How Sleep Improvement Changes Your Brain Function
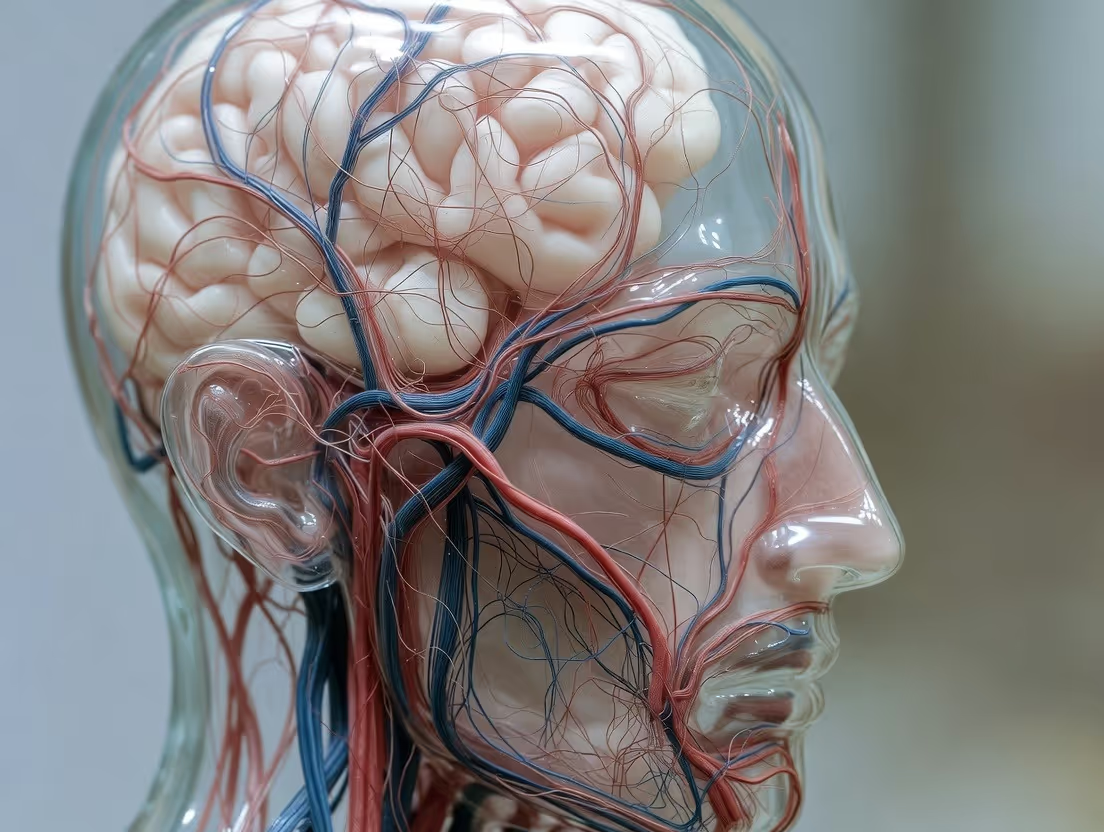
Sleep improvement enhances brain function by improving memory consolidation, clearing metabolic waste, and strengthening neural connections.
Sleep improvement enhances brain function by improving memory consolidation, clearing metabolic waste, and strengthening neural connections.
You’ve heard it a million times: “Get more sleep.” It’s advice that feels both universal and vaguely tedious, often filed away with “drink more water” and “eat your vegetables.” But what if that familiar refrain hides a truth far more profound than we’ve ever considered? What if sleep isn’t just a passive state of rest, but a dynamic, nightly neurological renovation project—one that directly architects your cognitive abilities, emotional resilience, and long-term brain health?
For decades, we viewed sleep as the brain’s offline mode. A blank space in the ledger of consciousness. Modern neuroscience, however, has shattered this misconception. We now understand that the sleeping brain is a hive of frenetic, purposeful activity. It is during these critical hours that your brain engages in a sophisticated sequence of maintenance, repair, consolidation, and purification processes that are utterly impossible during waking life. When you shortchange your sleep, you aren’t just accruing fatigue; you are actively degrading the very structure and function of your most vital organ.
