Sleep Stage Requirements: Do You Need Equal Time in Each?
You do not need equal time in each stage; a healthy pattern involves a balanced proportion of all stages across the night.
You do not need equal time in each stage; a healthy pattern involves a balanced proportion of all stages across the night.
For years, the quest for perfect sleep has been haunted by a single, pervasive myth: that truly restorative rest requires a perfectly balanced pie chart. We imagine our nights should be divided into neat, equal slices of light sleep, deep sleep, and REM sleep, chasing an elusive ideal where each stage gets its "fair share" of the night. This pursuit has led many of us down a rabbit hole of sleep tracker data, obsessing over percentages and feeling a pang of failure when our deep sleep dips by 2% or our REM cycle seems cut short.
But what if this fundamental premise is flawed? What if our bodies, in their infinite wisdom, are not designed for egalitarian sleep architecture, but for a dynamic, intelligent, and deeply personal rhythm that changes nightly?
The truth is, sleep is not a democratic process. It is a precisely orchestrated symphony of brainwaves, hormones, and physiological repairs, where the conductor is your own biology and the score is written by your daily life. The amount of time you spend in each sleep stage is not a target to be hit, but a readout to be understood—a complex language of recovery, memory processing, and hormonal regulation that is unique to you.
Modern technology, particularly advanced wearables like the Oxyzen smart ring, has given us an unprecedented window into this nocturnal world. For the first time, we can move beyond simply counting hours in bed and begin to decode the intricate ballet of our sleep cycles. This isn't about enforcing rigid equality; it’s about understanding intelligent allocation. Your brain doesn't waste a single minute of the night. It prioritizes what you need most, whether that’s extra deep sleep for physical recovery after a hard workout, prolonged REM for processing an emotionally charged day, or lighter sleep for maintaining environmental awareness during times of stress.
This article will dismantle the myth of equal sleep stages and guide you toward a more nuanced, empowering understanding of your sleep architecture. We will explore the non-negotiable roles of each stage, uncover the powerful factors that shift your personal sleep stage balance, and reveal how to interpret your own data not with anxiety, but with curiosity. The goal is not to control the symphony, but to learn its language, trust its conductor, and create the conditions for it to perform at its best.

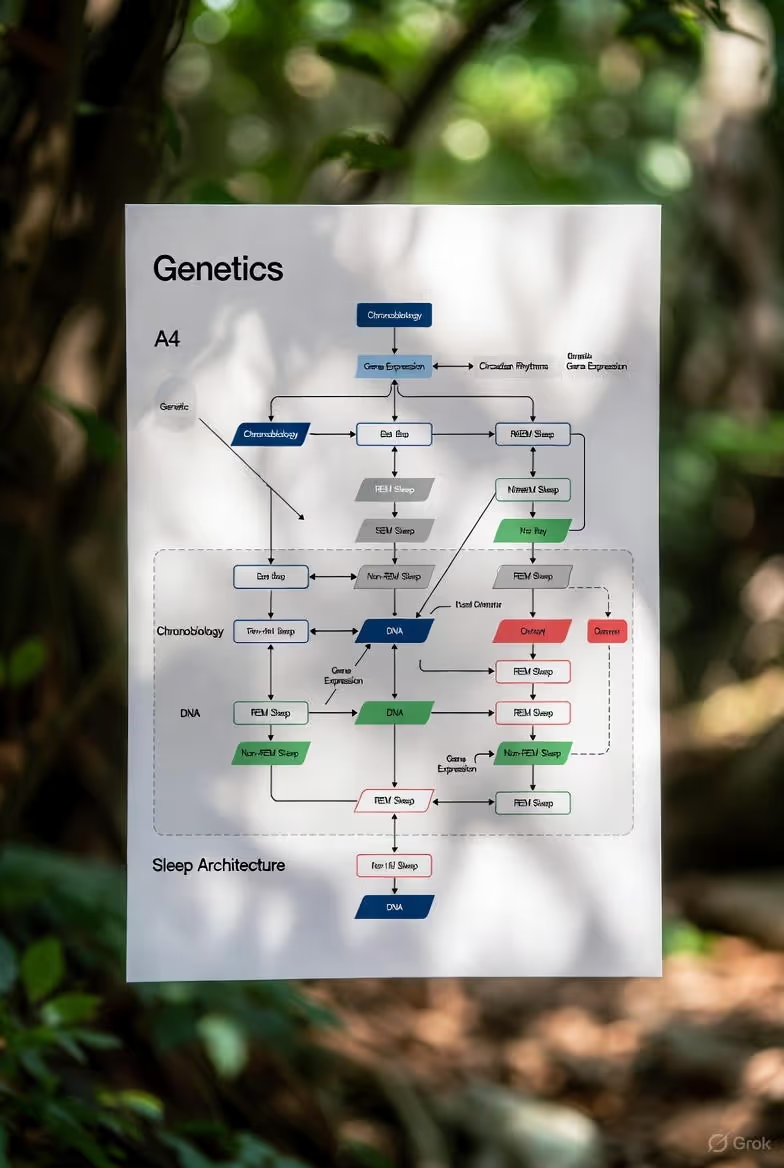
Before we can question the need for equality, we must first meet the players. Sleep is not a monolithic state of unconsciousness. It is a cyclical journey through four distinct stages, categorized into two broad types: Non-Rapid Eye Movement (NREM) sleep and Rapid Eye Movement (REM) sleep. Each cycle lasts roughly 90 to 120 minutes, and a healthy sleeper will journey through four to six of these cycles each night. The architecture of these cycles—the proportion and sequencing of stages—holds the key to understanding your sleep’s restorative power.
