes the growth of new neurons in the hippocampus and strengthens synaptic connections. It also naturally regulates serotonin, norepinephrine, and dopamine, and helps normalize HPA axis reactivity to stress. The benefits for emotional regulation are both immediate (through endorphin release) and long-term (through structural brain changes).
These practices represent the first critical toolkit, derived directly from our understanding of the emotional brain. In the next portion of our exploration, we will delve into the role of sleep, nutrition, and modern technology in creating a holistic ecosystem for emotional mastery, building upon this unshakable neurobiological foundation. To continue your learning on integrating these principles with daily life, our blog offers a wealth of related resources.
If emotional regulation is a daily performance, then sleep is the essential, non-negotiable dress rehearsal. The brain does not simply shut down during sleep; it engages in a meticulously orchestrated series of activities that are fundamental to emotional homeostasis. To neglect sleep is to sabotage the very neural machinery you rely on to manage your feelings.
The architecture of sleep is a cyclical journey through distinct stages: light sleep (N1, N2), deep slow-wave sleep (N3), and Rapid Eye Movement (REM) sleep. Each stage plays a unique role in emotional processing and regulation.
Slow-Wave Sleep (SWS): The Brain's Emotional Janitor
During deep, slow-wave sleep, the brain initiates a critical cleansing process. The day’s metabolic waste products, including beta-amyloid and other toxins, are flushed out via the glymphatic system. More pertinent to emotion, this stage is crucial for the consolidation of declarative memories (facts and events) in the hippocampus. But it also plays a role in "detoxifying" emotional memories.
Research suggests that during SWS, the neurochemical milieu shifts. Levels of stress-related neuromodulators like norepinephrine drop to their lowest point. In this quiet, low-norepinephrine state, the brain can reactivate emotional memories from the hippocampus and reprocess them in a safer, less charged context. It’s as if the memory is played back without the original, intense emotional soundtrack, aiding in integration and reducing its future disruptive power. Chronic sleep deprivation, which preferentially robs us of deep sleep, leaves this janitorial work undone, allowing emotional residue to accumulate.
REM Sleep: The Overnight Therapy Session
REM sleep, characterized by vivid dreaming, paralyzed muscles, and brain activity resembling wakefulness, is where emotional processing takes center stage. The amygdala and hippocampus are highly active during REM, while the prefrontal cortex is relatively offline. This unique neurochemical cocktail—high activity in emotional centers with low PFC control and low norepinephrine—allows the brain to associate and integrate memories, stripping them of their raw emotional intensity.
Matthew Walker, a leading sleep neuroscientist, posits that REM sleep functions as "overnight therapy." It allows us to process difficult experiences in a neurobiologically safe environment, where we can make novel connections between memories without the high-stress chemistry of the waking state. Deprivation of REM sleep, therefore, is linked to heightened emotional reactivity, difficulty modulating fear responses, and increased negativity bias—the tendency to perceive and remember negative stimuli more strongly.
Sleep Deprivation: A Perfect Storm for Dysregulation
A single night of poor sleep creates a neurobiological scenario primed for emotional volatility:
The result is a brain primed for irritability, anxiety, and poor impulse control. Prioritizing sleep is not a luxury; it is the most fundamental neurobiological intervention for emotional health. Tracking sleep stages and consistency with a wearable device provides invaluable data, moving sleep from a subjective feeling of "I slept okay" to an objective metric of your brain’s readiness to regulate. Seeing the direct correlation between a night of poor deep sleep and the next day’s emotional fragility is a powerful motivator for change. For a deeper look at the metrics that matter, our FAQ covers common questions about sleep tracking.
The idea that emotions are felt in the gut is more than a folk saying; it is a hardwired biological reality. The gut-brain axis is a complex, bidirectional communication network linking the emotional and cognitive centers of the brain with the peripheral functions of the digestive system. This dialogue occurs via neural pathways (primarily the vagus nerve), the immune system, and, most fascinatingly, through the metabolic activity of our gut microbiota.
