Sleep Stage Optimization: Can You Control Which Stages You Get?
While you cannot directly control sleep stages, consistent sleep schedules and good hygiene promote healthy stage distribution.
While you cannot directly control sleep stages, consistent sleep schedules and good hygiene promote healthy stage distribution.
You’ve dutifully tracked your sleep for months. Every morning, you check your smart ring or wearable to see the verdict: a sleep score, total hours, and a colorful chart breaking your night into neat slices of light, deep, and REM sleep. You know deep sleep is for physical restoration and REM is for memory and mood. You see the percentages, the trends, the comparisons to “optimal” ranges. And then, the inevitable question arises, moving from passive observation to active desire: What if I could control this?
What if, instead of just hoping for a good night, you could engineer one? Could you strategically increase your deep sleep to accelerate muscle recovery after an intense workout? Could you bolster your REM sleep before a critical day of creative problem-solving or learning a new skill? The very idea sounds like science fiction—a level of biohacking reserved for elite athletes or Silicon Valley CEOs. But as sleep science evolves and personal biometric technology becomes extraordinarily sophisticated, the line between observation and optimization is starting to blur.
Welcome to the frontier of sleep stage optimization. This isn’t just about sleeping more; it’s about sleeping smarter. It’s the pursuit of qualitative sleep mastery, where understanding the unique architecture of your night becomes the blueprint for enhancing your day. For the modern wellness enthusiast armed with data from devices like the Oxyzen smart ring, this represents the next logical step. We’ve moved beyond counting steps; now we’re architecting our restorative biology.
But is true, direct control over your sleep cycles even possible? Can you consciously “order” more deep sleep like you would a latte? The short answer is nuanced. You cannot micromanage your brain’s nocturnal activity with conscious, real-time precision. However, you can create the perfect internal and external conditions that reliably bias your sleep architecture toward more of what you need. This is the art and science of sleep environment design, lifestyle chronobiology, and data-driven habit formation. It’s about stacking the deck in your favor, night after night.
In this comprehensive exploration, we will dismantle the mystery of sleep stages, examine the levers we can pull to influence them, and separate the evidence-based strategies from the pervasive myths. We’ll leverage the latest research and consider how modern tools are putting unprecedented power in our hands—or, more accurately, on our fingers. By the end, you will have a clear framework for not just tracking your sleep, but actively shaping it to support your unique health, performance, and wellness goals. Let’s begin by understanding what we’re actually trying to optimize.

To optimize something, you must first understand its fundamental structure. Sleep is not a monolithic state of unconsciousness; it’s a dynamic, cyclical journey through distinct physiological and neurological territories. Each stage serves a non-negotiable purpose, and the architecture—the proportion and sequence of these stages—is a key determinant of sleep’s restorative quality.
Modern sleep science classifies sleep into four stages, which are grouped into two overarching types: Non-Rapid Eye Movement (NREM) sleep and Rapid Eye Movement (REM) sleep. A full cycle through all stages typically lasts about 90 to 110 minutes, and a healthy adult will complete four to six of these cycles per night.
Stage 1 (N1 - Light Sleep): This is the doorway to sleep, lasting several minutes. Your body begins to relax—heartbeat, breathing, and eye movements slow, and muscles may twitch. Brain waves start to transition from the waking alpha rhythms to slower theta waves. You’re easily awakened during this phase. It usually constitutes about 5% of your total sleep.
Stage 2 (N2 - Light Sleep): This is the foundational stage of sleep, where you spend nearly 50% of your night. Your body goes into a more subdued state: body temperature drops, eye movements stop, and heart rate and breathing become regular. Brain activity slows further with specific patterns called sleep spindles (brief bursts of activity) and K-complexes (sharp waveforms) that are thought to play a role in memory consolidation and sensory processing, preventing you from being awakened by minor noises.
Stage 3 (N3 - Deep Sleep or Slow-Wave Sleep): This is the most physically restorative phase. Breathing and heart rate reach their lowest levels, muscles are fully relaxed, and brain waves slow to deep, rhythmic delta waves. It is very difficult to wake someone from deep sleep. This stage is critical for tissue repair, muscle growth, immune function strengthening, and energy restoration. Growth hormone is primarily secreted during deep sleep. Early in the night, deep sleep periods are longer, and they diminish as the night progresses. It typically makes up 15-25% of sleep in healthy young adults.