Stage 1 (N1): The Gateway. This is the lightest stage of sleep, lasting just a few minutes as you drift from wakefulness into slumber. Your brain produces alpha and theta waves, your muscles begin to relax, and you can be easily awakened. Think of it as the curtain rising on the night’s performance.
Stage 2 (N2): The Foundation. Accounting for approximately 40-60% of a typical adult’s night, Stage 2 is the workhorse of NREM sleep. It’s not as light as N1 nor as deep as N3, but it is critical for memory consolidation and cognitive maintenance. During this stage, your brain produces distinctive electrical signatures called sleep spindles and K-complexes. Sleep spindles are believed to play a key role in solidifying new information and protecting sleep from external disruptions, while K-complexes may aid memory and help synchronize neural networks. This is where your body temperature drops and your heart rate begins to slow, setting the stage for deeper restoration.
Stage 3 (N3): Deep Sleep / Slow-Wave Sleep. This is the most physically restorative phase of sleep. Characterized by slow, powerful delta brainwaves, deep sleep is when the body undertakes its most critical repair work. Human Growth Hormone (HGH) is released, facilitating tissue growth and muscle repair. The immune system is bolstered, cellular energy is restored, and the brain’s glymphatic system activates in overdrive to clear out metabolic waste. It’s notoriously difficult to wake someone from deep sleep, and if you are awakened, you’ll likely feel groggy and disoriented—a state known as sleep inertia. In the first half of the night, your cycles are dominated by deep sleep, which gradually gives way to longer REM periods as the night progresses.
Stage 4: REM Sleep. Often called "paradoxical sleep," REM is when the brain is almost as active as it is during wakefulness, while the body is in a state of temporary muscle paralysis (atonia). This is the primary stage for dreaming, emotional regulation, and complex memory processing. The brain sifts through the day’s experiences, consolidating learning, making creative connections, and integrating emotions. REM sleep is essential for mental and emotional health. As the night goes on, REM periods lengthen, with the final REM stage of the morning sometimes lasting up to an hour.
Understanding this basic architecture is the first step. The crucial insight is that these stages are not isolated compartments but interconnected phases of a holistic recovery process. The quality of your deep sleep influences the effectiveness of your REM, and the light sleep of Stage 2 provides the essential scaffolding for the entire structure. To obsess over one stage in isolation is to miss the symphony for a single note. For a deeper dive into how devices like smart rings track these nuanced stages, our comprehensive blog on sleep technology offers valuable insights.
The allure of a perfectly balanced sleep chart is understandable. In a world of quantified health, we seek clear targets: 10,000 steps, 8 glasses of water, 8 hours of sleep. It feels natural to extend this to 25% in each of the four stages. However, this desire for simplicity clashes violently with the beautiful complexity of human biology.
Sleep stage distribution is inherently and purposefully unequal. A normative benchmark for healthy young adults might look something like this:
Notice the imbalance immediately. Stage 2 is the dominant player, often occupying about half the night. Deep sleep and REM, while critically important, typically command smaller, though vital, shares. This isn't a design flaw; it's a design feature.
Furthermore, the distribution is not static within a single night. Your sleep follows a distinct architectural pattern known as "ultradian rhythm." In the first two sleep cycles, deep sleep (N3) is the star—long and dominant. This is when the bulk of physical restoration occurs. As the night progresses, deep sleep durations shrink, and REM sleep episodes grow longer. Your final cycle before waking may consist almost entirely of Stage 2 and a lengthy REM period. This evolution is strategic: physical repair is prioritized early when sleep drive is highest, while mental and emotional processing is saved for later, closer to wakefulness.
