Anxiety Reduction for OCD: Managing Intrusive Thoughts and Compulsions
Methods for managing anxiety associated with Obsessive-Compulsive Disorder.
Methods for managing anxiety associated with Obsessive-Compulsive Disorder.
You’re trying to focus on a meeting, enjoy a meal, or fall asleep, but it’s there—an unwelcome, disturbing thought that crashes into your mind like a trespasser. It feels urgent, dangerous, and true. Your heart rate climbs, a cold dread settles in your stomach, and a desperate need to do something to make it stop takes over. You perform a mental ritual, a physical check, or seek a futile reassurance, earning a fleeting moment of relief before the cycle begins anew. This is the exhausting, often invisible, reality of living with Obsessive-Compulsive Disorder (OCD). It’s not a quirk or a preference for cleanliness; it’s a clinically recognized anxiety disorder where the brain gets stuck in a loop of intrusive thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) performed to neutralize the distress.
Yet, in this age of hyper-connectivity and relentless stress, a profound shift is occurring. We are moving beyond simply managing symptoms to fundamentally understanding and rewiring our response to anxiety. This journey isn't about achieving a thoughtless vacuum of a mind—an impossible and undesirable goal. It’s about changing your relationship with your thoughts, building resilience from the inside out, and leveraging both timeless wisdom and cutting-edge technology to reclaim your mental space and peace. In this comprehensive guide, we will explore the intricate neuroscience of OCD, dismantle the myths that fuel shame, and provide you with a robust, multi-faceted toolkit for anxiety reduction. From evidence-based psychotherapies and mindfulness practices to the revolutionary role of biometric feedback from devices like the Oxyzen smart ring, we will chart a path from turmoil to tranquility. This is your map for navigating the storm and discovering the calm that exists within you, even now.
Obsessive-Compulsive Disorder is often tragically misunderstood in popular culture, reduced to a caricature of excessive hand-washing or neatness. This minimization does a profound disservice to the millions who experience its debilitating grip. Clinically, OCD is defined by the presence of obsessions, compulsions, or both, which are time-consuming (take more than one hour per day) and cause significant distress or impairment in social, occupational, or other important areas of functioning.
Obsessions are recurrent and persistent thoughts, urges, or images that are experienced as intrusive and unwanted. They are not simply excessive worries about real-life problems. The individual attempts to ignore or suppress such thoughts, urges, or images, or to neutralize them with some other thought or action (i.e., by performing a compulsion). Common obsession themes include:
Compulsions are repetitive behaviors or mental acts that an individual feels driven to perform in response to an obsession or according to rigid rules. The behaviors are aimed at preventing or reducing anxiety or preventing a dreaded event; however, they are not connected in a realistic way to what they are designed to neutralize, or are clearly excessive. Examples include:
The critical engine of OCD is not the content of the thought—virtually everyone has intrusive, strange thoughts—but the catastrophic misinterpretation of its importance. The OCD brain sends a false alarm: “This thought is dangerous and means something terrible about you. You must act to fix it.” The compulsion is the futile attempt to pull the fire alarm when there is no fire, which only teaches the brain that the alarm system itself is vital, strengthening the circuit for next time. Understanding this faulty loop—the obsession causing distress, the compulsion providing temporary relief, and the resultant reinforcement of the fear—is the first, crucial step toward breaking free from it. To learn more about the mind-body connection in anxiety disorders, you can explore related articles on our blog.
To effectively manage OCD, it helps to understand the “where” and “how” inside your own brain. Modern neuroimaging studies have illuminated a specific circuit that becomes hyperactive and dysregulated in OCD, often called the “worry circuit.” This involves a dysfunctional conversation between several key regions:
When this circuit is stuck in overdrive, it creates a state of hyper-awareness and hyper-responsibility. The brain cannot register the “completion” of a task or thought, leading to the need for repetitive checking or mental rituals. Furthermore, the neurotransmitter serotonin is heavily implicated in modulating this circuit. Many effective medications for OCD (SSRIs) work by increasing serotonin availability, which can help calm the overactive signaling.
