The Hormonal Influences on Emotional Balance (Beyond Just Cortisol)
HSPs need strategies like managing sensory input, ensuring adequate downtime, and practicing self-compassion for their deep emotional processing.
HSPs need strategies like managing sensory input, ensuring adequate downtime, and practicing self-compassion for their deep emotional processing.
Think of your last emotional rollercoaster. That sudden flare of irritation over a misplaced key. The wave of inexplicable sadness on a sunny afternoon. The anxious knot in your stomach before a routine meeting. For decades, we’ve pointed a singular finger at the usual suspect: cortisol, the "stress hormone." While cortisol is a crucial player, this story is far richer, more complex, and more beautifully orchestrated than a single-note narrative.
Our emotional landscape is not a barren field governed by one weather system. It is a lush, dynamic ecosystem, meticulously tended by a symphony of chemical messengers—our hormones. These molecules course through our bloodstream, whispering instructions to our brain, our heart, our gut, and every cell in between. They are the invisible conductors of mood, motivation, focus, desire, and resilience. To understand emotional balance—true, sustained equilibrium—we must move beyond cortisol and listen to the entire hormonal orchestra.
From the ebb and flow of estrogen and progesterone dictating the nuanced tides of mood throughout a menstrual cycle, to testosterone’s underappreciated role in confidence and calm. From thyroid hormones setting the metabolic and emotional tempo of our entire body, to the gut-derived serotonin that reminds us we are truly a "second brain." This is a story of interconnected systems, where a dip in one hormone can send ripples through our entire emotional pond.
In this exploration, we will dismantle the myth of the monolithic stress hormone and embark on a journey through the endocrine system. We’ll uncover how these powerful chemicals shape our daily experiences, why "feeling off" is often a hormonal clue, and how modern technology, like advanced wellness wearables from pioneers like Oxyzen, is giving us unprecedented insight into this invisible symphony. The goal is not just knowledge, but empowerment: to equip you with the understanding needed to interpret your body’s signals and cultivate a profound, hormonally-supported emotional balance.

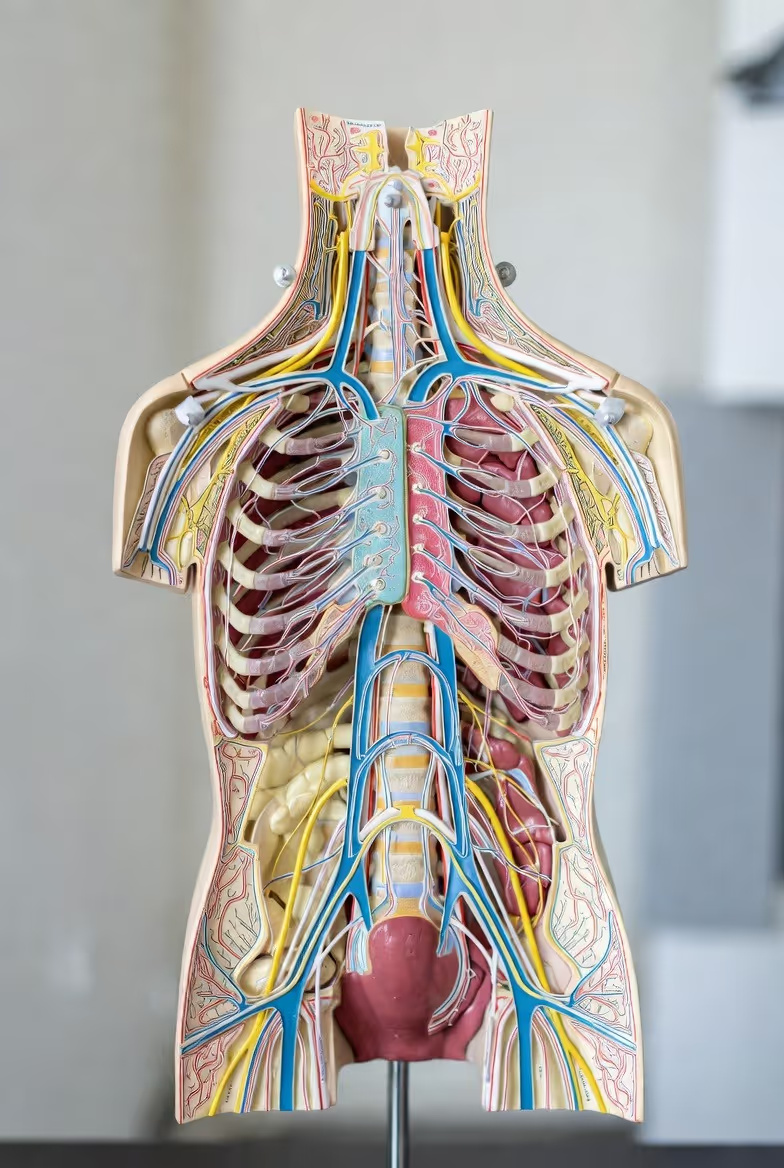
Before we meet the individual players, we must understand the stage and the conductor. The endocrine system is a network of glands and organs that produce, store, and secrete hormones. Unlike the nervous system's lightning-fast electrical signals, the endocrine system communicates through these chemical messengers released into the bloodstream, enacting slower, longer-lasting changes. Think of it as the body's long-term strategic planning division, while the nervous system handles immediate tactics.