This article is not another guilt trip about getting eight hours. It is a deep exploration into the tangible, biological transformations that occur inside your skull when you prioritize and improve your sleep. We will journey into the glymphatic system, your brain’s power-washer, which expands by 60% during deep sleep to flush out the toxic proteins linked to Alzheimer’s disease. We will decode how sleep stages orchestrate memory, turning fragile daily experiences into permanent knowledge. We will expose how a single night of poor sleep can rewire your emotional circuitry, making you more reactive to stress and less capable of joy.
Most importantly, we will move beyond the problem and into the solution. How can you measure, understand, and systematically upgrade your sleep to harness these brain-changing benefits? This is where data meets biology. In an era of wearable technology, tools like the advanced smart ring from Oxyzen are demystifying the black box of our sleep, offering personalized insights that go far beyond simple duration. By tracking physiological signals like heart rate variability, body temperature, and blood oxygen saturation, these devices provide a window into the quality of your sleep architecture—the true determinant of neurological repair.
The journey to a better-functioning brain begins not with a puzzle or a pill, but with the deliberate, science-backed improvement of your sleep. Let’s begin by understanding what’s really at stake when you close your eyes.

Before we can appreciate how sleep improvement changes the brain, we must first understand what “sleep” actually is. It’s not a uniform state of unconsciousness. Instead, sleep is a highly structured, cyclical process composed of distinct stages, each with a unique neurological signature and purpose. This structure is known as your sleep architecture.
Over the course of a night, your brain cycles through these stages every 90 to 110 minutes, repeating the sequence four to six times. Each cycle is like a shift in a sophisticated factory, with different teams clocking in to perform specialized tasks.
Stage 1 (N1) – The Gateway: Lasting just a few minutes, this is the lightest stage of sleep, the drift from wakefulness into slumber. Your brain waves begin to slow from their daytime patterns (beta waves) into alpha and theta waves. Muscles relax, and you can be easily awakened. Think of this as the brain’s “system initialization” phase.
Stage 2 (N2) – Foundation Building: You spend nearly 50% of your total sleep in this stage. Brain activity further slows with specific bursts of activity called sleep spindles and K-complexes. These are believed to be crucial for memory consolidation (transferring information from short-term to long-term storage) and protecting the brain from being awakened by external stimuli. It’s the brain’s way of filing away the day’s data and tuning out the outside world.
Stage 3 (N3) – Deep Sleep (Slow-Wave Sleep): This is the most physically restorative phase. Characterized by slow, powerful delta waves, this is when the body repairs tissues, builds bone and muscle, and strengthens the immune system. For the brain, this stage is critical for cognitive restoration and declarative memory consolidation (facts and figures). It’s also the prime time for the glymphatic system—the brain’s waste-clearance system—to kick into high gear. Waking from deep sleep often results in disorientation and mental fog.
REM Sleep – The Mental Theater: Rapid Eye Movement (REM) sleep is where dreaming primarily occurs. Despite the body being paralyzed (a safety feature known as atonia), the brain is as active as it is when you’re awake. This stage is essential for processing emotions, creative problem-solving, and procedural memory consolidation (skills and tasks). It’s like the brain’s overnight therapy and innovation session, where it makes sense of emotional experiences and forms novel connections.
The proportion of time spent in each stage changes throughout the night. Early cycles are rich in deep N3 sleep, while later cycles feature prolonged REM periods. This architecture is not fixed; it is dynamically responsive to your life. Learn a new language? Your brain may increase spindle activity in N2 sleep. Experience emotional trauma? REM sleep may intensify as your brain works to process it.
Why Architecture Matters More Than Just Hours: You could be in bed for 8 hours but, due to factors like stress, alcohol, an erratic schedule, or sleep apnea, get very little restorative deep or REM sleep. This is poor sleep quality, and its impact on the brain is as severe as getting only 4-5 hours of fragmented sleep. Improving sleep, therefore, isn’t just about extending time in bed; it’s about nurturing the integrity, balance, and continuity of these vital cycles.