But neuroscience isn’t just about pathology; it’s also about neuroplasticity—the brain’s ability to rewire itself based on experience. This is the foundation of hope. Every time you resist a compulsion and sit with the anxiety, you are not just “being brave.” You are actively engaging in a form of exposure therapy that weakens the synaptic connections in the fear circuit and strengthens pathways in the prefrontal cortex associated with rational appraisal and tolerance of uncertainty. You are, quite literally, reshaping your brain’s architecture with your behavioral choices. This biological perspective transforms recovery from a vague concept of “willpower” into a tangible, physiological process of healing.
If fighting intrusive thoughts directly only makes them stronger (a phenomenon known as ironic process theory), what is the alternative? The answer lies in a radical shift in strategy: from thought control to thought acceptance. This is the cornerstone of modern, evidence-based approaches like Acceptance and Commitment Therapy (ACT) and Mindfulness-Based Cognitive Therapy (MBCT).
The default human response to a distressing thought is to engage with it: to argue with it, analyze it, suppress it, or obey it. With OCD, this engagement is the compulsion (whether mental or physical). Cognitive defusion is a set of techniques designed to change how you relate to your thoughts, rather than changing the thoughts themselves. It’s about seeing thoughts for what they are—transient strings of words and images produced by the brain—not direct reflections of reality or commands that must be obeyed.
Practical Defusion Techniques:
The goal of defusion is not to feel good, but to get you out of a futile war with your private experiences so you have the freedom to act on your values. It creates space between the trigger (the intrusive thought) and your response (the urge to compulse). In that space lies your power to choose a different path. This foundational skill is what makes the subsequent, more active steps of Exposure and Response Prevention possible. For a deeper dive into mindfulness techniques that support this practice, consider reading our complete guide on mindful awareness.
While acceptance sets the stage, Exposure and Response Prevention (ERP) is the active, core behavioral intervention that has earned its status as the “gold standard” psychotherapy for OCD. ERP works directly on the conditioned fear response by breaking the link between the obsession (the feared stimulus) and the compulsion (the avoidance behavior). It’s based on the well-established principle of habituation: when you remain in the presence of a feared situation long enough without escaping or neutralizing it, your anxiety will naturally peak and then subside on its own. Your brain learns, through direct experience, that the feared outcome does not occur, and that the anxiety itself is tolerable and temporary.
ERP is a structured, hierarchical process:
Example: For someone with harm obsessions about their stove being left on, an ERP task might involve:
ERP is challenging work, but it is arguably the most potent and empowering treatment for OCD. It moves you from a passive victim of your thoughts to an active scientist, conducting behavioral experiments that prove your OCD wrong. For those curious about how objective data can support such therapeutic work, discover how Oxyzen works by providing real-time feedback on your physiological state during these challenging moments.
If ERP is the behavioral “doing” of recovery, mindfulness is the foundational “being.” Mindfulness, simply defined, is paying attention to the present moment, on purpose, and without judgment. For the OCD mind—which is perpetually time-traveling into catastrophic futures or ruminating on past actions—this is a revolutionary act.
Mindfulness training directly targets the core pathology of OCD: cognitive fusion and aversion to inner experience. It strengthens the “observing self,” the part of you that can notice thoughts, feelings, and sensations without being swallowed by them. This is not about achieving a blank mind or a state of blissful relaxation (though that may occur). It is about building meta-awareness—the ability to recognize, “Oh, I am currently caught in an obsessive loop,” which is the essential first step to disengaging from it.
Specific Applications for OCD:
Research shows that mindfulness-based interventions can lead to significant reductions in OCD symptoms, particularly when combined with ERP. They reduce activity in the default mode network (the brain’s “rumination circuit”) and increase connectivity in regions associated with cognitive control. By learning to observe the anxious storm from the steady, quiet eye within it, you fundamentally change your relationship to the entire experience. The company behind Oxyzen was founded on this very principle of harnessing inner awareness through technology, a journey you can learn about in our story of vision and values.
The brain is an organ, and like any organ, its function is profoundly influenced by the body’s overall state. Viewing OCD management solely through a psychological lens misses a critical piece of the puzzle: neurobiological regulation. You cannot expect a sleep-deprived, malnourished, and sedentary brain to have the resilience needed to do the hard work of ERP and mindfulness. Lifestyle factors are the bedrock of stability.