The maestro of this orchestra is the hypothalamus, a tiny region at the brain's base. It constantly monitors the body's status—like a chief sensor—and communicates with the pituitary gland, the so-called "master gland" dangling just below it. The pituitary then releases its own hormones, which travel to target glands (like the thyroid, adrenals, and ovaries/testes) to stimulate or inhibit their hormone production. This is a system of exquisite feedback loops. When a hormone reaches an optimal level, it signals back to the hypothalamus and pituitary to slow production, maintaining a delicate state of balance, or homeostasis.
When this balance is disrupted, our emotional world feels the tremor. It’s not merely a "chemical imbalance" in the brain; it’s often a systemic hormonal conversation that has gone awry. For instance, the adrenal glands don't just produce cortisol; they also make dehydroepiandrosterone (DHEA), a precursor to sex hormones and a crucial buffer against stress. An imbalance here can affect energy, anxiety, and resilience.
Similarly, the pancreas releases insulin, a hormone whose dysregulation can lead to blood sugar rollercoasters, directly causing mood swings, irritability, and brain fog. The pineal gland secretes melatonin, governing our sleep-wake cycle, and poor sleep is a notorious saboteur of emotional stability.
This interconnectedness is key. You cannot separate thyroid function from menstrual cycle health, or gut health from stress response. They are all parts of a whole. For those seeking to track these complex biological rhythms, modern tools have evolved beyond simple step counters. Companies like Oxyzen are at the forefront, developing technology that goes deeper. You can discover how Oxyzen works to provide insights into these physiological patterns, helping you see the correlations between your body’s data and your emotional state.
Understanding this orchestra is the first step toward harmony. It shifts the question from "Why am I so anxious?" to "What is my endocrine system trying to tell me about my current state of balance?"
Cortisol has dominated the stress conversation for good reason. In acute doses, it’s life-saving—sharpening focus, mobilizing energy, and preparing us for "fight or flight." However, chronic elevation of cortisol is corrosive, linked to anxiety, depression, weight gain, and immune suppression. But cortisol is only one side of the adrenal coin. Its often-overlooked counterpart is Dehydroepiandrosterone (DHEA).
DHEA is a steroid hormone produced primarily by the adrenal glands. It serves as a parent molecule, a precursor that the body converts into both estrogen and testosterone. But beyond its role as a precursor, DHEA has powerful direct effects, particularly on the brain and our resilience to stress. While cortisol helps you survive a threat, DHEA helps you thrive through it and recover afterward. Scientists sometimes call it an "anti-aging" or "resilience" hormone.
The Cortisol-DHEA Ratio: The True Stress Indicator
Modern endocrinology suggests it's not the absolute level of either hormone, but the ratio of cortisol to DHEA that most accurately predicts stress-related wear and tear and emotional vulnerability. A healthy, resilient system shows a balanced ratio. Under chronic stress, however, cortisol production often remains high while DHEA production dwindles—a state known as "adrenal fatigue" or, more accurately, HPA axis dysfunction.
This skewed ratio has profound emotional consequences:
Cultivating a Favorable Ratio
The goal isn't to eliminate cortisol, but to support DHEA and bring the ratio back into balance. Lifestyle interventions are key:
Tracking your body’s response to these interventions can be transformative. Wondering how your daily habits are affecting your underlying physiology? Reading real customer reviews and user experiences can illuminate how others have used detailed biometric feedback to make meaningful changes to their stress management routines.