Stage 4 (REM Sleep): About 90 minutes after falling asleep, you enter REM sleep, marked by rapid eye movements behind closed eyelids. Brain activity ramps up to levels near wakefulness, breathing becomes faster and irregular, and heart rate and blood pressure increase. However, a temporary paralysis (atonia) sets in for most voluntary muscles, preventing you from acting out your dreams. REM is the primary stage for cognitive functions: memory consolidation, learning, emotional processing, and creativity. The first REM period is short, but each subsequent one lengthens, with the final REM period potentially lasting an hour. REM constitutes about 20-25% of total sleep.

The sequence of these stages is not random; it follows a predictable narrative. The first half of the night is dominated by deep N3 sleep. Your body prioritizes physical restoration. As the night progresses, REM sleep periods lengthen, and deep sleep becomes less prominent. By morning, you’re spending most of your time in Stage 2 and REM sleep. This architecture is why cutting your sleep short by two hours doesn’t just mean you lose 25% of your sleep—you disproportionately lose the large, late-night REM periods, which can significantly impact mood and cognitive sharpness.
Understanding this blueprint is the first step toward optimization. You cannot change this fundamental narrative, but you can influence the quality, depth, and proportion of the acts within it. To do that effectively, you need precise data on your personal narrative. This is where technology like the Oxyzen smart ring transcends simple tracking, offering the granular insights needed to begin a true optimization journey. By monitoring physiological signals like heart rate variability, skin temperature, and movement, it provides a detailed map of your unique sleep architecture, night after night.
If we imagine our sleep as a complex, self-running program, where is the control panel? What internal and external factors decide how much deep or REM sleep we get on any given night? The answer lies in a delicate interplay of biological drives, circadian rhythms, homeostatic pressure, and environmental cues.
The most robust scientific model for sleep regulation is the Two-Process Model, which describes how two primary systems work in concert.
Process S (Sleep-Wake Homeostasis): This is your body’s internal timer for sleep pressure. Think of it as an hourglass that starts emptying when you wake up. The longer you are awake, the more adenosine (a byproduct of cellular energy consumption) accumulates in your brain. This increasing adenosine level creates a growing pressure to sleep—this is homeostatic drive. When you sleep, you clear adenosine, resetting the timer. Deep N3 sleep is particularly sensitive to Process S. A long period of wakefulness or sleep deprivation will result in a powerful rebound effect, where the brain prioritizes deep sleep to catch up on physical restoration. This is why after an exhausting day or a night of poor sleep, you’ll often experience more intense, longer deep sleep the following night.
Process C (The Circadian Rhythm): This is your body’s internal 24-hour clock, governed by the suprachiasmatic nucleus (SCN) in the hypothalamus. It influences not just when you feel sleepy or alert, but also the type of sleep you get at different times. Your core body temperature and melatonin secretion are key circadian outputs. REM sleep is more tightly coupled to the circadian rhythm. The propensity for REM sleep is highest in the morning hours, in alignment with your body’s lowest core temperature and the natural wake-up phase of your cycle. This explains why you often have vivid dreams just before your alarm goes off.
The optimal sleep window occurs when the high sleep pressure from Process S aligns with the circadian signal for sleep onset from Process C. Misalignment (like jet lag or shift work) disrupts the normal architecture, often suppressing REM sleep and fragmenting deep sleep.