Chasing equal time per stage misunderstands this dynamic flow. It would be like insisting a symphony spend equal time on the opening motif, the development, and the crescendo. The power of the piece lies in the intentional variation and progression. Similarly, the restorative power of sleep lies in the intelligent, non-linear allocation of resources throughout the night.
Your brain is a sophisticated project manager, dynamically allocating "resources" (time in each stage) based on the "project needs" of your body and mind. Did you run a marathon? Expect a project plan heavy on deep sleep for tissue repair. Did you spend the day learning a new language or navigating complex emotional situations? The brain will prioritize REM sleep to consolidate those memories and process those feelings. This is why your sleep stage data should be viewed as a responsive dialogue, not a report card. Understanding this principle is at the heart of Oxyzen's mission to provide meaningful, personalized health insights, not just raw data.
If sleep is a restorative factory, deep sleep (N3) is the heavy machinery and maintenance shift. It is the cornerstone of physical health, a period of intense anabolic activity where the body repairs itself from the cellular level up. This stage is so critical that even a single night of deep sleep deprivation can have measurable negative effects.
The physiological processes that occur during deep sleep are nothing short of miraculous:
Given its vital role, how much deep sleep do you actually need? While individual needs vary, most adults require between 1.5 to 2 hours of deep sleep per night, which typically constitutes that 15-25% of total sleep. However, it’s not just about the total minutes; it’s about the quality and the timing. The deepest, most restorative slow-wave sleep is concentrated in the first half of the night. This is why "catching up" on sleep on the weekend is a flawed concept—you cannot retroactively induce those first, critical cycles of deep sleep you missed.
Factors that can rob you of this precious stage include chronic stress (which elevates cortisol, a deep-sleep antagonist), alcohol consumption (which may help you fall asleep but severely fragments and suppresses deep sleep later in the night), sleeping in a warm or noisy environment, and even natural aging, as deep sleep duration tends to decrease as we get older.
The takeaway is clear: while we don’t need equal time in all stages, we do have a non-negotiable baseline requirement for deep sleep. Prioritizing the conditions that foster it—cool, dark, and quiet environments, consistent sleep schedules, and stress management—is paramount for physical health. This focus on foundational health is a core part of our story at Oxyzen, where we develop technology to help you safeguard these essential biological processes.

While deep sleep is the body's mechanic, REM sleep is the mind's therapist, librarian, and creative director all in one. This psychologically rich stage is where the brain processes, files, and makes sense of your waking life. It’s less about physical restoration and more about cognitive and emotional housekeeping.
During REM sleep, your brain is a hive of activity. The amygdala (the emotional center) and hippocampus (the memory hub) are highly active, while the prefrontal cortex (the rational CEO) is less engaged. This unique neural cocktail is ideal for integrating memories with their emotional contexts without the filter of strict logic. Key functions of REM include:
So, how much REM is essential? Adults generally need about 90-120 minutes of REM per night, spread across the lengthening episodes in the later sleep cycles. This equates to the 20-25% benchmark. Unlike deep sleep, which is front-loaded, REM sleep is a privilege earned as the night progresses. This is why cutting your sleep short by 90 minutes in the morning can deprive you of your longest and most impactful REM period.
Factors that suppress REM sleep include many common medications (like certain antidepressants and stimulants), alcohol (which, again, is a major disruptor), sleep disorders like apnea, and irregular sleep schedules. Many users of advanced sleep trackers report seeing their REM score plummet after even a single glass of wine in the evening, a stark data point that reflects this biological interference.
The balance between deep sleep and REM is a delicate dance. They exist in a reciprocal relationship; deep sleep provides the physical stability that allows the brain to safely engage in the intense, chaotic activity of REM. One cannot be optimally healthy at the severe expense of the other. They are complementary, not competitive. Understanding this balance is a common topic in our user testimonials, where individuals share how tracking these patterns revealed the hidden impact of their lifestyle on mental clarity and emotional resilience.
Often dismissed as "less important" sleep, Stages 1 and 2 (with a focus on N2) are the unsung heroes of the sleep architecture. They serve as critical transitions, stabilizers, and preparatory phases without which deep sleep and REM could not function effectively. Light sleep is not failed deep sleep; it is a purposeful and active state with its own indispensable roles.
Stage 2 (N2) is particularly fascinating. It acts as a gatekeeper and a facilitator:
Attempting to minimize light sleep in favor of more "valuable" deep or REM sleep is a fundamental misunderstanding. A night with insufficient light sleep would be fragmented and unstable, like a building with no mortar between the bricks. The cycles would be disjointed, and the transitions into deeper, more vulnerable states would be compromised.