For anyone who menstruates, the intimate link between hormones and emotion is a lived, monthly reality. The cyclical dance between estrogen and progesterone is perhaps the most dramatic and clear-cut example of hormones directly steering emotional states. This isn't just about "PMS"; it's about two powerful neuroactive hormones influencing neurotransmitter activity, brain connectivity, and emotional processing throughout an entire cycle.
Estrogen: The Mood and Energy Boost
Estrogen, particularly estradiol, is a potent neuromodulator. In the first half of the cycle (the follicular phase), rising estrogen levels:
Progesterone: The Calming Counterbalance
After ovulation, progesterone rises to prepare the body for a potential pregnancy. It is metabolized into allopregnanolone, a neurosteroid that acts on GABA receptors—the same receptors targeted by anti-anxiety medications like benzodiazepines.
When the Dance Becomes a Struggle: Common Imbalances
Emotional distress tied to the cycle often points to an imbalance in this dance:
Understanding this internal rhythm allows for profound self-compassion and targeted intervention. Tracking physical signs (basal body temperature, cervical fluid) alongside mood and energy can reveal personal patterns. For a deeper dive into how hormonal phases affect sleep and recovery metrics, explore our blog for more wellness tips on cyclical living. By syncing with, not fighting against, this tide, we can navigate our emotions with greater wisdom and grace.
Testosterone is often boxed into narrow categories: the hormone of male sexuality, aggression, and muscle mass. This reductionist view overlooks its critical, nuanced role in emotional balance for all genders. In optimal levels, testosterone is less about aggression and more about assertion, confidence, motivation, and a foundational sense of well-being and calm.
The Emotional Portfolio of Testosterone
In the brain, testosterone influences areas involved in mood regulation, risk assessment, and reward. Its emotional effects include:
Low Testosterone: An Overlooked Contributor to Mood Disorders
While a natural, gradual decline occurs with age, precipitous or premature drops can wreak havoc on emotional health. Causes include chronic stress (which diverts cholesterol away from sex hormone production), poor sleep, nutrient deficiencies (especially zinc and vitamin D), obesity, and environmental toxins.
Symptoms of Low Testosterone Can Include:
Supporting Healthy Testosterone Levels Naturally
Unlike the menstrual cycle, testosterone rhythms in men follow a circadian pattern, peaking in the morning and declining through the day. Disrupted sleep or circadian misalignment can directly impair its production.
For individuals tracking their holistic health, understanding these subtle hormonal influences is key. The Oxyzen smart ring is designed to capture the physiological outputs of these hormonal states—like sleep quality, heart rate variability (a marker of stress and recovery), and body temperature trends—offering actionable insights into your overall endocrine harmony.
If hormones were a household, the thyroid gland would be the metabolic and energetic thermostat. Situated in the neck, it produces thyroxine (T4) and the more active triiodothyronine (T3). These hormones set the metabolic rate for every single cell in your body, dictating how quickly you convert food and oxygen into energy. It’s no surprise, then, that when this thermostat malfunctions, our emotional and energetic world is thrown into disarray. Thyroid dysfunction is a master masquerader, often misdiagnosed as depression or anxiety.
Hyperthyroidism: The Overheated Engine
An overactive thyroid floods the system with excess hormones, speeding up all bodily processes.
Hypothyroidism: The Slow Burn
An underactive thyroid is far more common, especially among women. The body’s processes slow to a crawl.
The Crucial Role of Conversion and Autoimmunity
The story is often more complex than simply "high" or "low." The body must convert the storage hormone T4 into the active T3. Factors like chronic stress, nutrient deficiencies (selenium, zinc, iron), gut inflammation, and environmental toxins can impair this conversion, leading to a functional deficit of T3 even if TSH (Thyroid Stimulating Hormone) levels appear "normal."
Furthermore, the most common cause of hypothyroidism in the developed world is Hashimoto's thyroiditis, an autoimmune condition where the body’s immune system attacks the thyroid gland. This creates a fluctuating, often deteriorating function and is strongly linked to gut health and systemic inflammation, which themselves are powerful drivers of mood disorders.
Nurturing Thyroid Health for Emotional Stability
Supporting the thyroid is a cornerstone of emotional balance for many.