Beneath these two processes, a symphony of neurotransmitters and hormones conducts the transitions between wakefulness and the various sleep stages:
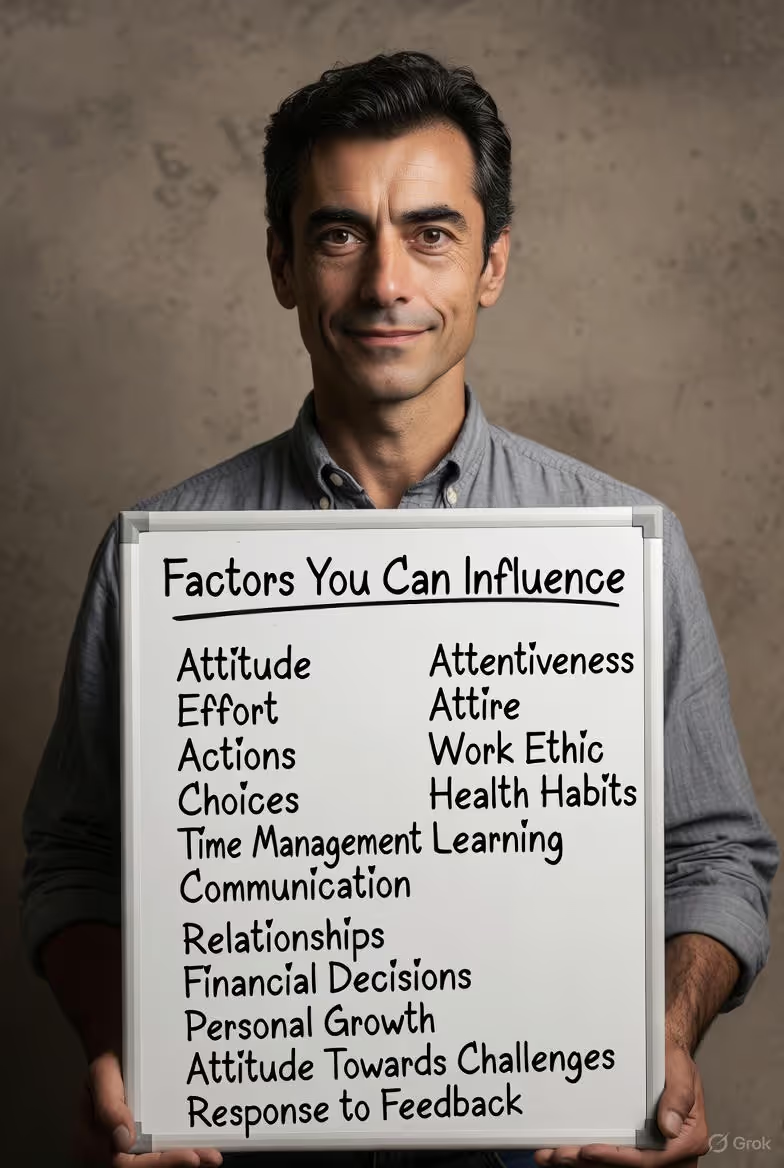
While the core machinery is automatic, its settings can be adjusted. Key modifiable factors include:
Understanding this control panel is empowering. It means that while you can’t push a button labeled “More REM,” you can adjust the master settings—light, timing, temperature, and relaxation—that the system uses to allocate resources. For a deeper dive into how technology interprets these biological signals, our blog features a detailed guide on biometric tracking.
Of all the sleep stages, deep sleep (N3) holds a particular fascination for biohackers and athletes. It’s often described as the most “restorative” stage, and for good reason. During these periods of slow-wave activity, your body executes essential physical and cerebral maintenance that is impossible to replicate during wakefulness or lighter sleep.
Deep sleep is when your body shifts into repair and rebuild mode. Several critical processes peak during this stage:
While REM gets credit for memory, deep sleep plays a foundational role in cognitive function:
When you miss deep sleep, the deficit is felt acutely:
The imperative is clear: deep sleep is a biological priority. Your brain will attempt to reclaim it after deprivation (the rebound effect), but consistently shortchanging it undermines your physical health and mental clarity. For active individuals, this stage is as important as the workout itself. As many users report in their Oxyzen testimonials, seeing their deep sleep metrics improve often correlates directly with better recovery times and higher daily energy levels.

If deep sleep is the body’s workshop, REM sleep is the mind’s theater, therapy session, and innovation lab combined. This psychologically rich stage is characterized by high brain activity, vivid dreaming, and is essential for emotional resilience, complex learning, and creative insight.
The functions of REM sleep are distinct from, but complementary to, those of deep sleep:
REM’s paradoxical nature—an active brain in a paralyzed body—serves a purpose. The muscle atonia prevents us from acting out our dreams, ensuring safety. The fluctuations in heart rate and breathing may be linked to the emotional content of dreams. The rise in brain temperature during REM is also a distinct feature of this stage.
Suppressing REM sleep, which is common with alcohol consumption and certain medications like SSRIs (which can initially suppress REM), has notable consequences:
Understanding the REM realm reframes sleep from passive rest to active mental cultivation. It’s not an escape from waking life, but an essential part of making sense of it. For professionals, students, artists, and anyone navigating complex emotional landscapes, honoring and protecting REM sleep is a strategic investment in cognitive and emotional capital. To see how consistent tracking can reveal your personal REM patterns, you can explore real user experiences with Oxyzen.