Furthermore, the proportion of light sleep often naturally increases with age. While deep sleep duration declines, the brain maintains a robust amount of Stage 2 sleep. This shift shouldn't necessarily be pathologized; it may represent an adaptive change in sleep architecture. The goal is not to fight this natural progression, but to ensure the light sleep you get is high-quality and stable, free from the micro-arousals caused by sleep disorders or poor sleep hygiene. For practical advice on optimizing all stages of sleep, including light sleep, our FAQ section addresses common user questions and concerns.
Your sleep stage percentages are not fixed genetic settings. They are a living, breathing reflection of your daily life, responding to a wide array of internal and external inputs. Understanding these factors transforms your sleep data from a static score into a dynamic story about your health and habits.
1. Age: The Primary Architect.
Age is the most powerful determinant of sleep structure. A newborn’s sleep is 50% REM, crucial for explosive brain development. By young adulthood, the pattern stabilizes into the classic 25% deep, 25% REM, 50% light split. From middle age onward, deep sleep (N3) begins a gradual but significant decline, often replaced by lighter Stage 2 sleep. Older adults may see deep sleep drop to less than 10% of the night, and sleep becomes more fragmented with more awakenings. This is a normal progression, not a disease, though it can increase sleep satisfaction concerns.
2. Physical Activity and Recovery.
Your body is an excellent accountant. Intense physical exertion, especially endurance or heavy strength training, creates a physiological debt that is repaid in deep sleep. Athletes often show increased deep sleep duration and intensity (higher amplitude slow waves) on nights following hard training. The body prioritizes tissue repair, muscle glycogen restoration, and HGH release. Conversely, sedentary periods can lead to a less pronounced deep sleep need.
3. Cognitive and Emotional Load.
A day filled with learning new skills, complex problem-solving, or high emotional stress sends a clear signal to the brain: "Prioritize REM." You may experience longer and more intense REM periods as your brain works to consolidate memories, integrate learning, and process emotional experiences. Students during exam periods or individuals going through emotionally taxing life events often report more vivid dreams—a hallmark of REM activity.
4. Sleep Debt and Circadian Rhythm.
When you are acutely sleep-deprived, your brain engages in "sleep stage rebound." On the recovery night, it will prioritize deep sleep above all else, often increasing its duration and intensity to catch up on physical restoration. Only after that debt is partially repaid will it then rebound into longer REM sleep on subsequent nights. Your circadian timing also plays a role; going to bed during your biological night (aligned with your natural melatonin release) promotes more robust and well-structured sleep cycles.
5. Substances and Medications.
6. Environment and Sleep Disorders.
A room that is too warm can inhibit the body’s natural temperature drop necessary for deep sleep. Noise pollution can increase micro-arousals, truncating deep and REM periods and inflating light sleep. Sleep apnea, characterized by repeated breathing interruptions, shatters sleep architecture, causing constant awakenings that prevent the sustained periods needed for deep and REM sleep.
Recognizing that your sleep is a mirror to your day empowers you to see patterns. That night of suppressed REM after a few drinks, or the spike in deep sleep after a marathon gardening session, are not data errors—they are biological confirmations. This principle of personalized response is central to the technology behind devices like the Oxyzen smart ring, which tracks these subtle nightly variations to provide context to your wellness journey.

In the age of wearables, we have more data than ever, but not always more wisdom. The path from raw percentages to peaceful sleep lies in intelligent interpretation. Here’s how to engage with your sleep stage data constructively, avoiding the trap of orthosomnia (an unhealthy preoccupation with perfect sleep data).
1. Look for Trends, Not Nightly Fluctuations.
A single night’s data point is a snapshot—often a blurry one. The true story is in the week-long or month-long trend. Did your deep sleep gradually increase as you started a new exercise routine? Has your REM sleep been consistently low during a period of high stress at work? Trends reveal the impact of lifestyle changes and chronic conditions, while single-night variations are often noise.
2. Correlate with How You Feel.
This is the golden rule. Your subjective feeling upon waking—refreshed, groggy, anxious—is a vital data point that no device can measure. If your tracker says you got 90 minutes of deep sleep but you feel like you were hit by a truck, trust your body. The data may be off, or it may be revealing an issue like sleep apnea that is making your deep sleep less restorative. Conversely, if you feel great but your REM is "low," you may simply need less, or the algorithm may be mis-scoring. Let your lived experience be the final judge.
3. Understand Device Limitations.
Consumer wearables like smart rings and watches use accelerometers, heart rate sensors, and heart rate variability (HRV) to estimate sleep stages. They are very good at detecting sleep vs. wake and can provide good relative trends (e.g., "you got more deep sleep this week than last"). However, they are not medical-grade polysomnography (PSG), which measures brain waves directly. Discrepancies of 10-20% in stage scoring are common. Use your device as a guide to patterns, not a clinical diagnostic tool.