Understanding your body’s unique rhythms, including its temperature regulation (a key thyroid output), can provide early clues. Advanced wearable technology, like that developed by Oxyzen, can track these subtle biometrics. To learn more about the science behind this holistic tracking, you can read our complete guide on interpreting your body's data for better health.
Here is a paradigm-shifting fact: Over 90% of your body's serotonin is produced not in the brain, but in your gastrointestinal tract. Serotonin, that famed "happy chemical," is primarily a gut hormone. This revelation is at the heart of the gut-brain axis, a bidirectional superhighway of communication where the gut microbiome directly dialogues with the brain via the vagus nerve, hormones, and immune messengers.
Serotonin’s Dual Citizenship
While brain serotonin regulates mood, sleep, appetite, and cognition, gut serotonin has different, but equally vital, jobs: it governs intestinal motility, modulates the immune response in the gut, and even influences bone metabolism. However, this gut-derived serotonin is a critical player in emotional health because it:
When the Gut Goes Rogue: Dysbiosis and "Leaky Gut"
An unhealthy gut microbiome, often caused by a poor diet, chronic stress, antibiotics, or infections, can lead to:
Cultivating a Serotonin-Supportive Gut
Emotional health truly begins in the gut.
The journey to optimal gut health is personal and requires tuning into your body’s signals. For those navigating this path, understanding the company behind tools that aid this journey can be helpful. You can learn more about the mission and values of Oxyzen, a company dedicated to empowering individuals with the data to connect lifestyle choices with physiological outcomes like those influenced by gut health.
In our 24/7 world, sleep is often the first sacrifice at the altar of productivity. Yet, the hormone that governs it, melatonin, is a linchpin of emotional balance and neurological repair. Secreted by the pineal gland in response to darkness, melatonin does far more than make you sleepy. It is a powerful chronobiotic (synchronizer of circadian rhythms) and a potent antioxidant, and its rhythmic release is foundational for emotional stability.
Melatonin’s Mood-Mending Functions
The Consequences of Melatonin Disruption
Optimizing Your Melatonin Rhythm for Emotional Resilience
You cannot supplement your way out of poor sleep hygiene. The goal is to support your body’s natural production.
Tracking your sleep objectively is the first step to improving it. Simple wearables have evolved; the Oxyzen smart ring, for instance, is designed to monitor sleep stages, nighttime movement, and even peripheral body temperature—a key proxy for circadian rhythm timing—giving you a clear picture of your sleep architecture and how to optimize it for emotional repair.

If cortisol is the hormone of "fight or flight," then oxytocin is the hormone of "tend and befriend." Synthesized in the hypothalamus and released by the pituitary gland, this neuropeptide has earned its nickname as the "love hormone" or "cuddle chemical," but its role in emotional balance is far more profound than romantic sentiment. Oxytocin is the biochemical substrate of connection, trust, and safety, and it acts as a powerful physiological antidote to stress.
Oxytocin: The Physiological Antidote to Cortisol
During moments of positive social connection—a hug, a meaningful conversation, playing with a pet, even sharing a meal—oxytocin is released. Its effects create a positive feedback loop for emotional well-being:
The Oxytocin Deficit: Loneliness and Hypervigilance
In an age of digital connection and social fragmentation, an oxytocin deficit is a real concern. Chronic loneliness and social isolation are associated with lower oxytocin levels, creating a vicious cycle: lack of connection reduces oxytocin, which increases social anxiety and makes future connection feel more difficult. This state keeps the nervous system in a subtle but persistent state of threat vigilance, eroding emotional resilience.
Cultivating Oxytocin in Daily Life
The beautiful thing about oxytocin is that it’s triggered by simple, accessible actions:
Understanding and prioritizing these micro-moments of connection is not a luxury; it’s a non-negotiable pillar of hormonal and emotional health. For a community that values this holistic approach to well-being, you can explore the brand journey and vision of companies that build technology to support, not replace, these essential human connections.
Our relationship with food is deeply emotional, and the hormones that regulate hunger and satiety are direct players in this dynamic. Leptin and ghrelin are often described in simple terms: ghrelin is the "hunger hormone" that signals an empty stomach, and leptin is the "satiety hormone" released from fat cells to signal fullness. However, their influence extends deep into the brain's emotional and reward centers, impacting mood, energy, and even symptoms of depression and anxiety.