With a clear understanding of what each stage does, the tantalizing question returns: Can we consciously control this process? The internet is rife with bold claims: “Hack your deep sleep with this supplement!” or “Trigger lucid dreaming and control your REM!” It’s crucial to separate the plausible from the fantastical and ground our expectations in physiology.
Your sleep architecture is governed by the ancient, autonomic parts of your brain—the brainstem and hypothalamus. You cannot consciously decide to enter deep sleep at 1:17 a.m. or initiate a 45-minute REM period on command. The transitions are automatic, driven by the neurochemical and homeostatic systems we’ve discussed. Furthermore, each stage serves a vital purpose; the brain has its own intelligence in allocating resources based on your body’s needs. After heavy physical exertion, it will prioritize deep sleep. During periods of intense learning or emotional stress, REM may increase.
Attempting to brute-force control over one stage would likely disrupt the natural, healthy balance of the entire system. For instance, artificially increasing deep sleep through external means (if it were possible) might come at the cost of REM or light sleep, which have their own essential functions.
The realistic and powerful approach is not one of direct control, but of influence. You can’t dictate the play, but you are the stage manager, lighting director, and script consultant. You create the ideal environment and context for the brain’s natural processes to unfold optimally. This is the domain of evidence-based sleep hygiene, chronobiology, and lifestyle design.
Think of it like gardening. You cannot force a tomato plant to grow fruit. But you can ensure it has perfect soil, the right amount of water and sunlight, protection from pests, and a sturdy trellis. By optimizing these conditions, you maximize the plant’s inherent potential to produce a bountiful harvest. Similarly, by optimizing your sleep conditions—light, temperature, timing, nutrition, and stress—you maximize your brain’s inherent potential to generate healthy, abundant, and well-structured sleep.
This shift in mindset—from controller to cultivator—is liberating and effective. It moves us away from gimmicks and towards sustainable habits that work with our biology, not against it. The goal becomes sleep stage support, not sleep stage steering.
This is where precision tracking becomes invaluable. Without data, optimization is guesswork. You might feel tired, but not know if you missed deep sleep or REM. A device like the Oxyzen smart ring acts as your nightly report card, showing you the outcomes of your “gardening” efforts. Did that evening meditation correlate with a calmer heart rate and more stable sleep? Did that late-night meal fragment your deep sleep? Did a consistent 10 p.m. bedtime for a week improve your REM percentage? The data provides the feedback loop necessary for intelligent experimentation and personalization, which you can read more about in our comprehensive FAQ on sleep tracking.
Of all the environmental factors you can manipulate, light is the master conductor of your circadian rhythm, and by extension, your sleep architecture. Its influence is profound, direct, and rooted in millions of years of evolution. Getting your light exposure right is the single most effective step you can take to bias your sleep toward healthier, more balanced stages.
Light is detected by specialized photoreceptor cells in your retina called intrinsically photosensitive Retinal Ganglion Cells (ipRGCs). These cells are most sensitive to short-wavelength blue light (around 480 nanometers). When they detect blue light—especially from the bright, blue-rich sky of morning—they send a direct signal to your brain’s SCN, your master clock.
Your goal is to create a strong contrast between day and night in your light environment.
For a Strong Circadian Rhythm & Better Deep Sleep:
Consistent, correct light exposure leads to a well-timed, robust melatonin signal. This helps you fall asleep faster at the optimal time, when sleep pressure is high. Falling asleep at the right circadian time ensures your first sleep cycle, which is richest in deep sleep, begins under ideal conditions. It also protects the later, REM-rich cycles from being truncated by a misaligned wake-up time. In essence, light discipline sets the stage for the entire nightly performance to run on schedule. For more on designing your environment for optimal rest, our blog covers advanced sleep hygiene strategies.
After light, temperature is arguably the next most powerful environmental lever for sleep quality. Your body’s core temperature follows a circadian rhythm, and its deliberate drop is a non-negotiable biological signal for sleep onset and maintenance. Mastering this thermal dance is key to unlocking deeper, less fragmented sleep.