Sleep: Sleep deprivation is a potent anxiety trigger. It increases activity in the amygdala (the brain’s fear center) and decreases connectivity with the prefrontal cortex (the rational regulator). For someone with OCD, a single poor night’s sleep can lead to a dramatic increase in intrusive thoughts and a decreased ability to resist compulsions. Prioritizing 7-9 hours of quality sleep is non-negotiable. Establishing a consistent sleep schedule, creating a dark/cool environment, and implementing a “wind-down” routine are acts of direct OCD management.
Nutrition: The gut-brain axis is a well-established communication pathway. Diets high in processed sugars and refined carbohydrates can cause blood sugar spikes and crashes, leading to mood instability and heightened anxiety. Conversely, a diet rich in whole foods—fruits, vegetables, lean proteins, healthy fats, and complex carbohydrates—provides a steady supply of energy and the necessary building blocks for neurotransmitters like serotonin. Omega-3 fatty acids (found in fish, walnuts, flaxseeds) have anti-inflammatory properties and are linked to improved brain health. Staying hydrated is equally critical, as even mild dehydration can increase cortisol (the stress hormone).
Movement: Exercise is a powerful, natural anti-anxiety treatment. It burns off excess stress hormones like adrenaline and cortisol, releases endorphins (natural mood lifters), and promotes the release of brain-derived neurotrophic factor (BDNF), a protein that supports neuroplasticity—the very mechanism of learning and recovery. Crucially, exercise also serves as a form of contextual exposure. The increased heart rate, sweating, and shortness of breath mimic anxiety symptoms. By tolerating these sensations in a positive context, you learn they are not inherently dangerous, which can help you better tolerate them during an OCD spike. Even a daily 30-minute brisk walk can yield significant benefits.
Managing these pillars isn’t about perfection; it’s about creating a physiological foundation that gives your psychological tools a fighting chance. When your nervous system is more regulated, you have a wider “window of tolerance” for distress, making every other strategy more effective. For support on integrating wellness tracking into your lifestyle routine, our FAQ page offers helpful guidance.
We live in an era where technology can extend our self-awareness in unprecedented ways. While our subjective feeling of anxiety is real, our perception of our own physiological state can be surprisingly inaccurate. You might feel “extremely anxious” for hours, not noticing the subtle shifts and downturns in your actual arousal. This is where biometric feedback from wearable devices like the Oxyzen smart ring becomes a game-changer in modern anxiety and OCD management.
The Oxyzen ring continuously and passively tracks key biomarkers of your autonomic nervous system (ANS) state:
How This Data Empowers OCD Management:
Technology like the Oxyzen ring doesn’t replace therapy; it augments it. It acts as an objective coach, providing feedback that cuts through the subjective fog of anxiety and helps you build a more accurate, compassionate, and empowered relationship with your own body and mind. It embodies the mission of our company: to fuse human insight with technological innovation for better well-being, a principle you can learn more about on our about page.
Recovery from OCD is not a linear journey to a fixed destination where intrusive thoughts never occur. It is the ongoing process of building a robust, flexible system of resilience—a toolkit you can reach into daily to maintain balance and navigate inevitable challenges. This toolkit should include micro-practices that strengthen your psychological and physiological armor.
Your Daily Resilience Toolkit Might Include:
Consistency with these small practices is far more powerful than occasional grand efforts. They are the daily reps that build the mental muscle of resilience, making you less susceptible to being hijacked by the OCD loop when stress inevitably arises. For inspiration on how others have built their own wellness routines, you can read real user experiences and testimonials.
Inevitably, there will be days, or even weeks, where it feels like you’ve taken steps backward. A new stressor emerges, an old obsession returns with surprising force, or you find yourself performing a compulsion almost automatically. In the old paradigm, this is called a “relapse” and is often met with crushing self-criticism: “I’ve failed. All my progress is lost. I’ll never beat this.” This harsh response is not only painful but counterproductive, often triggering more anxiety and compulsive behavior.
A more compassionate and accurate model is to view recovery as a spiral, not a straight line. You may revisit familiar challenges, but from a slightly higher perspective, with more tools and knowledge than before. A “setback” is simply data—a sign that your current stressors have exceeded your current coping capacity. It is not a failure; it is feedback.
How to Navigate a Setback with Self-Compassion:
Research by Dr. Kristin Neff and others has consistently shown that self-compassion is strongly associated with mental health and resilience. It lowers cortisol levels, reduces anxiety, and fosters a growth mindset. In the context of OCD, self-compassion directly targets the shame and self-loathing that often fuel the disorder. By meeting your own suffering with kindness, you begin to heal the very ground in which OCD takes root. For additional resources and support on this continuous journey, remember that you can always explore our blog for more wellness tips.