Understanding this architecture is the first step toward taking control of it. With modern tools that track these phases—like the comprehensive sleep analysis provided by the Oxyzen smart ring—you’re no longer guessing about your sleep quality. You have a data-driven blueprint of your brain’s nightly renovation project, allowing you to make targeted lifestyle changes that enhance the most critical phases of repair and consolidation.
One of the most groundbreaking discoveries in modern neuroscience is the glymphatic system. Identified just over a decade ago, this waste-clearance network operates like a microscopic, cerebral plumbing system, and its primary shift supervisor is deep, non-REM sleep.
During waking hours, your brain is a metabolic furnace, consuming about 20% of your body’s energy. This intense activity generates metabolic waste products, including proteins like beta-amyloid and tau. In healthy brains, these proteins are efficiently cleared away. However, when they accumulate, they form the sticky plaques and toxic tangles that are the hallmarks of Alzheimer’s disease and other neurodegenerative disorders.
So, how does the brain, which is encased in a hard skull and lacks a traditional lymphatic system, take out the trash? Enter the glymphatic system. It utilizes the unique layout of the brain’s glial cells (specifically astrocytes) to create a network of periarterial channels. Cerebrospinal fluid (CSF) flushes into these channels, mixes with interstitial fluid (the fluid between brain cells), and forcefully sweeps away accumulated waste, funneling it out of the brain and into the body’s circulatory system for disposal.
The Sleep Connection: Researchers using advanced imaging discovered that the glymphatic system is most active during slow-wave deep sleep. In fact, the interstitial space in the brain expands by over 60% during this stage, effectively turning the faucet to full blast. The slow, synchronized neural activity of deep sleep appears to create the perfect pressure waves to drive this cleansing flow.
“Think of the waking brain as a bustling city during the day—producing waste, traffic, and clutter. Sleep, particularly deep sleep, is the night crew that comes in. The streets are empty, and powerful cleaning trucks can finally flush out the accumulated garbage, leaving the city fresh and functional for the next day.”
When you miss deep sleep, you directly impair this cleansing process. A single night of sleep deprivation leads to a measurable increase in beta-amyloid in the brain’s hippocampus—a region vital for memory. Chronic sleep restriction essentially means your brain is trying to function in a toxic, polluted environment. The long-term implications for cognitive decline are stark and scientifically validated.
Improving Sleep to Power the Cleanse: The direct line between sleep quality and this detoxification process makes prioritizing deep sleep one of the most proactive steps you can take for long-term brain health. Lifestyle factors that enhance deep sleep include:
Monitoring your deep sleep is no longer a mystery. Advanced wearables that track physiological markers can estimate your time in this crucial stage, giving you feedback on how your habits affect your brain’s nightly cleanse. For a deeper dive into how technology is unlocking these insights, our blog features ongoing research into sleep and neurodegeneration. This isn’t just about feeling rested tomorrow; it’s about protecting your cognitive function for decades to come.
You study for hours, rehearse a presentation, or practice a new chord on the guitar. Where does that effort go when you sleep? It doesn’t vanish; it gets engineered into the fabric of your brain. The process of converting fragile, short-term memories into stable, long-term knowledge is called memory consolidation, and sleep is its master architect.
This isn’t a passive storage process. It’s an active, selective, and highly sophisticated editing session. Sleep doesn't just save everything; it strengthens what’s important, integrates it with existing knowledge, and often discards the irrelevant noise of the day.
The Two-Step Dance of Sleep-Dependent Memory:
Different Stages for Different Memories:
The Creativity Bonus: Associative Memory
Beyond simple consolidation, sleep enhances memory integration. During REM sleep, the brain’s chemistry changes, and its connectivity patterns become more flexible. This allows it to forge novel connections between disparate pieces of information. Have you ever gone to bed with a problem and woken up with a solution? This “sleeping on it” phenomenon is real. By loosening the logical constraints of waking thought, REM sleep allows the brain to detect distant associations and arrive at creative insights and solutions that elude you during the day.
The Cost of Poor Sleep: Skimping on sleep, especially after learning something new, drastically reduces your brain’s ability to perform this consolidation. Studies show that pulling an all-nighter after studying can reduce memory retention by 40% or more. It’s not just that you’re tired; the memory trace itself is weaker because it was never properly cemented.