In the evening, as part of your circadian wind-down, blood vessels in your skin dilate (a process called vasodilation). This increases blood flow to your extremities, releasing core heat and causing a slight drop in your body’s internal temperature. This drop, beginning about 1-2 hours before your natural bedtime, is a critical signal to the brain that it’s time for sleep. It’s why you might feel sleepy in a cool room and why a warm bath before bed can be helpful—the rapid cooldown after the bath mimics and amplifies this natural signal.
A cool sleeping environment is essential because it supports this natural thermoregulation. A room that’s too warm prevents the necessary heat dissipation, confusing your internal signals and leading to:
Research consistently points to an ideal bedroom temperature between 60-67°F (15.5-19.5°C) for most adults. This range facilitates the core-to-shell heat transfer without making you so cold that it becomes a stressor.
The optimal temperature can be personal. This is where biometric tracking shines. The Oxyzen smart ring continuously measures your skin temperature, one of the most reliable proxies for circadian rhythm and sleep quality. By reviewing your data, you can see if a warmer-than-usual night correlated with restless sleep or reduced deep sleep. You can experiment with different thermostat settings and see the objective impact on your sleep architecture. This personalized feedback turns a general guideline (“sleep cool”) into a precise, customized protocol for you. Understanding these subtle biometrics is part of the innovative technology behind Oxyzen.
You are not just what you eat; you sleep how and when you eat. The timing, composition, and quantity of your food and drink act as powerful zeitgebers and metabolic signals that can either harmonize with or disrupt your sleep architecture. Navigating this relationship is a cornerstone of sleep stage optimization.
Eating sends a signal to your peripheral circadian clocks, particularly in organs like the liver. Consistent meal times help synchronize these clocks with your central brain clock. Erratic eating patterns, especially late at night, can send conflicting signals, causing circadian misalignment that manifests as poor sleep.
Macronutrients:
Key Micronutrients and Compounds:
By viewing your diet as a series of timed signals to your circadian system and a provider of sleep-supportive nutrients, you turn eating into a proactive sleep optimization tool. The effects of these choices are often clearly visible in your sleep stage data, providing a compelling reason to align your nutrition with your sleep goals. For personalized insights, our support team can help interpret your data.
Exercise is a potent, dual-action tool for sleep optimization. It builds homeostatic sleep pressure (Process S) and strengthens circadian rhythms (Process C). However, its effects on sleep architecture are nuanced and highly dependent on timing, type, and intensity. Used strategically, movement can be one of your most reliable levers for increasing deep sleep and stabilizing your nightly structure.
The relationship between exercise timing and sleep is a U-shaped curve, not a straight line.
This is where a smart ring becomes an essential training partner. You can conduct personal experiments:
By observing the direct impact of different exercise modalities and timings on your sleep architecture, you can create a perfectly personalized movement protocol that maximizes your recovery and sleep quality. This data-driven approach is at the heart of modern wellness, a principle we champion in everything we do at Oxyzen.
In our hyper-stimulated, always-on culture, the transition from wakefulness to sleep is not automatic. It requires a deliberate bridge—a wind-down ritual. This practice is not about luxury; it is a non-negotiable neurological protocol for shifting your nervous system from sympathetic dominance (alert, stressed) to parasympathetic dominance (calm, restorative). A consistent wind-down is arguably the most direct behavioral intervention you have to improve sleep onset, reduce nighttime awakenings, and create the stable internal environment needed for robust deep and REM sleep.
When you are stressed or mentally engaged, your brain exhibits high-frequency beta waves. Sleep requires slower alpha (relaxed wakefulness) and theta (drowsiness) waves. A wind-down ritual guides this descent. It also lowers cortisol, which opposes melatonin, and reduces “cognitive popcorn”—the intrusive thoughts that can prevent sleep onset and cause micro-awakenings.
A powerful ritual is personalized, consistent, and sensory.
1. The Digital Sunset (The #1 Priority):
As discussed, this is non-negotiable. Put phones, tablets, and laptops away. If you must read, use a dedicated e-ink reader or a physical book. The goal is to stop consuming new, stimulating information and to eliminate blue light.
2. Environmental Transition:
3. Physical Deactivation:
4. Cognitive and Emotional Deactivation:
5. The Consistency Signal:
Perform your ritual in the same order, at roughly the same time each night. This classical conditioning trains your brain to recognize these activities as precursors to sleep, triggering the release of sleep-promoting neurochemicals.