The Enteric Nervous System (ENS): Your Gut's Independent Mind
Lining your gastrointestinal tract is a vast, intricate network of over 100 million neurons—the enteric nervous system. Often called the "second brain," the ENS can operate independently, controlling digestion, local blood flow, and gut motility. It constantly communicates with the central nervous system (CNS) via the vagus nerve, sending signals that profoundly influence mood and cognition. Over 90% of the vagus nerve's fibers carry information from the gut to the brain, not the other way around.
Microbiota: The Tiny Chemists of Emotion
Residing within your gut is a universe of trillions of bacteria, viruses, and fungi—your gut microbiome. These microbes are not passive residents; they are active chemists. They produce a staggering array of neuroactive compounds, including:
Dysbiosis—an imbalance in the gut microbiome—has been correlated with increased anxiety, depression, and stress reactivity in both animal and human studies. Inflammation triggered by a "leaky gut" (increased intestinal permeability) can lead to systemic inflammation, which is a known driver of neuroinflammation and mood disorders.
Dietary Levers for Emotional Regulation
This science empowers dietary choices as direct interventions for brain health:
By nurturing a diverse, healthy gut microbiome, you are essentially farming the internal producers of your own neurochemicals. The gut-brain axis underscores that emotional regulation is a whole-body process. Feelings of anxiety or low mood can sometimes be a signal not just from the mind, but from the microbiome. Monitoring physiological stress markers alongside dietary logs can reveal powerful, personalized connections between what you eat and how you feel, a synergy at the heart of modern wellness technology. Learn more about the holistic science that informs our product development.
For millennia, the only feedback loop for our internal state was subjective feeling—the vague sense of being "stressed" or "calm." Today, wearable technology like advanced smart rings provides an objective, real-time mirror to our autonomic nervous system, transforming emotional regulation from an abstract art into a trainable science.
Heart Rate Variability (HRV): The North Star Metric
As introduced earlier, HRV is the most significant single biometric for assessing autonomic balance and regulatory capacity. It is not your heart rate, but the variation in the milliseconds between beats. A higher, more variable HRV indicates a robust, responsive ANS—a system that can efficiently ramp up the sympathetic response when needed and powerfully apply the parasympathetic brake to recover. It is a proven biomarker of resilience, stress tolerance, and even emotional flexibility.
A low HRV indicates a rigid, stressed system stuck in "fight-or-flight" or a fatigued state. By tracking HRV trends—especially nighttime HRV (which is less influenced by momentary activity and reflects underlying recovery)—you gain an unfiltered view of your nervous system's baseline health. Seeing a dip in your weekly average HRV can be an early warning to prioritize sleep, manage workload, or engage in restorative practices before burnout or illness manifests.
Beyond HRV: A Symphony of Signals
Modern sensors integrate multiple data streams to create a richer picture:
The Power of the Feedback Loop
This is where passive tracking becomes active training. The process follows a clear neurobehavioral model:
This technology acts as an external prefrontal cortex—a source of objective data that helps override our often flawed subjective perceptions and excuses. It makes the invisible visible. For anyone on a journey to master their emotional landscape, this feedback is invaluable. You can discover how Oxyzen implements this precise feedback philosophy.
Your brain’s emotional regulation capacity is not static throughout the day. It ebbs and flows in a predictable rhythm governed by your circadian system—the internal, roughly 24-hour master clock located in the suprachiasmatic nucleus (SCN) of the hypothalamus. This clock regulates the daily cycles of hormone release, body temperature, sleep-wake states, and, critically, emotional reactivity.
The Cortisol Curve: A Daily Stress Hormone Wave
A healthy circadian rhythm produces a specific cortisol profile:
Disruption to this curve—a blunted morning spike, elevated evening levels—is a hallmark of chronic stress, burnout, and depression. It directly impairs the HPA axis's ability to respond appropriately to new stressors and recover efficiently.
The Amygdala's Daily Schedule
Research shows that amygdala reactivity to negative stimuli follows a diurnal pattern, often tracking inversely with PFC control. Emotional reactivity tends to be higher in the late afternoon and evening ("the witching hour") when circadian-driven alertness wanes and prefrontal resources may be depleted from a day's cognitive labor. This is why conflicts often flare in the evening and why poor sleep the night before sets the stage for a more emotionally volatile next day.