Improving your sleep, therefore, is a direct investment in your learning efficiency and intellectual capital. By ensuring robust sleep architecture—rich in both deep NREM and REM sleep—you turn your nights into a cognitive workshop. For anyone from students to lifelong learners to professionals seeking an edge, this is non-negotiable. To see how users leverage sleep data to optimize learning periods, the real-world testimonials at Oxyzen provide compelling narratives of improved focus and skill acquisition.
If you’ve ever felt irritable, emotionally fragile, or quick to anger after a poor night’s sleep, you’ve experienced firsthand the powerful link between sleep and emotion. This isn’t just a subjective feeling; it’s a measurable neurological phenomenon. Sleep, particularly REM sleep, acts as a nightly therapy session for the brain’s emotional centers.
The key player in this process is the amygdala, the brain’s almond-shaped alarm system for threat and fear. The prefrontal cortex (PFC), located just behind your forehead, is the brain’s executive center, responsible for rational decision-making, impulse control, and regulating the amygdala’s emotional reactions.
The REM Sleep Reset:
During REM sleep, the brain undergoes a unique neurochemical shift. Stress-related neurotransmitters like noradrenaline (norepinephrine) are virtually shut off. In this safe, low-stress chemical environment, the brain reactivates emotional memories from the day. However, it does so while simultaneously strengthening the connections between the prefrontal cortex and the amygdala. This process, sometimes called “overnight therapy,” allows the brain to process the emotional content of memories while stripping away some of their raw, visceral charge.
Think of it this way: The memory of a stressful work meeting is replayed, but without the high levels of stress chemicals, the brain can file it away as a memory of an event rather than reliving it as an ongoing threat. This is how sleep helps us gain perspective and maintain emotional equilibrium.
The Consequences of Disruption:
When REM sleep is cut short or fragmented, this recalibration process is short-circuited.
Sleep and Emotional Intelligence: Beyond just regulating negative emotions, good sleep enhances positive social and emotional functioning. It improves your ability to accurately read facial expressions, show empathy, and navigate complex social situations. A well-rested brain is a socially intelligent brain.
Improving sleep quality, with a focus on achieving sufficient, uninterrupted REM sleep, is therefore a cornerstone of mental health. It’s not an alternative to therapy or other interventions, but a foundational biological support for them. Techniques that stabilize sleep—like mindfulness, light management, and consistent routines—directly contribute to a more resilient emotional life. Understanding your personal sleep patterns is the first step; the team at Oxyzen built their technology to provide these very insights, and you can learn more about their mission to empower emotional wellness through data.

Your waking life is a constant barrage of learning, experiences, and stimuli. Every new thought, sensation, and skill forms connections between your brain’s neurons—these are called synapses. If this process of synaptic strengthening (or potentiation) continued unchecked during all waking hours, your brain would eventually become over-saturated, overloaded, and energetically bankrupt. This is where one of sleep’s most fundamental functions comes into play: Synaptic Homeostasis.
The Synaptic Homeostasis Hypothesis (SHY) proposes that a core function of sleep, particularly slow-wave deep sleep, is to downscale the overall strength of synapses that were strengthened during the day. It’s a global, intelligent reset.
How It Works:
The Benefits of the Nightly Reset:
In essence, deep sleep is the brain’s way of running a “disk defragmentation” and system cleanup. It consolidates the important files (memories) and deletes the temporary cache, ensuring the system runs smoothly, efficiently, and is ready for new input.
When the Reset Fails: Chronic sleep deprivation disrupts synaptic homeostasis. Synapses remain chronically potentiated, leading to a brain that is metabolically stressed, noisy, and inefficient. This neural “clutter” manifests as brain fog, an inability to concentrate, slower learning, and mental fatigue. Over the long term, this state of constant synaptic overload may contribute to neurodegenerative processes.
Improving your sleep, specifically by maximizing the quality and amount of deep NREM sleep, directly supports this vital reset function. It ensures your brain starts each day on a clean, efficient slate. For tech enthusiasts and biohackers, this is the ultimate cognitive optimization protocol—and it’s built into your biology. Tracking your deep sleep can show you how well this process is functioning, a key feature explored in the Oxyzen FAQ regarding the ring’s sleep stage accuracy and interpretation.