A effective wind-down doesn’t just help you fall asleep. By lowering physiological arousal (heart rate, cortisol) before bed, you create a smoother entry into the first sleep cycle. This stability is crucial for that initial, precious period of deep sleep. Furthermore, by reducing anxiety, you protect your REM sleep from being suppressed by stress hormones. In short, a calm mind and body at bedtime allow the natural sleep program to run without interference.
Tracking the efficacy of your ritual is straightforward with the right tools. Notice if implementing a consistent wind-down correlates in your data with a lower nighttime heart rate, fewer periods of restlessness, and an improved sleep score. It’s the ultimate feedback loop for mental hygiene. For inspiration and shared experiences on building better routines, our community often shares their journeys on the Oxyzen blog.
We’ve covered the lifestyle pillars of light, temperature, diet, and routine. Now we must confront the most common—and often most damaging—chemical interventions in our daily lives: caffeine, alcohol, and medications. These substances don’t just make you feel awake or sleepy; they actively hijack the neurochemical pathways governing your sleep architecture, often with consequences that last long after their primary effects wear off. Understanding this is critical for anyone serious about sleep stage optimization.
Caffeine is the world's most popular psychoactive drug, celebrated for its ability to promote alertness. Its mechanism of action is elegantly simple and profoundly disruptive to sleep.
Caffeine works by mimicking adenosine in shape, allowing it to bind to adenosine receptors in the brain. However, it doesn't activate them; it blocks them. Adenosine accumulates with wakefulness, creating "sleep pressure." By blocking the receptors, caffeine masks the feeling of tiredness. The critical issue is that adenosine continues to build up behind the blockade. When caffeine finally metabolizes (with a half-life of 5-6 hours, longer in some individuals), the pent-up adenosine floods the receptors, causing the infamous "caffeine crash." More insidiously, this blockade directly interferes with the sleep-wake homeostasis system (Process S).
Research shows that caffeine, even consumed 6 hours before bedtime:
The takeaway is stark: caffeine doesn't just keep you awake; it degrades the quality of the sleep you eventually get. For optimization, treating caffeine with precision is key.
Alcohol is the great deceiver of sleep. It is a sedative, not a sleep aid. It induces a state of unconsciousness that lacks the organized, restorative structure of natural sleep.
Alcohol's impact on sleep follows a predictable, destructive pattern:
Chronic alcohol use, even in moderate amounts near bedtime, can lead to:
For true sleep stage optimization, the ideal is to avoid alcohol within 3-4 hours of bedtime. If you do consume:
Many common prescription and over-the-counter medications have significant, yet often unappreciated, effects on sleep architecture.
Mastering your intake of these common substances is a direct, high-impact step toward reclaiming control over your sleep architecture. It requires honesty and observation, but the reward—truly restorative, well-structured sleep—is foundational to every aspect of health and performance.
Sometimes, despite perfect habits, sleep architecture remains elusive. This can be a sign of an underlying sleep disorder—a medical condition that systematically dismantles the natural sleep cycle. For the optimizer, recognizing the fingerprints of these disorders in your data is crucial, as they represent barriers no amount of behavioral hacking can fully overcome without professional intervention.
Obstructive Sleep Apnea (OSA) is characterized by repeated collapses of the upper airway during sleep, leading to breathing pauses (apneas) or reductions (hypopneas). Each event causes a micro-arousal—a brief shift to a lighter stage of sleep or near-wakefulness to restart breathing. These arousals are often so brief the sleeper has no memory of them.
Insomnia, particularly chronic insomnia, is not just "trouble sleeping." It is a state of 24-hour physiological and cognitive hyperarousal. The nervous system is stuck in a heightened state of alertness, fighting against the natural sleep process.
RLS involves an irresistible urge to move the legs, with uncomfortable sensations that worsen at rest and in the evening. PLMD involves repetitive, involuntary jerking of the legs (and sometimes arms) during sleep.
Sleep stage optimization operates within the bounds of healthy physiology. A sleep disorder is a medical malfunction. If you observe the following, it is time to consult a sleep specialist:
A professional diagnosis, often involving an in-lab or at-home sleep study, is the first step toward treatment (like CPAP for apnea, or specific medications for RLS). Effective treatment can be revolutionary, restoring the natural architecture that forms the basis for all optimization. This journey from disorder to health is a powerful one, and hearing others' experiences can be enlightening, as shared in some of our customer stories.