Circadian Misalignment: The Jet Lag of Modern Life
Our modern environment is rife with circadian disruptors:
Chronic misalignment is linked not only to poor sleep but directly to mood disorders, increased impulsivity, and weakened emotional control. Aligning with your circadian rhythm is a powerful form of emotional regulation. This means consistent sleep/wake times, morning light exposure, and mindful timing of food, exercise, and even demanding cognitive work.
Technology for Circadian Alignment
Wearable devices are exceptional tools for circadian insight. By tracking 24-hour heart rate and temperature rhythms, they can visualize your body's unique internal timing. You might discover your natural "wind-down" phase begins earlier than you thought, or that your body temperature minimum (a circadian marker) occurs at a specific time, guiding optimal sleep scheduling. This data moves circadian health from a generic prescription to a personalized practice, a core tenet of sophisticated wellness platforms. For real-world examples of how this data transforms habits, browse user testimonials on their experiences.
For decades, psychiatry and immunology were separate domains. We now understand they are intimately linked. Inflammation—the body's innate immune response to injury or pathogen—when chronic, can become a significant disruptor of emotional regulation and a direct contributor to mood disorders.
From Peripheral Inflammation to "Sickness Behavior"
When the immune system is activated, immune cells release signaling proteins called pro-inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α). These cytokines communicate with the brain via several pathways: through leaky regions in the blood-brain barrier, by binding to vagal nerve receptors, and via active transport. Once in the brain, they trigger microglia (the brain's immune cells) to produce local inflammatory signals.
This neuroinflammatory state induces "sickness behavior": fatigue, social withdrawal, anhedonia (loss of pleasure), and heightened anxiety. These are adaptive, energy-conserving responses meant to help you rest and recover from illness. However, when inflammation becomes chronic due to factors like poor diet, obesity, autoimmune disease, or persistent psychosocial stress, this "sickness behavior" morphs into symptoms of depression and anxiety.
Inflammation's Direct Assault on Brain Circuits
Chronic inflammation impacts emotional regulation through several key mechanisms:
Lifestyle as an Anti-Inflammatory Intervention
The recognition of this link is empowering because many lifestyle factors that regulate inflammation are within our control:
Monitoring physiological data can reveal the shadow of inflammation. A persistently elevated resting heart rate, poor HRV recovery after stress, and disrupted sleep can all be indirect signs of a heightened inflammatory state. Addressing emotional health, therefore, increasingly requires looking at the whole-body inflammatory picture. This integrated view is central to a modern, science-backed approach to wellness. Explore our blog for more on the lifestyle-science connection.
While mindfulness encourages acceptance, cognitive reappraisal is an active, powerful strategy for changing the emotional trajectory itself. It is the mental process of reinterpreting a situation to alter its emotional impact, and it represents the pinnacle of top-down prefrontal regulation.
The Neuroscience of Reappraisal
When you successfully reappraise, functional MRI studies show a clear neural signature:
This isn't "positive thinking" or denial. It is a flexible, realistic search for alternative interpretations. There are several core reappraisal tactics:
1. Reframing the Stimulus: Changing your perception of the event itself.
2. Reframing the Response: Changing your perception of your own emotional or physiological reaction.
3. Broadening the Perspective: "Zooming out" to see the event in a larger context.
4. Normalizing and Validating: Acknowledging that your reaction is a normal human response.
The Practice of Cognitive Flexibility
Reappraisal is a skill that requires practice. It starts with cultivating metacognition—the ability to think about your own thinking. The simple act of noticing, "I'm telling myself a story that this is catastrophic," creates the space for reappraisal. Journaling is a potent training ground. Writing down the triggering event, your initial automatic thought, the emotion it generated, and then actively generating 2-3 alternative, evidence-based interpretations strengthens the neural pathways for cognitive flexibility.
When paired with physiological awareness, reappraisal becomes even more powerful. Noticing your body's stress response can be the cue to engage your PFC: "My heart is racing. My amygdala is sounding the alarm. Let me assess the actual threat level here." This integration of body and mind is where lasting emotional agility is forged. The journey to mastering these skills is supported by a community and resources dedicated to growth; you can learn more about our mission to support that journey here.