Neuroplasticity is the brain’s lifelong ability to reorganize itself by forming new neural connections. It is the physical basis for all learning, memory, and recovery from injury. While neuroplasticity occurs throughout the day, sleep is the period when these new connections are solidified, integrated, and made permanent. Improving sleep doesn’t just rest you; it directly amplifies your brain’s capacity to change and adapt.
Sleep-Dependent Synaptic Plasticity: The synaptic strengthening (long-term potentiation, or LTP) that underlies learning is initiated during waking experience. However, the stabilization and enhancement of LTP—the process that makes a temporary change permanent—is strongly sleep-dependent. During deep NREM and REM sleep, the neural patterns activated during learning are “replayed.” This replay triggers biochemical cascades that reinforce the newly formed synapses, literally cementing the change in your brain’s wiring.
The Role of Different Sleep Stages:
Practical Evidence: Skill Enhancement Overnight: Landmark studies on motor skill learning (like typing a sequence of numbers) show a clear pattern. Performance improves with practice during the day, plateaus, and then shows a significant, jump in improvement after a night of sleep—not after an equivalent period of daytime wakefulness. This “offline” enhancement is a direct product of sleep-dependent neuroplasticity. The brain is literally practicing and refining the skill while you rest.
The Impact of Sleep Improvement: By prioritizing sleep, you are:
For anyone engaged in continuous learning—whether a student, a professional mastering new software, a musician, or an athlete—optimizing sleep is the most powerful performance enhancer available. It turns passive recovery time into an active learning session. Understanding your unique sleep patterns is key to harnessing this, a principle central to the vision behind Oxyzen’s development story.
The brain is not just an electrical network; it’s a sophisticated chemical orchestra. Sleep acts as the conductor, ensuring that hormones and neurotransmitters—the chemical messengers that govern everything from mood to metabolism—are produced, released, and balanced in perfect rhythm. Disrupt sleep, and this hormonal symphony descends into chaos, with direct consequences for brain function.
Key Hormones Regulated by Sleep:
The Brain on a Hormonal Rollercoaster: When you are sleep-deprived, you are essentially sending your brain through a chemical storm. You’re stressed (high cortisol), hungry for junk food (low leptin/high ghrelin), mentally sluggish (disrupted growth hormone), and emotionally vulnerable (low serotonin). This chemical imbalance directly impairs prefrontal cortex function, emotional regulation, and metabolic support for the brain.
Restoring Balance Through Sleep Improvement: By consistently achieving high-quality, sufficient sleep, you restore the natural rhythm of these hormones. This creates a stable internal chemical environment where the brain can thrive: lower inflammation, balanced energy, effective stress management, and optimal cellular repair. It’s a foundational form of biochemical support for cognitive and emotional health. For those navigating the complexities of modern life and stress, tools that help track sleep’s impact on readiness and recovery, like those discussed on the Oxyzen blog, can be invaluable for maintaining this delicate balance.
The prefrontal cortex (PFC) is the brain’s chief executive officer. It sits behind your forehead and is responsible for executive functions: a suite of high-level cognitive skills that include focused attention, complex decision-making, problem-solving, impulse control, planning, and social conduct. It is the last brain region to mature in young adulthood and is also one of the first to show signs of decline with age or neglect. Its number one non-negotiable requirement? Sleep.
How Sleep Deprivation Sabotages the CEO:
MRI scans reveal that after even one night of poor sleep, there is a significant reduction in metabolic activity and blood flow in the PFC. Meanwhile, activity in the more primitive, emotional centers (like the amygdala) increases. This is a neurological power shift from rationality to reactivity.
The consequences are specific and debilitating:
Sleep as PFC Maintenance: Deep NREM sleep is particularly vital for restoring metabolic resources in the PFC. The slow waves are thought to help replenish cellular energy stores (like ATP) and clear out metabolic byproducts that accumulate during waking hours. Think of it as rebooting and defragging the brain’s central processing unit.