Integrating Therapy Modalities: ERP, ACT, and Beyond
While Exposure and Response Prevention (ERP) stands as the behavioral powerhouse for OCD treatment, the therapeutic landscape is enriched by integrating complementary modalities. This integrative approach addresses not just the behavioral loop, but the underlying cognitive, emotional, and existential struggles that often accompany the disorder. Think of it as using a full toolkit: ERP is the precise wrench, but sometimes you need a hammer, a level, or a screwdriver to build a stable structure.
Acceptance and Commitment Therapy (ACT) is arguably ERP's most synergistic partner. While ERP focuses on changing your behavioral response to fear, ACT focuses on changing your relationship with your internal experience. Its core framework, known as the "Hexaflex," provides a robust psychological model for flexibility:
In practice, an integrative ACT+ERP approach means you might engage in an exposure not just to "habituate to fear," but as a valued action. For example, if you value being a present parent, your exposure might involve playing with your child in a "messy" environment (triggering contamination fears) without washing, framing it as "making room for anxiety so I can be the engaged parent I want to be." This adds a layer of motivation and meaning beyond symptom reduction.
Inference-Based Cognitive Therapy (ICBT) is another specialized modality that targets a specific cognitive flaw in OCD: the confusion between imaginary possibility and realistic probability. ICBT posits that individuals with OCD get stuck in a "narrative" built on irrelevant details and remote possibilities, mistaking it for reality. Therapy involves helping the client distinguish between "inferential confusion" (a story the OCD mind constructs) and "reality-based information" from the senses and common sense. By learning to distrust the OCD narrative and trust reality-based reasoning, the urge to compulse naturally diminishes.
An effective therapist skilled in these modalities will weave them together fluidly. They might use Cognitive Behavioral Therapy (CBT) principles to challenge the initial catastrophic interpretations, employ ACT metaphors to foster acceptance, and design ERP exercises to behaviorally test the new learning. The goal is a personalized protocol that not only reduces symptoms but also builds a more psychologically flexible, values-driven life. For those seeking to understand the broader philosophy behind such integrative, human-centric approaches to wellness, you can learn more about our mission and vision.
For many individuals, particularly those with moderate-to-severe OCD, psychotherapy alone may not be sufficient. Medication can be a vital component of treatment, helping to lower the overall "volume" of anxiety and intrusive thoughts enough for therapy skills to take hold. It’s important to view medication not as a "crutch" or a sign of failure, but as a biological intervention that corrects a neurochemical imbalance, much like insulin for diabetes.
First-Line Pharmacotherapy: SSRIs
Selective Serotonin Reuptake Inhibitors (SSRIs) are the most commonly prescribed and well-researched medications for OCD. They work by increasing the availability of serotonin in the synaptic cleft, which over time helps modulate the overactive fear circuit (OFC-ACC-caudate loop). Common SSRIs used for OCD include:
Key Considerations with SSRIs for OCD:
Adjunct and Second-Line Medications:
The decision to use medication is a personal one, made in collaboration with a knowledgeable psychiatrist. It is most powerful when combined with therapy (CBT/ERP). Medication can provide the neurochemical stability to engage fully in the challenging work of ERP, creating a positive feedback loop where behavioral success further reinforces brain changes. If you have questions about how lifestyle tracking can complement a treatment plan that includes medication, our FAQ section provides supportive information.
OCD is an isolating disorder. The very nature of intrusive thoughts can make you feel alien, broken, or dangerous. Compulsions are often performed in secret. This isolation is both a symptom and a fuel for the disorder. Therefore, deliberately and courageously building a connected support system is not a luxury—it is a critical component of recovery.
The Therapeutic Relationship: Your therapist is your primary ally and guide. A strong, trusting relationship with a therapist who specializes in OCD is paramount. They provide a safe, non-judgmental space to expose your most frightening thoughts, offer expert guidance through ERP, and model acceptance and compassion. They are your coach in the ring, and finding the right fit is essential.