Beyond cognitive and behavioral practices, a frontier of direct neuromodulation techniques—often called "biohacks"—is emerging. These methods aim to directly influence the activity of the nervous system to promote calm, focus, and resilience. While some require professional guidance, others are becoming accessible for personal use.
Transcutaneous Vagus Nerve Stimulation (tVNS)
The vagus nerve is the primary information superhighway of the parasympathetic nervous system. tVNS involves delivering a mild, gentle electrical current to the auricular branch of the vagus nerve in the outer ear via a small, wearable device. This non-invasive stimulation is thought to send calming signals directly to the brainstem, increasing parasympathetic tone. Studies suggest tVNS can reduce perceived stress, improve HRV, and modulate mood, showing promise as an adjunct tool for anxiety and depression. It’s a direct method of "exercising" the vagus nerve to strengthen its regulatory capacity.
Heart Rate Variability Biofeedback (HRV-B)
HRV-B is a structured training protocol that uses real-time feedback of your heart rhythm (typically via a finger sensor or chest strap) to teach you to produce a specific, healthy pattern: a smooth, sine-wave-like rhythm called respiratory sinus arrhythmia. This pattern is achieved by synchronizing your breath with your heart rate—typically breathing at your unique resonance frequency (often around 5-6 breaths per minute for adults).
Practicing HRV-B for 10-20 minutes daily has robust evidence for:
It works by creating a positive feedback loop between the heart and brain (the heart-brain coherence model), where controlled breathing entrains the heart rhythm, which in turn sends stabilizing signals via the vagus nerve to the amygdala and higher brain centers.
Controlled Hypoxic Training & Breathwork Patterns
Advanced breathing techniques like the Wim Hof Method (which combines cyclic hyperventilation, breath retention, and cold exposure) or Tummo (inner fire) meditation are forms of voluntary stress inoculation. By voluntarily and safely inducing a controlled physiological stress response (changes in blood pH, oxygen, and CO2 levels), these practices may train the body and brain to become more resilient to involuntary stress. Preliminary research suggests they can reduce the inflammatory response to pathogens and influence the sympathetic nervous system and immune signaling in novel ways. Crucially, these powerful practices should be approached with caution and proper guidance.
The Integration with Passive Tracking
The power of these active biohacks is multiplied when integrated with passive biometric tracking. You can use a wearable device to measure your baseline HRV, then perform a 10-minute HRV-B session, and observe the immediate and next-day impact on your HRV and sleep data. This turns an abstract practice into a data-driven experiment, allowing you to personalize and optimize your regulation toolkit. For those seeking to understand the full potential of such integrations, our FAQ provides further technical insights.
Understanding healthy emotional regulation casts a clarifying light on what happens when these systems break down. Mood and anxiety disorders are not moral failings or simply "bad thoughts." They are, at their core, disorders of the brain's emotional regulation circuitry, often involving a combination of genetic vulnerability, neurobiological dysfunction, and environmental stress.
Major Depressive Disorder (MDD): A System in Collapse
The neurobiology of depression reflects a multi-system failure in regulation:
Generalized Anxiety Disorder (GAD): A Stuck Alarm System
Anxiety disorders often represent an overactive threat-detection system with an underpowered brake:
The Promise of Plasticity in Treatment
This circuit-based understanding is revolutionizing treatment. Cognitive Behavioral Therapy (CBT) works by directly training reappraisal and exposure, strengthening the PFC and weakening maladaptive amygdala-based fear associations. Mindfulness-Based Cognitive Therapy (MBCT) cultivates decentering and present-moment awareness, increasing insula and PFC regulation.
Even pharmacological treatments are viewed through this lens. SSRIs, over time, are believed to promote neuroplasticity—increasing BDNF and supporting the regeneration of hippocampal neurons and the strengthening of prefrontal connections—which may be more fundamental to their therapeutic effect than the simple increase of serotonin.
This perspective is profoundly destigmatizing and empowering. It frames recovery as a process of neuro-rehabilitation—using behavioral, cognitive, and sometimes pharmacological tools to retrain and rewire the brain's emotional regulation circuits. For many, the journey involves leveraging every available tool, from therapy to lifestyle to technology, to support this rehabilitation, a holistic approach we deeply believe in. You can discover more about our story and commitment to this integrated vision.