Leptin: The Satiety Signal with a Mood Connection
Produced primarily by adipose (fat) tissue, leptin’s job is to communicate energy sufficiency to the hypothalamus. But leptin receptors are also found in brain regions involved in mood regulation.
Ghrelin: The Hunger Hormone with an Anxiolytic Twist
Secreted by the stomach when empty, ghrelin stimulates appetite. But intriguingly, ghrelin also has anti-depressant and anti-anxiety effects in animal studies. It appears to boost dopamine activity in reward pathways and may help the brain cope with stress. This creates a complex picture: the hormone that makes us seek food also seems to provide a short-term mood buffer, which may explain the emotional pull of "comfort food" during times of stress, even when we're not physically hungry.
The Blood Sugar Rollercoaster’s Emotional Toll
While not a hormone itself, blood sugar stability is governed by insulin and directly impacts the hunger hormones. A diet high in refined sugars and carbohydrates leads to rapid spikes and crashes in blood glucose. This rollercoaster causes corresponding spikes and crashes in energy and mood, leading to irritability, anxiety, brain fog ("hanger"), and intense cravings—driven in part by ghrelin—for more quick-energy food, perpetuating the cycle.
Stabilizing the System for Emotional Balance
Tuning into your body’s true hunger and satiety signals, rather than emotional cues, is a skill. For support and answers to common questions on using data to understand your body's unique rhythms, you can always visit our comprehensive FAQ and support page.
Perhaps the most revolutionary understanding in modern psychiatry and endocrinology is the role of inflammation as a direct driver of mood disorders. We’ve moved beyond seeing the brain as an isolated organ; we now understand it is in constant, dynamic conversation with the immune system. The messengers in this conversation are cytokines—small proteins released by immune cells that signal inflammation. When this system becomes chronically activated, it can fundamentally alter brain chemistry and function, leading to a state often termed "sickness behavior" that mirrors depression.
From Peripheral Inflammation to Brain Fog and Gloom
When your body is fighting an infection, dealing with gut permeability, or carrying excess visceral fat (an active endocrine organ that secretes pro-inflammatory cytokines), systemic inflammation rises. These inflammatory cytokines can:
Emotional Symptoms of a "Inflamed Brain" (Neuroinflammation)
This isn't about feeling "a bit off." It can manifest as:
Sources of Chronic, Mood-Disrupting Inflammation
Calming the Fire for a Calmer Mind
An anti-inflammatory lifestyle is a direct strategy for emotional health.
Connecting daily choices to internal states like inflammation requires seeing the unseen. The data from a comprehensive wellness tracker can reveal patterns—how poor sleep one night correlates with lower heart rate variability (a marker of stress/inflammation) the next day. To see how others have made these connections, explore real customer reviews and experiences with in-depth health tracking.
We typically think of insulin in the context of blood sugar and diabetes. However, this pancreatic hormone is a master regulator of metabolism with profound and direct effects on brain function and emotional health. The brain is a glucose-hungry organ, and insulin is the key that allows glucose to enter cells for energy. But insulin’s role in the brain extends far beyond fueling neurons; it acts as a neuroactive hormone that influences neurotransmitter activity, synaptic plasticity, and inflammation.
Insulin Resistance: When the Brain Starves in a Sea of Sugar
Insulin resistance is a condition where cells throughout the body—including, critically, brain cells—become less responsive to insulin's "open up for glucose" signal. This is often driven by a diet high in refined carbohydrates and sugars, chronic stress, and inactivity. The pancreas compensates by pumping out more and more insulin, leading to hyperinsulinemia (high insulin levels).
This metabolic dysfunction has devastating consequences for emotional balance:
The Emotional Profile of Insulin Dysregulation
Mood symptoms are often the first sign of insulin resistance, appearing long before a diagnosis of prediabetes. These can include:
Re-Sensitizing the Brain: Diet and Lifestyle as Medicine
The good news is that insulin resistance is largely reversible through lifestyle.
Understanding your body’s unique metabolic responses is key. Tracking biomarkers like fasting glucose (and ideally, insulin) with your doctor, and observing how your energy and mood respond to different foods, is crucial. For a deeper exploration of the science behind metabolic health and wearable technology, be sure to explore our blog for more wellness tips. This knowledge empowers you to make food choices that fuel both your body and your emotional resilience.