The Competitive Advantage of Sleep: In a knowledge economy, executive function is currency. Improving sleep quality directly invests in your cognitive capital. A well-rested PFC means sharper focus, better strategic thinking, more innovative problem-solving, and greater emotional intelligence in leadership. It is the ultimate productivity hack, not because you work more hours, but because your brain’s executive suite operates at peak efficiency during the hours you are awake. Learning to protect and nurture your sleep is a professional strategy, a truth echoed in many of the experiences shared by Oxyzen users who track their data for peak performance.
Beyond the macroscopic systems like the glymphatic network, sleep facilitates profound repair and maintenance at the cellular and molecular level. While you are asleep, your brain’s individual cells engage in housekeeping, damage repair, and energy restoration that are prioritized over the demands of waking activity.
Cellular Energy Restoration: The ATP Cycle
Adenosine triphosphate (ATP) is the universal currency of cellular energy. During waking hours, ATP is broken down to fuel neuronal activity, leading to a buildup of its byproduct, adenosine. This accumulating adenosine is one of the key drivers of “sleep pressure”—the feeling of sleepiness. During sleep, particularly deep sleep, the brain has the opportunity to recycle adenosine and resynthesize ATP, restoring its energy reserves. Caffeine works by blocking adenosine receptors, tricking your brain into feeling alert despite the energy debt.
DNA Repair and Protein Synthesis:
Wakefulness, with its metabolic activity and exposure to environmental stressors, causes wear and tear at the DNA level within neurons. Sleep increases the expression of genes involved in DNA repair and the synthesis of new proteins. These proteins are the building blocks for repairing cellular components, strengthening synapses, and producing neurotransmitters. Without this dedicated repair shift, cellular damage accumulates, accelerating aging and impairing function.
Mitochondrial Health:
Mitochondria are the power plants of your cells, including neurons. Sleep is crucial for mitochondrial maintenance and turnover (mitophagy). Poor sleep leads to mitochondrial dysfunction, reducing the brain’s energy output and increasing oxidative stress, a key contributor to neurodegeneration.
Anti-Inflammatory Effects:
Chronic, systemic inflammation is a known enemy of brain health, linked to depression, cognitive decline, and Alzheimer’s. Sleep has a potent anti-inflammatory effect. Deep sleep is associated with the release of anti-inflammatory cytokines and a reduction in pro-inflammatory ones. Conversely, sleep deprivation triggers a marked increase in inflammatory markers, which can directly damage brain tissue and disrupt the blood-brain barrier.
The Cumulative Impact:
This nightly shift of cellular repair is not a luxury. It is essential maintenance that prevents the accelerated degradation of your brain’s hardware. When you consistently get good sleep, you are:
Neglecting sleep is like running a factory 24/7 without ever stopping for equipment maintenance. Eventually, things break down. By improving sleep, you schedule this non-negotiable maintenance, protecting the very cellular integrity of your brain. The pursuit of longevity and lifelong cognitive vitality is deeply intertwined with this cellular cleanup, a connection we explore in our ongoing research and articles on wellness technology.
Thus far, we’ve explored the individual benefits of good sleep for the brain. But the reality for many is a self-perpetuating trap: Poor sleep leads to brain changes that make it even harder to achieve good sleep. Understanding this cycle is the key to breaking it.
The Cycle in Action:
Breaking the Cycle with Sleep Improvement Strategies:
The escape route requires deliberate, consistent action that targets multiple points in the cycle:
Breaking the cycle isn’t about perfection; it’s about consistent, positive pressure in the right direction. Every night of improved sleep begins to reverse the neurological damage, calming the amygdala, restoring the PFC, and stabilizing hormones, making the next good night easier to achieve. For those seeking guidance on starting this journey, a great resource is the Oxyzen FAQ, which addresses common questions on using data to improve sleep habits.
Understanding the science is one thing; seeing your own progress is another. How do you know your brain is actually benefiting from your efforts to improve sleep? In the past, this was guesswork. Today, we can move from anecdote to data, quantifying the neurological payoff of better sleep through both subjective feelings and objective biomarkers.