Human beings are a social species. Our survival has always depended on our ability to connect, collaborate, and belong. This evolutionary truth is etched into the very fabric of our neural architecture. The social brain network—a web of regions including the prefrontal cortex, amygdala, insula, and specialized circuits for facial recognition and theory of mind—doesn't just facilitate interaction; it is a primary regulator of our emotional state. Social connection acts as a buffer against stress, while loneliness can trigger a cascade of neural and physiological events akin to physical pain.
The Neurochemistry of Bonding
Positive social interactions trigger the release of a powerful cocktail of neurochemicals that promote bonding and calm:
When we are with safe, trusted others, our nervous systems engage in a process called coregulation. A calm, regulated person can, through their tone of voice, facial expression, and heart rhythm, help downregulate the agitated nervous system of another. This is most evident in a parent soothing an infant, but it continues throughout life. A supportive conversation with a friend literally lowers cortisol levels and reduces cardiovascular reactivity to stress.
Loneliness: A Hypervigilant Threat State
Conversely, perceived social isolation—loneliness—is processed by the brain as a critical threat to survival. The pioneering work of social neuroscientists like John Cacioppo revealed that chronic loneliness creates a distinct and damaging neural pattern:
Chronic loneliness doesn't just feel bad; it is a significant risk factor for depression, anxiety, cognitive decline, and physical health maladies on par with smoking or obesity. It represents a profound failure of the emotional regulation system’s need for secure social scaffolding.
Building Social Resilience
Strengthening the social dimension of emotional regulation involves both quality and quantity:
Our physiological data often reflects our social world. A period of social isolation or conflict can manifest as elevated resting heart rate, poor sleep, and lowered HRV. Conversely, a week filled with positive connection may show improved recovery metrics. This feedback can serve as a powerful nudge to reach out and invest in our relational health, a cornerstone of the holistic wellness approach championed by platforms like Oxyzen. For stories of how community and connection play into personal wellness journeys, you can read our user testimonials.
The adage "you are what you eat" reaches its fullest expression in the brain. Every thought, feeling, and regulatory impulse is powered by molecules derived from our diet. The emerging field of nutritional psychiatry examines how specific nutrients and dietary patterns directly influence brain structure, neurotransmitter function, inflammation, and ultimately, emotional health.
Critical Nutrients for Neurotransmitter Synthesis
The brain cannot manufacture the raw materials for its chemical messengers; it must draw them from the bloodstream.
The Gut-Brain Diet Connection
As explored earlier, the gut microbiome is a key player. A diet that supports a diverse, healthy microbiota inherently supports the brain:
The Inflammatory Culprit: The Standard Western Diet
Contrast this with the standard Western diet—high in refined sugars, processed meats, and industrial seed oils, and low in fiber and phytonutrients. This pattern:
Studies, such as the SMILES trial, have demonstrated that a Mediterranean-style diet—rich in vegetables, fruits, whole grains, olive oil, and fish—can be as effective as psychotherapy or medication for some individuals with moderate-to-severe depression.
Personalizing Nutrition Through Data
The link between food and mood is highly individual, influenced by genetics, microbiome, and food sensitivities. Here, biometric tracking becomes a powerful discovery tool. By logging food intake and correlating it with physiological data (energy, HRV, sleep quality, resting heart rate), you can begin to identify personal triggers (e.g., a blood sugar crash from refined carbs leading to irritability) and supporters (e.g., a salmon dinner correlating with excellent deep sleep). This moves nutrition from generic advice to a personalized N-of-1 experiment in emotional regulation. For more resources on building a brain-healthy lifestyle, our blog offers continuing guidance.
Emotional regulation is not solely about managing negative states; it is equally about cultivating positive ones that broaden our cognitive and behavioral repertoire and build resilience. The work of psychologist Barbara Fredrickson’s "Broaden-and-Build" theory posits that positive emotions like joy, interest, contentment, and awe widen our scope of attention, cognition, and action, building durable personal resources. Engaging in play, creativity, and experiences of awe are not frivolous diversions; they are neural exercises for a flexible, resilient mind.