Involving Family and Partners (Family-Based Treatment): Loved ones often become unintentionally entangled in OCD rituals, providing reassurance or participating in avoidance ("Just check the lock for him so he can relax"). This is called family accommodation, and while done out of love, it directly reinforces the OCD. Psychoeducation for family members is vital. They need to understand OCD as a neurobiological disorder, not a personal choice. Involving them in therapy can teach them how to:
Peer Support and Community: Connecting with others who "get it" can be profoundly healing. Support groups, whether in-person or online (through organizations like the International OCD Foundation - IOCDF), provide:
Building this system requires vulnerability, but it transforms a solitary battle into a shared journey. It reminds you that you are not your OCD; you are a person worthy of connection and support, fighting a disorder. For stories of how others have navigated their wellness journeys with support, you can find inspiration in real customer reviews and experiences.
"Pure O" (Purely Obsessional OCD) is a misleading but common term for OCD where the compulsions are primarily covert—hidden mental rituals like analyzing, reviewing, thought suppression, or seeking internal reassurance. The suffering is intense because the battle is invisible, raging entirely within the mind. For "Pure O," advanced mindfulness practices are not just helpful; they are often the cornerstone of treatment.
The key is to apply mindfulness not just to thoughts, but to the emotional and sensory substrate of the obsession. An intrusive thought like "What if I'm a bad person?" triggers a tsunami of feeling: a clenching in the chest, a sinking stomach, a wave of heat. The mental ritual is an attempt to escape these unbearable sensations.
Advanced Practice: Mindful Exposure to Sensation
This practice of interoceptive exposure (exposure to internal sensations) accomplishes two things: It breaks the automatic link between thought and mental compulsion by redirecting attention to the body, and it teaches emotional tolerance. You learn that the anxiety is not a monolithic block of doom, but a collection of transient physical sensations. By staying present with them, you deprive the mental ritual of its job, and the obsessive cycle weakens.
Similarly, mindfulness can be applied directly to urges. The urge to perform a compulsion is not a command; it is a feeling of intense pressure or "wrongness" that peaks and falls. You can practice "urge surfing":
These advanced skills turn your own awareness into the most precise tool for dismantling even the most hidden forms of OCD. For more resources on developing this kind of mindful awareness, our blog offers a variety of guided approaches.
OCD compulsions are, at their core, deeply ingrained maladaptive habits. They are automatic behaviors triggered by specific cues (obsessions or general anxiety) and reinforced by the immediate (though temporary) relief they provide. Understanding this through the lens of habit science provides another powerful framework for change, complementing ERP.
The Habit Loop (Cue -> Routine -> Reward):
ERP works by preventing the Routine, which eventually dismantles the loop. Habit Reversal Training (HRT) adds another layer by focusing on creating a competing, healthier response.
Behavioral Activation (BA) is a related strategy that addresses the broader behavioral withdrawal OCD causes. When consumed by obsessions and rituals, people often stop engaging in pleasurable or meaningful activities—they cancel plans, stop hobbies, avoid work. This withdrawal leads to depression, which in turn lowers energy and increases vulnerability to OCD. BA is the systematic scheduling of value-based activities regardless of mood. The principle is "action before motivation." By forcing yourself to go for a walk, call a friend, or work on a project while having OCD thoughts, you accomplish two things: you break the cycle of avoidance, and you generate natural, healthy rewards (enjoyment, mastery, connection) that compete with the false "reward" of the compulsion. This proactive rebuilding of your life is a powerful form of exposure and habit reversal in itself.
The emerging field of nutritional psychiatry provides compelling evidence that diet is not just about physical health, but a direct modulator of brain function and mental health. The gut-brain axis—a bidirectional communication network linking the enteric nervous system in the gut with the central nervous system—plays a significant role in inflammation, neurotransmitter production, and stress response. For OCD, this opens up a tangible avenue for adjunctive support.
Key Nutritional Considerations for OCD:
Important Caveat: Diet is a supportive tool, not a cure. It should never replace evidence-based therapy. Furthermore, be wary of developing "health OCD" or orthorexic tendencies around food. The goal is nourishment, not perfection. Working with a functional medicine doctor or registered dietitian knowledgeable in mental health can help create a personalized, non-stressful plan. For those interested in tracking how dietary changes might affect their physiological stress markers, the Oxyzen ring can provide fascinating objective data—a topic you can explore further on our homepage.