The connection between a stressful day and a poor night's sleep is intuitive. But the mechanistic link—how daytime psychological states physically alter your nighttime biology—is where we can intervene. Chronic stress and a dysregulated nervous system don't just make it hard to fall asleep; they actively suppress the most valuable stages of sleep, turning nights into a mere echo of the day's chaos.
Cortisol, your primary stress hormone, and melatonin operate in a delicate inverse rhythm. Cortisol should peak in the morning to help you wake up and decline throughout the day, reaching its lowest point around midnight. Melatonin should rise as cortisol falls. Chronic stress, anxiety, or rumination flattens this cortisol curve, keeping levels elevated into the evening. High evening cortisol:
Optimizing sleep stages, therefore, requires daytime stress management. This isn't just about evening meditation; it's about building all-day resilience.
1. Strategic Stress Breaks (Not Just Work Breaks):
2. Reframe Your Relationship with Stress:
Research by Dr. Alia Crum shows that viewing stress as a enhancing, rather than debilitating, can change its physiological impact. Instead of "My stress is ruining my sleep," try, "My body is energized to meet these challenges, and I will support it with excellent recovery tonight." This mindset shift can reduce the secondary anxiety about stress.
3. The Power of Physical Release:
As discussed, exercise is a potent stress-buffer. Even a 10-minute walk outside can metabolize stress hormones and reset a frazzled nervous system.
4. The Evening Audit (Part of Your Wind-Down):
The practice of journaling or a "brain dump" is effective because it externalizes circling thoughts. Writing down worries and to-dos tells the brain, "It is noted. You can let go now."
Your sleep tracker is a brilliant stress auditor. A day filled with deadlines and conflict will often show up as:
By correlating daytime events with nighttime data, you gain profound insight into your personal stress-sleep relationship. This allows you to proactively deploy your stress-management tools on challenging days, knowing your sleep architecture depends on it. For more on interpreting these biometric signals, our blog has extensive resources on HRV and recovery.
We have now explored the theory and the levers. But generic advice has limits. The final, and most powerful, step in sleep stage optimization is personalization. Your perfect sleep formula—the exact combination of light, temperature, exercise timing, and wind-down that yields your most restorative architecture—is unique. Discovering it requires moving from passive tracking to active experimentation, using biometric data as your objective guide. This is the era of the quantified self, and for sleep, it’s a game-changer.
A modern wellness wearable like the Oxyzen smart ring captures a symphony of physiological signals each night: heart rate (HR), heart rate variability (HRV), skin temperature, blood oxygen saturation (SpO2), and movement. Together, these data streams paint a detailed picture of your autonomic nervous system state and sleep structure.
Key metrics for stage optimization include:
Become a scientist of yourself. Use the isolate and test method.
*Sarah, a 35-year-old graphic designer, noticed her Oxyzen data showed consistently low REM sleep (15%) and frequent awakenings after 3 a.m. Her hypothesis: Evening screen work was disrupting her circadian rhythm and fragmenting her late, REM-rich cycles.*
This process transforms you from a passenger to a pilot. It removes guesswork and empowers you with knowledge about what your body specifically needs. The mission of Oxyzen as a brand is rooted in this empowerment—providing the precise, comfortable tools that enable this kind of lifelong self-discovery and optimization.
The pursuit of optimized sleep is supported by a growing ecosystem of technology designed to measure, analyze, and influence your sleep environment. Choosing the right tools is about understanding their strengths and integrating them into a cohesive system.
The choice of where to wear your primary sensor matters for accuracy and comfort.
Smart Rings (e.g., Oura, Oxyzen):
Wrist-Worn Trackers (e.g., Apple Watch, Fitbit, Whoop):
The Verdict for Sleep Optimization: For the singular focus on sleep stage accuracy and recovery metrics, the smart ring form factor currently holds an edge due to its superior physiological placement for nocturnal data capture.
Technology to shape your sleep environment is equally important.
Your wearable's companion app is your data dashboard. Look for:
The ideal setup is a sensor you trust (like a smart ring) providing the data, paired with environmental controllers (thermostat, lights) that automate the perfect conditions, all reviewed through an intelligent app that helps you understand your unique patterns. This creates a closed-loop system where measurement informs action, and action improves outcomes. To explore how one such system is designed from the ground up for this purpose, you can learn more about Oxyzen's integrated approach.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/