4. Ask the Right Questions.
Instead of "Why wasn't my REM 25%?", ask:
5. Focus on Controllable Inputs, Not Outputs.
You cannot will yourself into more deep sleep. What you can control are the inputs that influence it: your sleep consistency, your bedroom environment, your wind-down routine, your alcohol intake, and your stress management. Obsess over perfecting those habits, not over the numbers they produce. The numbers will follow.
This balanced approach to data is something we strongly advocate. For those looking to delve deeper into understanding their biometrics, we encourage you to explore our blog for articles on data interpretation, sleep hygiene, and the science behind the sensors.
While you can’t directly control your sleep stages, you can pull powerful lifestyle levers that create the optimal conditions for your brain to allocate time wisely. Think of these as tuning the instrument so the conductor (your brain) can perform the symphony flawlessly.
To Support Deep Sleep (N3):
To Support REM Sleep:
To Support Stable, High-Quality Light Sleep:
Remember, these levers work synergistically. A cool, dark room supports both deep and REM sleep. Avoiding alcohol benefits REM and deep sleep stability. A consistent schedule strengthens your entire circadian framework. Your goal is to create a holistic sleep-supportive lifestyle, and the nuanced feedback from a device like the Oxyzen ring can help you see which levers have the most impact on your personal architecture. For more personalized strategies, our community often shares their successes in the testimonials section.
While variability is normal, certain persistent and severe imbalances can be red flags for underlying health issues or sleep disorders. It’s important to know when your data might be pointing toward a need for professional consultation, rather than just a bad night.
1. Chronically Low or Absent Deep Sleep.
If your tracker consistently shows near-zero deep sleep over weeks (and you feel unrefreshed), it’s worth investigating. Potential causes include:
2. Chronically Suppressed REM Sleep.
Persistently low REM (outside of the known effects of medications like SSRIs) is less common but can be significant. It’s associated with:
3. Excessive Deep or REM Sleep.
While often seen as desirable, extremes can be problematic.
4. Extreme Fragmentation and Lack of Cycling.
The complete absence of clear, cyclical patterns—constant bouncing between light sleep and wakefulness with no sustained deep or REM—is a major red flag. This is the hallmark of severely disrupted sleep, seen in conditions like untreated sleep apnea, severe insomnia, or circadian rhythm disorders.
When to Seek Help:
If your data shows persistent, severe deviations and you are experiencing debilitating daytime symptoms—such as excessive fatigue, cognitive impairment, mood disturbances, or loud, chronic snoring—it is time to consult a sleep specialist. Bring your long-term trend data from your wearable; while not diagnostic, it can provide a useful picture of your home sleep patterns and guide further testing, such as a clinical polysomnogram. For general questions on how wearables can complement professional care, our FAQ offers some preliminary guidance.
We are standing on the brink of a revolution in sleep science, moving far beyond the one-size-fits-all model of "8 hours with equal stages." The future lies in hyper-personalized sleep optimization, where your unique biology, daily context, and long-term goals guide your sleep strategy.
Biomarker-Responsive Sleep Guidance.
Imagine a device that doesn't just track your sleep stages but understands their cause. Future algorithms will integrate sleep data with continuous glucose levels, cortisol patterns, core body temperature, and detailed HRV analysis. They could say: "Your deep sleep was fragmented because your blood sugar spiked at 2 a.m.," or "Your REM was strong because your daytime stress biomarkers were low." This moves from what happened to why it happened, enabling truly precise interventions. This integrated approach to wellness is at the core of Oxyzen's vision for the future of health technology.
Adaptive Sleep Scheduling and Cycle Alignment.
Instead of a fixed alarm, smart systems could learn your personal sleep cycle length and wake you during the lightest sleep phase within a desired time window, minimizing sleep inertia. Further out, they may recommend personalized bedtimes based on your circadian type (night owl vs. early bird) and the next day's cognitive demands, optimizing your architecture for the challenge ahead.
Precision Nutrition and Supplementation.
Research into sleep-supportive nutrients (magnesium, glycine, apigenin) will become more personalized. Based on your sleep architecture and genetic predispositions, a system could suggest specific dietary tweaks or supplement timing to gently support the stages you naturally lack, moving beyond blanket recommendations.
Closed-Loop Sleep Environments.