Often categorized merely as a vitamin, Vitamin D is, in fact, a potent secosteroid hormone. It is synthesized in the skin from sunlight exposure and undergoes activation in the liver and kidneys. While its role in bone health is well-known, its function as a neuroactive hormone is critical for emotional balance. Receptors for vitamin D are found throughout the brain, particularly in areas linked to mood regulation, such as the prefrontal cortex and hippocampus. Its deficiency is now recognized as a significant, yet modifiable, risk factor for depression, seasonal affective disorder (SAD), and anxiety.
Vitamin D’s Mood-Modulating Mechanisms
This "sunshine hormone" operates on multiple levels to support emotional well-being:
The Modern Epidemic of Deficiency and Its Emotional Toll
Despite its name, it is challenging to get sufficient vitamin D from diet alone (fatty fish, egg yolks, fortified foods). The primary source is sun exposure, which is limited by modern indoor lifestyles, use of sunscreen, geographical location, and seasonal changes.
Optimizing Vitamin D for Emotional Resilience
As with all hormones, balance is key. While deficiency is harmful, megadoses can also have negative consequences. The goal is sufficiency, not excess. For individuals using comprehensive wellness trackers, observing correlations between mood scores, energy levels, and even sleep quality across different seasons can provide personal insight into one’s sensitivity to this light-dependent hormone, a fascinating data point explored in many resources on the Oxyzen blog.
While often discussed in the context of athletic performance and aging, Human Growth Hormone (HGH) and its primary mediator, Insulin-like Growth Factor-1 (IGF-1), are vital for brain health and emotional equilibrium. Released in pulses from the pituitary gland, primarily during deep, slow-wave sleep, this hormonal axis is responsible for cellular repair, growth, and regeneration throughout the body—including the brain.
The Brain’s Maintenance Crew
HGH stimulates the liver to produce IGF-1, which then crosses the blood-brain barrier. Their roles in the nervous system are profound:
The Decline and Disruption of the Growth Axis
Production of HGH/IGF-1 naturally declines with age, but lifestyle factors can cause a premature or precipitous drop:
Supporting Natural HGH/IGF-1 Production
Pharmacologic HGH is controversial and reserved for specific medical diagnoses. The focus for emotional health should be on supporting the body’s natural production.
The profound link between deep sleep and this repair axis highlights why simply tracking "hours in bed" is insufficient. Understanding your sleep architecture—how much time you spend in each restorative stage—is key. Advanced wearables like the Oxyzen ring are designed to provide this precise analysis, helping you connect the dots between your lifestyle, your sleep quality, and your body’s innate repair processes. You can discover how Oxyzen works to uncover these vital patterns.
Dopamine is frequently mislabeled as the "pleasure hormone." A more accurate description is the "motivation, reward, and anticipation molecule." It is the core driver of our "seek and pursue" behavior, fueling desire, focus, goal-directed action, and the feeling that our efforts are worthwhile. Its balance is exquisite—too little leads to apathy and anhedonia; too much, or dysregulated signaling, is linked to anxiety, addiction, and psychosis.
Dopamine’s Role in Emotional Drive
Dopaminergic pathways, particularly the mesolimbic pathway, are central to how we experience motivation and satisfaction.
Dopamine Dysregulation: Two Sides of the Same Coin
Supporting Healthy Dopamine Tone Naturally
The goal is not to spike dopamine artificially, but to support its natural, rhythmic production and receptor sensitivity.
Understanding your own motivational patterns and energy cycles is a form of self-awareness that can be enhanced by data. Tracking your daily activity, sleep, and recovery metrics can help you identify the times of day you are naturally most focused and driven, allowing you to schedule demanding tasks accordingly. For more on structuring your day for optimal performance, the Oxyzen blog offers a wealth of related insights.
While not a hormone in the classic endocrine sense, Gamma-Aminobutyric Acid (GABA) is the primary inhibitory neurotransmitter in the central nervous system. Its function is paramount to emotional balance: it acts as the brain’s "brake pedal," slowing down neural activity, promoting relaxation, reducing neuronal excitability, and quieting the "noise." Where cortisol, norepinephrine, and glutamate (the main excitatory neurotransmitter) accelerate, GABA applies the brakes. An imbalance in this system is at the heart of many anxiety disorders, insomnia, and even seizures.