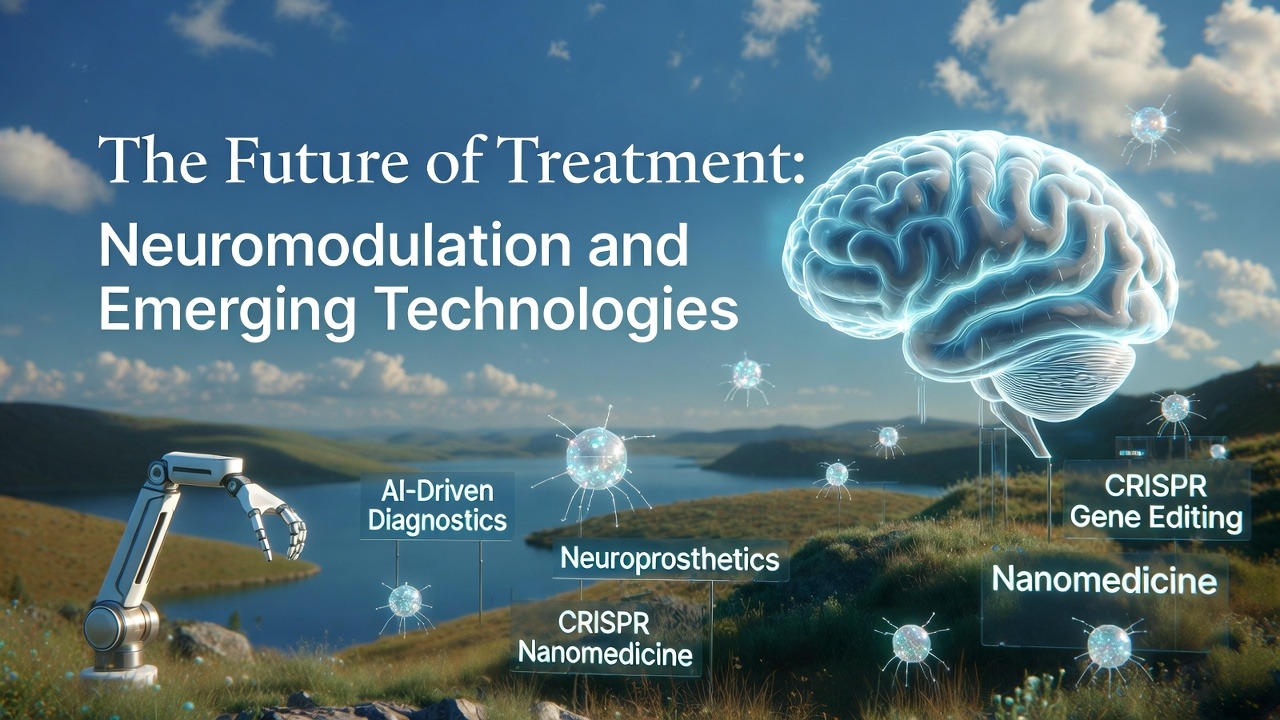
For individuals with severe, treatment-resistant OCD, the future holds promising advances that go beyond medication and talk therapy. These interventions, known as neuromodulation, directly target the dysfunctional brain circuits identified in OCD, offering hope where traditional methods have faltered.
Deep Brain Stimulation (DBS): A surgical treatment where electrodes are implanted in specific brain targets (often the ventral capsule/ventral striatum or the subthalamic nucleus). A pacemaker-like device delivers continuous electrical stimulation to modulate the overactive OCD circuit. DBS is reserved for the most severe, debilitating, and treatment-resistant cases and requires a multidisciplinary team for evaluation and management. Results can be dramatic, with some patients achieving a 50-60% reduction in symptoms.
Transcranial Magnetic Stimulation (TMS): A non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. The FDA has cleared a specific TMS protocol for OCD, targeting the anterior cingulate cortex and medial prefrontal cortex. A coil is placed against the scalp, delivering repetitive magnetic pulses (rTMS) over several weeks. It is an outpatient procedure with minimal side effects (mostly mild headache or scalp discomfort). While not as potent as DBS, it offers a valuable intermediate option.
Emerging Tech & Digital Therapeutics: This is where personal wellness technology and clinical treatment begin to converge.
These advanced treatments underscore a vital truth: OCD is a brain-based disorder, and its most stubborn forms may require brain-based solutions. The landscape of hope is continually expanding, driven by neuroscience and technology.