Play: The Brain's Training Ground for Flexibility
Play, in all its forms—from rough-and-tumble play in children to games, sports, and humor in adults—is a state of voluntary engagement in intrinsically rewarding, non-serious activity. Neurologically, play:
In adults, the loss of play is linked to rigidity, burnout, and diminished creativity. Integrating play—whether through a hobby, a sport, or simply being silly—is a potent antidote to chronic stress, reminding the brain of safety and possibility.
Creativity: A State of Flow and Cognitive Reorganization
Creative acts—writing, painting, making music, coding, gardening—often induce a flow state, characterized by complete absorption, loss of self-consciousness, and a distorted sense of time. The neuroscience of flow reveals:
Engaging in creativity is not about producing a masterpiece; it’s about the process of exploration and expression. It serves as an emotional outlet, a form of mindfulness, and a way to cognitively restructure experiences. It builds neural pathways for problem-solving and cognitive flexibility that transfer to emotional challenges.
Awe: The Emotion That Expands the Self
Awe is the feeling of encountering something vast that transcends our current understanding—a breathtaking landscape, the night sky, a profound piece of art or music, or an act of great kindness. It is a self-transcendent emotion. Studies led by Dacher Keltner show that experiences of awe:
Seeking awe is a powerful regulation strategy for anxiety and depression, which often trap the mind in a cycle of repetitive, self-focused negative thought. Awe literally changes the brain's pattern of activity, creating a sense of perspective and wonder that can dissolve stress. A simple "awe walk"—a walk where you intentionally focus on the vast or wondrous details around you—can be a powerful daily practice.
These positive states are not just the result of good regulation; they are the cause of it. They build the psychological and neural capital that allows us to weather emotional storms. Tracking how your body responds to these activities—perhaps noting a significant boost in HRV after an afternoon in nature or a deep flow state—can reinforce their importance in your wellness regimen. To understand the philosophy behind integrating all aspects of well-being, explore our company's story and vision.
While neurotransmitters are the rapid-fire messengers of the brain, hormones are the slower, broader tidal forces that shape the emotional landscape over hours, days, and years. The sex hormones—estrogen, progesterone, and testosterone—exert profound influence on neurotransmitter systems, neural plasticity, and stress reactivity, creating distinct emotional rhythms across the menstrual cycle and life stages.
Estrogen: The Neuroprotective Mood Modulator
Estrogen is far more than a reproductive hormone; it is a potent neurosteroid.
The premenstrual phase, when estrogen and progesterone drop sharply, can lead to a "withdrawal" from these neuroprotective and mood-stabilizing effects in susceptible individuals, contributing to Premenstrual Dysphoric Disorder (PMDD).
Progesterone & Allopregnanolone: The Double-Edged Sword
Progesterone’s metabolite, allopregnanolone, is a powerful positive modulator of GABA-A receptors, exerting strong anxiolytic (anti-anxiety) and sedative effects. In the luteal phase (post-ovulation), rising progesterone and allopregnanolone can promote calm. However, in some, the rapid decline of these compounds premenstrually can trigger a paradoxical increase in anxiety, irritability, and insomnia—a kind of GABAergic withdrawal.
Testosterone: Beyond Aggression to Motivation and Calm
Often stereotyped as the hormone of aggression, testosterone’s role in emotional regulation is more nuanced:
Low testosterone in men and women is associated with fatigue, low mood, irritability, and decreased stress resilience.
Lifespan Transitions: Puberty, Postpartum, and Perimenopause
These hormonal transitions are periods of heightened vulnerability for emotional dysregulation due to massive neuroendocrine shifts:
Tracking the Rhythm
For those with menstrual cycles, tracking mood and biometrics alongside cycle phases can reveal powerful personal patterns. You may discover your HRV is highest and your resting heart rate lowest in the follicular phase (as estrogen rises), or that sleep disruption is predictable in the luteal phase. This knowledge is not about resignation, but about strategic adaptation—scheduling demanding cognitive work during high-energy phases and prioritizing stress-reduction techniques during vulnerable windows. This level of personalized insight is a cornerstone of modern, data-informed wellness. For support in understanding your own unique patterns, our FAQ provides answers to common questions.