Your bedroom itself will become an active partner in sleep optimization. Smart beds, lighting, and climate systems will respond in real-time to your sleep stage (as estimated by your wearable). They might gradually cool the room as you enter deep sleep, introduce subtle rhythmic thermal pulses to stabilize light sleep, or use precisely timed sounds to enhance sleep spindle activity, all to reinforce your natural cycles.
In this future, the question "Do I need equal time in each sleep stage?" will seem charmingly antiquated. The focus will shift entirely to: "What is my unique sleep architecture telling me I need tonight to be healthier, sharper, and more resilient tomorrow?" The goal is a seamless, intelligent partnership between technology and biology, where data flows into actionable wisdom that respects and enhances the body's innate intelligence. This journey of discovery and optimization is one we are deeply committed to, and we invite you to learn more about how we're building this future.
If lifestyle choices and daily activities are the daily weather patterns of your sleep, then genetics and chronobiology are the enduring climate. These are the deep, foundational factors that set your personal baseline—the inescapable, hardwired code that shapes your propensity for certain sleep stage distributions, your ideal timing for sleep, and even your vulnerability to specific sleep disorders. Understanding this layer is key to moving from fighting your nature to working harmoniously with it.
The Genetic Blueprint of Sleep Stages
Twin studies have provided some of the most compelling evidence for the heritability of sleep architecture. Research suggests that the proportion of time spent in different sleep stages has a significant genetic component, with heritability estimates ranging from 30% to 50%. This means that your natural tendency to be a "deep sleep champion" or a "REM sleep heavyweight" is partly inherited.
Specific genetic variations are being linked to sleep traits:
This genetic underpinning is why a one-size-fits-all sleep stage target is biologically nonsensical. Your optimal architecture is uniquely yours, informed by a code written at conception. The journey is to find the lifestyle that allows your genetic potential to express itself optimally, a philosophy deeply embedded in Oxyzen's approach to personalized data.
Chronotype: Your Body's Internal Schedule
Your chronotype is your genetically predisposed inclination to sleep and be active at certain times. It's the reason some people are vibrant at 6 a.m. while others hit their peak at 10 p.m. Chronotype powerfully influences sleep architecture because it dictates when, relative to your biological night, you actually go to sleep.
The Master Regulators: The Two-Process Model in Depth
Your sleep-wake cycle is governed by two primary, interacting biological processes, elegantly described by the Two-Process Model. This isn't an abstract theory; it's the operating system for your sleep architecture.
Process S (Sleep Homeostasis): Think of this as your "sleep pressure" tank. The chemical adenosine builds up in your brain from the moment you wake, steadily increasing your drive for sleep. During sleep, especially deep NREM sleep, this tank is drained. The longer you're awake, the fuller the tank, the higher the pressure, and the deeper and more intense your subsequent deep sleep will be. Process S is the primary driver for the amount of deep sleep you get. After a long, taxing day, Process S ensures you get a strong dose of physical restoration.
Process C (Circadian Rhythm): This is your 24-hour internal clock, orchestrated by the suprachiasmatic nucleus (SCN) in your brain. It’s not a simple "sleep clock" but a rhythm of alertness and sleepiness that ebbs and flows. It creates a "wake maintenance zone" in the late evening (making it hard to fall asleep just before your natural bedtime) and a strong drive for sleep in the middle of your biological night. Crucially, Process C modulates the type of sleep you get. It promotes REM sleep during the latter part of your sleep episode, independent of how long you've been asleep. Even if you nap at 3 p.m., you're unlikely to hit REM because Process C isn't in the REM-promoting phase.
The magic—and the complexity—lies in the interaction. Process S builds the need, and Process C opens the "sleep gate" at the appropriate biological time. Your sleep architecture is the product of this negotiation. If you go to bed when Process S is high (sleep-deprived) but Process C is still in a wake-promoting phase (due to an evening chronotype or late light exposure), you may fall asleep quickly but experience fragmented sleep with less efficient deep sleep. Conversely, perfect alignment creates the conditions for robust, well-structured cycles.
Understanding this model explains why simply going to bed earlier or later doesn't always fix sleep problems. It's about aligning your habits with your internal, genetically-influenced physiology. For many, discovering their chronotype through tracking devices is the first step toward this alignment, a story echoed in numerous user experiences shared on our site.
Your sleep architecture is not a static monument but a river, constantly changing and flowing through the landscape of your life. From the explosive neural development of infancy to the consolidation of adulthood and the subtle shifts of older age, each life stage presents a different "job" for sleep, reflected in dramatic changes in stage distribution. Charting this evolution helps normalize age-related changes and distinguish them from potential disorders.