Subjective Measures (How You Feel):
Objective Biomarkers (The Data):
Modern wellness technology, particularly advanced wearables like smart rings, provides a window into the physiological correlates of brain-relevant sleep improvement:
Creating Your Baseline and Tracking Progress:
The power of this data lies in comparison. By establishing your personal baseline over a few weeks, you can then see the impact of interventions: How does cutting off caffeine after 2 PM affect your deep sleep? Does a 10-minute meditation before bed raise your HRV? Does a consistent wake time smooth your temperature curve?
This transforms sleep improvement from a vague goal into a personalized, iterative science experiment. You are no longer just “trying to sleep better”; you are measuring your brain’s specific response to lifestyle changes. This journey of discovery, of understanding one’s own biology, is at the heart of the Oxyzen story and its mission to empower individuals with actionable health intelligence.
Understanding the "why" is meaningless without the "how." Now that we've established the non-negotiable connection between high-quality sleep and superior brain function, we move to the practical art and science of building a sleep lifestyle—a personalized protocol that transforms your bedroom from a mere resting place into a true sanctuary for neurological renovation.
This isn't about rigid, one-size-fits-all rules, but about creating a flexible framework based on circadian biology and sleep science. Think of it as curating the perfect environment and habits for your brain's night shift to perform at its peak.
Your master biological clock, the suprachiasmatic nucleus (SCN), needs clear, consistent signals to keep its 24-hour rhythm precise. A strong circadian rhythm is the bedrock of sleep quality.
You cannot sprint into sleep. Your brain needs a transition period—a "buffer zone"—to downshift from the sympathetic-driven alertness of the day to the parasympathetic state required for sleep.
What you consume acts as direct input to your sleep-wake systems.
How you spend your day dictates the quality of your night.
This is where modern technology elevates your protocol from guesswork to a precise science. Using a wearable device to track the biomarkers we discussed—sleep stages, HRV, resting heart rate—allows you to:
Building your sleep sanctuary is an active, ongoing practice of self-care for your brain. It requires intention but pays exponential dividends in cognitive clarity, emotional stability, and long-term health. For a deeper library of practical tips and protocol ideas, our blog is regularly updated with science-backed strategies.

For millions, the struggle with sleep isn't just about poor habits; it's a clinical disorder that hijacks the brain's natural processes. Recognizing when you're facing a disorder versus a correctable habit issue is crucial. Pushing through with standard "sleep hygiene" when you have an underlying condition can be futile and frustrating. Here, we explore common disorders, their direct impact on brain function, and the critical pathways to treatment.
OSA is characterized by repeated collapses of the upper airway during sleep, causing breathing to stop (apneas) or become shallow (hypopneas). Each event triggers a micro-arousal to restart breathing, fragmenting sleep.
Impact on the Brain:
Signs & Action: Loud snoring, witnessed pauses in breathing, and excessive daytime sleepiness are red flags. Diagnosis requires a sleep study. The gold-standard treatment is Continuous Positive Airway Pressure (CPAP), which uses gentle air pressure to keep the airway open. Treatment is often life-changing, restoring healthy sleep architecture and protecting the brain from ongoing damage.
Insomnia isn't just "trouble sleeping." It's a disorder of conditioned hyperarousal, where the brain and body are stuck in a state of heightened alertness at night. As detailed in the vicious cycle section, the insomnia brain shows increased metabolic activity in emotional centers and decreased activity in the PFC.
Impact on the Brain:
Signs & Action: Difficulty falling asleep, staying asleep, or waking too early, occurring at least 3 nights per week for 3 months, despite adequate opportunity for sleep. The first-line, gold-standard treatment is Cognitive Behavioral Therapy for Insomnia (CBT-I), a structured program that retrains sleep habits and thoughts about sleep. It is more effective and durable than sleep medication.
RLS involves an irresistible urge to move the legs, often accompanied by uncomfortable sensations, that worsens at rest and in the evening. PLMD involves involuntary, rhythmic limb jerking during sleep.
Impact on the Brain:
Signs & Action: Uncomfortable "creepy-crawly" sensations in the legs with an urge to move, relief with movement, and a clear evening worsening. Diagnosis is clinical and sometimes confirmed by a sleep study. Treatment may involve iron supplementation (if levels are low) or specific medications that target dopamine or calcium channels.