With this wealth of information on strategies from therapy and medication to mindfulness and technology, the final—and most important—step is synthesis. A scattered approach yields scattered results. You need a Personalized OCD Management Plan, a living document that integrates the tools relevant to you into a coherent, daily practice. This plan is your blueprint for resilience.
Steps to Create Your Plan:
This plan turns abstract concepts into concrete actions. It moves you from being passive—"I hope I feel better"—to being active: "At 8 AM, I will meditate. At 3 PM, I will practice my exposure. This evening, I will review my biometric data." This sense of agency is the ultimate antidote to the helplessness OCD breeds. For guidance on integrating a wellness device into such a structured plan, our FAQ page can be a helpful starting point.
A pivotal moment in recovery arrives when the primary goal shifts from reducing symptoms to building a life worth living. This is the essence of values-driven action, a core tenet of Acceptance and Commitment Therapy (ACT). OCD operates as a value thief; it demands your time, energy, and attention, pulling you away from the people, activities, and principles that give your life meaning. True freedom is not the absence of intrusive thoughts—it’s the reclamation of your values as the compass for your actions, irrespective of the mental noise.
Identifying Your North Star: Values are not goals; they are ongoing directions, like "heading west." A goal is to reach a specific city; the value is the journey of exploration itself. To disentangle from OCD, you must first clarify what it has been stealing from you. Ask yourself:
Common value domains include: Family, Intimate Relationships, Friendship, Career, Education/Personal Growth, Health, Spirituality, Citizenship/Community Service, and Recreation.
Committed Action in the Presence of OCD: This is the active practice of living your values while having obsessive thoughts. It is the ultimate exposure.
Each value-based action, taken in the presence of anxiety, serves a dual purpose: it enriches your life and it weakens OCD’s dictatorial power. It proves to your brain that you can have the thought and do the meaningful thing. This process is beautifully supported by tools that provide objective feedback on your progress; you can discover how Oxyzen works to show the physiological calm that can coexist with purposeful action.
Recovery is not a linear ascent to a symptom-free plateau. It is a journey through varied terrain, with inevitable stretches of rough trail. A "relapse"—or more accurately, a symptom exacerbation—is not a failure but a predictable part of the chronic condition management process, much like a flare-up of asthma or arthritis. The goal is not to avoid all flare-ups, but to have a plan to navigate them effectively and shorten their duration.
Building an Early Warning System: The most powerful relapse prevention tool is awareness of your personal precursors. These are subtle shifts that often occur before a major spike in symptoms:
Your Relapse Response Plan (RRP): Create a written, step-by-step guide for yourself when you notice warning signs.
By depersonalizing the relapse and seeing it as a logistical problem to be managed with your toolkit, you remove the shame and paralysis that can turn a brief flare-up into a prolonged setback. For ongoing support and community stories that normalize this process, you can explore related articles on our blog.
While self-help strategies are powerful, there are clear indicators that professional intervention is necessary. Seeking help is a sign of strength and a proactive step toward reclaiming your life. Consider reaching out to a therapist specializing in OCD (look for training in ERP, ACT, or I-CBT) if you experience any of the following:
Starting therapy can feel daunting. A good first step is to contact organizations like the International OCD Foundation (IOCDF), which maintains a directory of trained therapists. When you contact a therapist, ask about their specific experience with OCD and their treatment approach. Remember, you are hiring them for their expertise; it’s okay to ask questions to ensure a good fit. For those who wonder about the integration of technology with professional care, our about page details our commitment to this holistic approach.
OCD doesn't exist in a vacuum; it profoundly impacts relationships. It can strain partnerships, frustrate family members, and create loneliness. Navigating this terrain requires education, communication, and boundary-setting from both the individual with OCD and their loved ones.
For the Person with OCD:
For Loved Ones:
Intimacy: Sexual obsessions can be particularly distressing in the context of a relationship. It is vital to understand that these thoughts are not reflections of true desire or character. With the guidance of a therapist, couples can work on rebuilding intimacy through gradual, pressure-free exposure and a focus on emotional connection, separating the experience of closeness from the OCD-driven mental noise. This journey of connection, for many, is supported by tools that foster self-awareness; reading real user experiences and testimonials can provide hope and relatable context.