Infancy and Childhood: The REM-Dominated Construction Phase
A newborn’s sleep is a world apart from an adult’s. They sleep 14-17 hours per day, divided into multiple short cycles. The most striking feature is the dominance of REM sleep, which constitutes about 50% of total sleep time. This "active sleep" is crucial for the phenomenal brain development occurring in early life. The brain is forming millions of neural connections per second, and REM sleep is believed to play a vital role in this synaptic pruning and pathway formation, as well as in the maturation of visual and sensory systems. Deep sleep (N3) is present but not as pronounced in early infancy, gradually increasing as the child grows.
As children move into the preschool and school-age years, REM sleep decreases to near-adult levels (around 25%), and deep sleep reaches its lifetime peak. Children are often deep sleep powerhouses, able to sleep through thunderstorms and fire alarms, reflecting the intense physical growth and immune system development occurring during this stage.
Adolescence: The Great Delay and REM Rebound
Puberty brings a well-documented circadian shift toward eveningness. The adolescent melatonin release is delayed, making it biologically challenging to fall asleep early. When combined with early school start times, this creates a perfect storm of chronic sleep deprivation. The consequence? On weekends, when allowed to sleep in, teens experience a massive REM sleep rebound. Their brains, starved for emotional and memory processing during the week, seize the opportunity. This is not laziness; it's a biological imperative. The adolescent brain is undergoing a second wave of massive reorganization, particularly in the prefrontal cortex, and REM sleep is essential for this maturation.
Adulthood: The Plateau of Consolidation
In healthy young and middle-aged adults, sleep architecture stabilizes into the classic pattern we’ve discussed: ~5% N1, ~50% N2, ~20-25% N3 (deep), and ~20-25% REM. This is the maintenance phase. Sleep supports daily physical repair, cognitive performance, emotional stability, and metabolic health. However, the decline of deep sleep begins subtly as early as the late 20s or 30s. Lifestyle factors—career stress, parenthood, changing health—now become the primary sculptors of nightly variation around this stable baseline.
Older Adulthood: The Shift Toward Lighter Sleep
The changes in later life are often misinterpreted as "poor sleep." In normal, healthy aging:
Critically, feeling unrefreshed is not a normal part of aging. While architecture changes, the perception of non-restorative sleep is often due to other factors: medical conditions, medications, pain, or primary sleep disorders like sleep apnea, whose prevalence increases with age. Differentiating between normal architectural evolution and treatable pathology is key to maintaining quality of life. The nuanced tracking offered by devices like the Oxyzen smart ring can help individuals and their healthcare providers make this important distinction.
While sleep stages provide a structural map of the night, they are not the only—or even always the most important—metrics for assessing sleep quality and recovery. Several other physiological parameters, often measured simultaneously by advanced wearables, paint a fuller picture of your nervous system's state and your body's readiness for the day. To focus solely on stages is to read only the chapter titles of a complex novel.
Heart Rate Variability (HRV): The Golden Metric of Autonomic Balance
HRV is the subtle variation in time between successive heartbeats. It is not an anomaly; it is a sign of a healthy, responsive heart being dynamically guided by the autonomic nervous system (ANS).
Resting Heart Rate (RHR) and Its Nocturnal Dip
A healthy cardiovascular system shows a distinct drop in heart rate during sleep, typically reaching its lowest point (the nadir) during deep sleep phases. This nocturnal dip (usually a 10-20% decrease from daytime resting rates) is a sign of efficient autonomic regulation.
Respiratory Rate and Stability
Your breathing rate during sleep is a stable, telling biomarker. Normal adult rates are between 12-20 breaths per minute. Significant increases can indicate:
A stable, low respiratory rate throughout the night is another marker of a nervous system in a state of deep, unbroken recovery.
Sleep Onset Latency and WASO: The Bookends of Consolidation
Integrating the Picture
The most powerful insights come from correlation. For example:
This holistic interpretation moves you from being a stage-counting accountant to a sleep-quality strategist. Learning to read these interconnected signals is a journey, and resources like the Oxyzen blog are dedicated to helping users develop this literacy.
To move from theory to practical understanding, let’s walk through hypothetical but data-informed case studies. These illustrate how the factors we’ve discussed—lifestyle, stress, age, chronotype—manifest in real sleep data and subjective experience. (Note: These are composite examples based on common patterns).
Case Study 1: The Overtrained Marathoner (Physical Load Dominant)
Case Study 2: The Stressed Project Manager (Cognitive/Emotional Load Dominant)
Case Study 3: The "Healthy" 60-Year-Old (Age-Related Shifts)
In our quest for perfect sleep, a paradoxical and counterproductive disorder has emerged in the digital age: orthosomnia. Coined by sleep researchers, this term describes an unhealthy preoccupation with achieving perfect sleep data, leading to increased anxiety, worsened sleep, and a vicious cycle of obsession.