If you suspect a sleep disorder:
Addressing a sleep disorder is one of the most profound interventions you can make for your brain health. It removes a major physiological obstacle, allowing all the natural, restorative processes we've described to finally function as intended. If you have questions about how wearable data can support conversations with healthcare providers, the Oxyzen FAQ covers this important topic.
The adage "you are what you eat" extends powerfully into the night. The nutrients you consume provide the raw materials for neurotransmitters, modulate inflammation, and influence the production of sleep-regulating hormones. Strategic nutrition supports the brain's repair work during sleep, while poor dietary choices can actively sabotage it.
Emerging research highlights the gut microbiome as a key player in sleep regulation. The gut produces neurotransmitters (about 90% of serotonin is made in the gut) and communicates with the brain via the vagus nerve and inflammatory pathways.
Nutrition for sleep is not about a single "magic" food, but about a consistent pattern of eating that provides stable energy, reduces inflammation, and supplies the specific nutrients your brain needs to manufacture sleep and perform its nocturnal duties. It's a foundational pillar that works synergistically with your other sleep hygiene practices. For more on integrating nutrition with holistic wellness tracking, explore the resources on our blog.
Physical activity and sleep exist in a virtuous, bidirectional cycle. Exercise improves sleep, and high-quality sleep enhances athletic performance and recovery. For the brain, this cycle is particularly potent, as both activities—moving and sleeping—are powerful drivers of neuroplasticity, neurogenesis, and resilience.
Regular, moderate-to-vigorous exercise has a measurable effect on the structure of sleep itself:
The relationship between exercise and sleep is not linear; timing and intensity create a curve.
This is the other side of the cycle. Sleep is when the benefits of exercise are cemented.
For the brain, this means that the neuroplastic sparks ignited by learning and physical challenge during the day are fanned into lasting neural connections during the night. Exercise and sleep are a matched pair for building a more resilient, adaptable, and capable brain. The synergy between activity tracking and sleep analysis is a core focus for performance-minded individuals, a theme often seen in user experiences with Oxyzen.
The hyperaroused state of the modern mind—characterized by rumination, worry, and a constant low-grade stress response—is arguably the single greatest thief of sleep in the 21st century. Fortunately, we have a powerful, innate tool to counter it: the deliberate practice of turning attention inward. Mindfulness and related stress-reduction techniques don't just calm the mind; they directly and positively alter the physiological state of the body and brain, paving a neural pathway to better sleep.
The brain's default mode network (DMN), active during mind-wandering and self-referential thought, is often overactive in poor sleepers and those with anxiety. At night, this translates as the "racing mind." This mental activity:
Mindfulness practices train the brain to observe thoughts and sensations without judgment and to return attention to an anchor (like the breath or body). This has several sleep-specific neurobiological consequences:
These are not abstract concepts but concrete tools to use in your wind-down routine.
Research shows that mindfulness-based interventions (like Mindfulness-Based Stress Reduction or MBSR) lead to:
Building this mind-body bridge is a skill. It requires consistent, short practice. The payoff is a brain that is not only better at sleeping but is fundamentally more resilient during waking hours. This holistic approach to wellness, connecting mental practice with physiological outcomes, aligns with the core philosophy behind Oxyzen's mission to provide a complete picture of health.
The nightly choices we make about sleep are not just loans against tomorrow's energy; they are investments in—or withdrawals from—our cognitive retirement fund. The relationship between sleep across the lifespan and the risk of age-related cognitive decline and neurodegenerative diseases like Alzheimer's and Parkinson's is now one of the most compelling areas of neurological research. Improving sleep is arguably one of the most powerful preventive medicines we have for the aging brain.
Think of the brain processes we've detailed—glymphatic clearance, synaptic homeostasis, cellular repair, anti-inflammatory action. Now imagine these processes being subtly impaired, night after night, for decades. The deficit compounds.
Conversely, prioritizing sleep builds brain resilience:
It's normal for sleep architecture to evolve. Understanding this helps us adapt our habits proactively.
The message is one of profound hope and agency. While we cannot control all risk factors for brain aging, sleep is a domain where we have significant influence. The journey to protect your brain for the long term begins tonight. For a deeper exploration of the science of sleep and longevity, our blog features ongoing analysis of the latest research in this critical field.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/