The demands of performance and social evaluation in work and school can be potent triggers for OCD. Perfectionism, fear of mistakes (harm obsessions), and concerns about contamination in shared spaces can make these environments feel like minefields. Strategic management is key to thriving.
Disclosure and Accommodations: This is a personal choice. You are not legally required to disclose a mental health condition unless you are requesting accommodations under the Americans with Disabilities Act (ADA) or similar laws.
Effective Workplace/Academic Strategies:
The goal is to transform the environment from a trigger zone into a practicing ground for your recovery skills, ultimately enhancing your competence and confidence.
For many, the journey with OCD raises profound existential questions: "Why me? What does this mean? Is there a purpose to this suffering?" Engaging with these questions through a spiritual or philosophical lens—whether within an organized religion, personal spirituality, or secular humanism—can be a profound source of strength and post-traumatic growth.
Reconciling OCD with Religious Faith: Scrupulosity, or religious OCD, can be especially agonizing. It hijacks sacred beliefs and turns them into sources of terror. Working with a therapist who understands both OCD and your faith tradition is crucial. Theologians often clarify that OCD-driven doubt is not a failure of faith, but a medical condition. The goal is to move from a fear-based, punitive relationship with the divine to one based on love, grace, and acceptance—concepts that are the antithesis of OCD’s rigidity.
Finding Meaning in the Struggle: Post-traumatic growth refers to positive psychological change experienced as a result of the struggle with highly challenging life circumstances. Individuals who navigate OCD often report:
Your struggle with OCD can become a crucible that forges unparalleled resilience, empathy, and wisdom. It can become a part of your story, not the definition of it. This journey of finding light in the struggle is central to our brand's own story of vision and values.
The path of managing OCD and reducing anxiety is not a straight line from illness to wellness. It is a spiral journey toward integration and wholeness. You are not trying to excise a part of yourself, but to heal the relationship between all parts: the anxious brain, the observing mind, the feeling heart, and the active body.
This journey requires courage—the courage to face feared thoughts, to tolerate uncertainty, to be vulnerable with loved ones, and to treat yourself with a kindness that OCD would deny you. It is built on the consistent application of evidence-based tools: the behavioral power of ERP, the psychological flexibility of ACT, the grounding force of mindfulness, the stabilizing support of lifestyle and sometimes medication, and the illuminating feedback of modern technology.
Remember, progress is measured not by the absence of intrusive thoughts, but by your changing response to them. It is measured in the seconds you delay a compulsion, the values you live out loud, the moments of peace you notice and savor, and the life you rebuild brick by brick outside OCD's walls.
You have within you, and available to you, everything needed to navigate this storm. You are not your OCD. You are a person of profound strength and capacity, learning to hold your own inner experience with compassion while stepping boldly into a life of your own choosing. The calm is not just a destination at the end of the journey; it is the space you create within yourself, moment by mindful moment, choice by brave choice, as you travel.
For continued support, resources, and community on this path, remember that you are not alone. Explore our blog for more wellness tips, and know that tools like the Oxyzen ring are designed to be companions in your pursuit of a measured, aware, and resilient life. Your journey continues, and each step forward is a victory.
Your Trusted Sleep Advocate (Sleep Foundation — https://www.sleepfoundation.org/)
Discover a digital archive of scholarly articles (NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature (PubMed — https://pubmed.ncbi.nlm.nih.gov/)
experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/)
Every life deserves world class care (Cleveland Clinic -
https://my.clevelandclinic.org/health)
Wearable technology and the future of predictive health monitoring. (MIT Technology Review — https://www.technologyreview.com/)
Dedicated to the well-being of all people and guided by science (World Health Organization — https://www.who.int/news-room/)
Psychological science and knowledge to benefit society and improve lives. (APA — https://www.apa.org/monitor/)
Cutting-edge insights on human longevity and peak performance
(Lifespan Research — https://www.lifespan.io/)
Global authority on exercise physiology, sports performance, and human recovery
(American College of Sports Medicine — https://www.acsm.org/)
Neuroscience-driven guidance for better focus, sleep, and mental clarity
(Stanford Human Performance Lab — https://humanperformance.stanford.edu/)
Evidence-based psychology and mind–body wellness resources
(Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/)
Data-backed research on emotional wellbeing, stress biology, and resilience
(American Institute of Stress — https://www.stress.org/)