Orthosomnia is the shadow cast by the very light of self-quantification. It turns a tool for awareness into a source of performance pressure. The individual becomes a sleep perfectionist, where the goal is no longer feeling rested, but seeing "green" scores and "ideal" percentages on their dashboard.
The Symptoms of Data-Driven Sleep Anxiety:
How to Avoid the Trap: A Healthy Relationship with Sleep Data
The technology is meant to be a servant, not a master. Its purpose is to provide gentle feedback and reveal patterns, not to become a nightly source of judgment. Developing this balanced mindset is crucial for long-term success with any wellness tracking, a topic we often address to help users get the most from their journey with Oxyzen.
Armed with a nuanced understanding of sleep stages, their influencers, and the bigger picture metrics, you are now ready to construct a personalized plan. This is not about rigidly controlling outcomes, but about intelligently managing inputs to create the conditions for your best possible sleep. Follow this step-by-step blueprint.
Phase 1: The Baseline Assessment (4 Weeks)
Phase 2: Targeted, Single-Variable Experiments (2-3 Weeks Each)
Based on your baseline, choose ONE factor to modify. Changing too much at once makes it impossible to see what's working.
Phase 3: Integrate and Refine
Adopt the experiments that yielded clear, positive results in your data and how you felt. Discard those that didn't or added stress. Slowly build a sustainable, personalized sleep-supportive lifestyle from these proven components.
When to Bring in a Professional:
Use your collected data as a powerful tool for conversation. If, after optimizing lifestyle factors, you still see:
The journey to better sleep is iterative and personal. It requires curiosity, patience, and a willingness to be your own sleep scientist. For ongoing support and to see how others have navigated this process, the community and resources found through Oxyzen's platform can be an invaluable companion on this path.
Emerging research is revealing one of the most fascinating and complex relationships in human biology: the bidirectional communication network between your gut microbiome and your brain, with sleep architecture as a central player in this dialogue. The trillions of bacteria residing in your digestive tract do far more than aid digestion; they produce neurotransmitters, modulate inflammation, and send signals that directly influence the quality and structure of your sleep.
Neurotransmitter Production: The Gut’s Pharmacy
Your gut microbiome is a prolific biochemical factory. Many strains of bacteria are responsible for producing or influencing the precursors to key sleep-regulating neurotransmitters:
Inflammation and Circadian Disruption
A dysbiotic gut often leads to increased intestinal permeability ("leaky gut") and systemic inflammation. Circulating inflammatory cytokines, such as interleukin-1β and tumor necrosis factor-alpha, are potent sleep-modulators. They can:
Furthermore, the gut microbiome itself has a circadian rhythm. Its composition and function fluctuate over a 24-hour period, synchronized by your feeding times and sleep-wake cycle. Jet lag, shift work, or erratic eating patterns can desynchronize this microbial rhythm, which in turn sends conflicting signals to the brain’s master clock, worsening sleep disruption.
Dietary Levers for a Sleep-Supportive Microbiome
You can cultivate a microbiome that supports healthy sleep architecture through deliberate dietary choices:
The takeaway is profound: the path to better deep sleep and stable REM may well begin at your dinner plate. A diet that diversifies and nourishes your gut microbiome creates a foundation of reduced inflammation and optimized neurochemical production, setting the stage for more resilient sleep architecture. For more on the intersection of nutrition, gut health, and quantified wellness, resources on our blog delve deeper into these connections.
Light is not just something that allows you to see; it is the primary zeitgeber (time-giver) for your master circadian clock. The quality, quantity, and timing of light exposure you receive are arguably the most powerful environmental tools you have for shaping not just when you sleep, but how well you sleep across all stages.
The Melanopsin System: Your Body's Light Meter
Deep within your eyes are specialized, non-visual photoreceptor cells called intrinsically photosensitive retinal ganglion cells (ipRGCs). They contain a photopigment called melanopsin, which is exquisitely sensitive to short-wavelength blue light (around 480 nanometers). These cells do not help you see images; they send signals directly to your suprachiasmatic nucleus (SCN) to synchronize your internal clock with the external world.
Beyond Blue: The Role of Light Intensity and Spectrum Throughout the Day
While blue light gets most of the attention, the full spectrum and intensity of light matter.
Practical Light Hygiene for Optimal Sleep Architecture
By consciously managing your light exposure, you are not just helping yourself fall asleep; you are programming your circadian biology to orchestrate a more harmonious, well-structured night of deep and REM sleep. This foundational principle of working with biology, not against it, is central to the holistic vision behind Oxyzen.