GABA’s Role in Quieting the Mind and Body
GABA Deficiency and Dysfunction
Low GABA activity is strongly linked to:
It’s important to note that oral GABA supplements are controversial, as it’s unclear how well they cross the blood-brain barrier. The more effective strategy is to support the body’s own production and the sensitivity of GABA receptors.
Natural Strategies to Enhance GABAergic Tone
The ability to track your physiological state of calm—through metrics like Heart Rate Variability (HRV)—provides direct feedback on your nervous system's balance between "gas" (sympathetic) and "brake" (parasympathetic, which is GABA-influenced). A higher HRV generally indicates a more resilient, flexible system capable of calming down effectively. Seeing this data can motivate and guide relaxation practices. To understand how this technology fits into a holistic wellness vision, you can learn more about the company’s mission and values.
We’ve explored serotonin’s gut connection, but the enteric nervous system—the "second brain" in your gut—produces a vast array of other hormones that directly signal the brain. Two key players are Peptide YY (PYY) and Glucagon-like Peptide-1 (GLP-1). Released from intestinal cells in response to food, especially protein and fat, these hormones do far more than regulate digestion and appetite; they are potent modulators of stress, anxiety, and reward.
Peptide YY (PYY): The Satiety Hormone with Anxiolytic Effects
PYY is released after eating and works to slow gastric emptying and promote a lasting feeling of fullness. New research reveals a fascinating brain-gut connection:
Glucagon-like Peptide-1 (GLP-1): Beyond Blood Sugar Control
GLP-1 is famous for its role in stimulating insulin release and inhibiting glucagon, making it a target for diabetes and weight loss drugs. Its emotional effects are profound:
The Gut-Brain Dialogue in Real Time
This means the composition of your meal directly influences the hormonal messages sent to your brain. A meal high in processed carbohydrates that causes a rapid blood sugar spike and crash will send very different signals (involving insulin and subsequent hunger hormones) than a balanced meal with protein, fat, and fiber that stimulates a sustained, calming release of PYY and GLP-1.
Feeding Your Gut for a Calmer Brain
Tuning into how you feel after meals—not just physically, but emotionally—is a powerful practice. Do you feel energized and focused, or sluggish and irritable? This biofeedback is your gut-brain axis speaking. For those navigating dietary changes and seeking community support, reading real customer reviews and experiences can provide relatable insights and motivation.
Norepinephrine (or noradrenaline) is both a neurotransmitter and a hormone. Released from the adrenal glands into the bloodstream and from neurons in the brainstem's locus coeruleus, it is the body’s primary chemical for alertness, arousal, focus, and vigilance. It prepares the mind and body for action. In a balanced amount, it is essential for motivation, attention, and responding to challenges. However, like all potent molecules, its dysregulation is central to several mood and anxiety disorders.
The Dual Role of Norepinephrine
Norepinephrine in Emotional Balance and Imbalance
Modulating Norepinephrine for Calm Focus
The goal is not to eliminate norepinephrine, but to support its healthy, regulated release.
Tracking physiological markers of arousal, such as resting heart rate and heart rate variability, can provide objective insight into your sympathetic (norepinephrine-driven) tone. Seeing these metrics improve with consistent stress-management practices offers powerful positive reinforcement. For technical questions on how these metrics are captured and interpreted, our FAQ page is a valuable resource.
Up to this point, we have examined the individual players in the endocrine orchestra. But the true magic—and complexity—lies in their interactions. Hormones do not operate in isolation; they exist in a state of constant, dynamic conversation through feedback loops. A shift in one creates a ripple effect, altering the production, sensitivity, or function of others. This interconnected web explains why emotional imbalance is rarely about a single "deficiency" but rather a systemic pattern of dysregulation.
Key Hormonal Conversations
The Vicious Cycles of Imbalance
These interconnections often create self-perpetuating cycles:
The Systems-Thinking Approach to Emotional Health
This web affirms that the most effective approach to hormonal and emotional balance is holistic. It is futile to address only one hormone in isolation. The most powerful interventions are those that positively influence multiple systems simultaneously:
Understanding this symphony allows you to be the conductor of your own health. By making lifestyle choices that support the entire system, you create harmony. For a deeper look at the philosophy behind creating technology that honors this complexity, you can explore our story and vision. The journey toward emotional balance is about connecting the dots, and with the right knowledge and tools, you can map your unique path to harmony.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/