We stand at the brink of a new era in emotional regulation, where wearable biometrics are just the beginning. The frontier of neurotechnology promises tools that move beyond measuring the nervous system to actively modulating it with increasing precision. This emerging field blends neuroscience, engineering, and data science to create interfaces between the brain and external devices.
Current Wearables: The Foundational Layer
Today's advanced wearables, like the Oxyzen ring, represent the first, crucial layer: providing continuous, passive, and multi-modal physiological data (HRV, HR, temperature, activity, sleep). This creates a digital phenotype—a dynamic, objective representation of your autonomic state. The next step is sophisticated analytics and machine learning that can:
Next-Generation Biofeedback: Neurofeedback and fNIRS
Non-Invasive Brain Stimulation: tDCS & TMS
The Future: Closed-Loop Systems and Ethical Frontiers
The horizon holds the potential for closed-loop systems. Imagine a device that detects the early physiological signature of a panic attack (via HRV, respiration) and automatically delivers a subtle, calming vagus nerve stimulation to avert it. Or a system that detects prefrontal fatigue and suggests an optimal break.
With these advances come profound ethical questions about privacy, data ownership, and the very nature of emotional authenticity. The goal must always be augmentation, not replacement—using technology to enhance our innate human capacity for self-awareness and regulation, not to outsource it. The core mission remains empowerment through knowledge. To see how we are thoughtfully navigating this future, you can learn more about our mission and vision.
Understanding the neurobiology of emotional regulation provides a magnificent map. But a map is only useful if you use it to navigate. The final step is translation—integrating this knowledge into a sustainable, personalized daily practice that strengthens your brain's regulatory circuits and builds resilience from the ground up.
This is not about a rigid, hour-by-hour protocol. It is about creating a toolkit and a mindset. Think of it as building your personal "Emotional Regulation Operating System" (EROS), with daily habits as the code that runs it.
The Foundational Pillars: Non-Negotiable Maintenance
These are the basics that keep the entire system stable. Neglecting them makes all other strategies an uphill battle.
The Daily Training: Strengthening the Circuits
These are the active exercises for your prefrontal cortex and autonomic nervous system.
5. Mindfulness Anchor: A minimum of 10-20 minutes of formal mindfulness practice (focused attention, body scan) to strengthen the insula and PFC and weaken amygdala hijacking.
6. Physiological Sigh Breaks: Use the double-inhale, long-exhale breath 3-5 times, multiple times a day—especially during transitions—to rapidly reset the ANS.
7. Cognitive Check-Ins: Practice metacognition. Pause several times a day to ask: "What is my body feeling? What story am I telling myself? Is there a more helpful or accurate way to see this?" This is reappraisal in action.
8. Positive Experience Savoring: Intentionally linger on a good moment for 20-30 seconds—a delicious taste, a warm interaction, a small win. This enhances encoding in the hippocampus and builds positive neural pathways.
The Weekly Investments: Building Capital
These practices build the deeper resources for long-term resilience.
9. Social Connection: Schedule quality time with people who leave you feeling energized and safe. Prioritize face-to-face interaction.
10. Play & Creativity: Block out time for an activity that induces flow or pure, non-productive joy. This is system maintenance for cognitive flexibility.
11. Awe Exposure: Plan a weekly "awe walk" in nature, visit a museum, or stargaze. Deliberately seek experiences that make you feel small in a wonderful way.
12. Data Review & Adaptation: Once a week, review your biometric trends (HRV, sleep, activity) not with judgment, but with curiosity. What patterns do you see? What small experiment can you run next week to improve one metric?
The Role of Technology: Your Co-Pilot
Your wearable device is the co-pilot in this journey. It provides the objective feedback that counters subjective blind spots. It shows you the tangible impact of a good night's sleep, a stressful week, or a consistent meditation practice. It turns self-care from a vague concept into a data-informed science. Let it be a source of motivation and discovery, not another source of stress or perfectionism.
The path to mastering the neurobiology of emotional regulation is a lifelong journey of self-experimentation and compassion. There will be days when the amygdala wins. The goal is not perfection, but progress—a gradual strengthening of the neural pathways for peace, resilience, and wisdom. You are not at the mercy of your biology; you are its gardener. For ongoing support, resources, and community on this journey, we invite you to explore our full platform and blog.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/