Sleep Pattern Tracking: What to Monitor Week by Week
Week-by-week, track your bedtime, wake time, total sleep, and energy levels to identify what routines yield your best rest.
Week-by-week, track your bedtime, wake time, total sleep, and energy levels to identify what routines yield your best rest.
We spend roughly one-third of our lives asleep, yet for many of us, this vital process remains a profound mystery. We know we need it, we crave it when we don’t get enough, but understanding the intricate architecture of our own sleep has, until recently, been the domain of sleep labs and overnight studies. Enter the era of the smart ring: a discreet, powerful tool that has democratized sleep tracking, offering a nightly window into our restorative cycles from the comfort of our own beds. But with a deluge of data at our fingertips—from heart rate variability to oxygen saturation—a critical question emerges: What does it all mean, and what should you actually focus on?
Tracking your sleep isn’t about chasing a perfect score or becoming obsessive about a single metric. It’s a journey of self-discovery, a process of uncovering the unique rhythms and needs of your body. This is where a week-by-week monitoring framework becomes transformative. Rather than reacting to a single night’s poor reading, this methodical approach allows you to observe trends, identify patterns, and connect the dots between your daily habits and your nocturnal life. It transforms raw data into actionable wisdom.
This article is your comprehensive guide to that journey. We will move beyond the basics, diving deep into the key metrics you should monitor, the meaningful connections between them, and how to interpret the story they tell over weeks. Whether you are a new user of a device like the Oxyzen smart ring or a seasoned biohacker looking to refine your approach, this framework will help you cultivate not just better sleep data, but genuinely better sleep. For a deeper dive into the technology making this possible, you can always discover how Oxyzen works on our main site.
Our exploration begins with the foundational elements of sleep architecture, then progresses through the interconnected systems of your body, and finally guides you in building a holistic, sustainable sleep practice. Let’s begin the first week of understanding.

Before you can improve something, you must first learn to measure it correctly. Sleep architecture refers to the basic structure of your sleep—the cyclical stages your brain and body progress through each night. Modern smart rings use a combination of accelerometers, optical heart rate sensors, and sophisticated algorithms to estimate these stages. Your first weeks of tracking should be dedicated to understanding and establishing your baseline in these core areas.
Total Sleep Time vs. Time in Bed: This is the most fundamental, yet often misunderstood, metric. Your goal is to maximize actual sleep time, not just the hours you spend in bed. A ring tracking your movement and heart rate can pinpoint the exact moment you fall asleep and wake up, revealing the gap between "lights out" and "sleep on." In your first week, observe this discrepancy. Is it 10 minutes or 45? This "sleep latency" is your first clue about your wind-down effectiveness.
Sleep Stages Breakdown (Light, Deep, REM): Your sleep is not a monolithic state. It's a carefully choreographed dance of stages:
During your initial weeks, don't panic over nightly fluctuations. Instead, look at your weekly averages. Does your deep sleep dip after intense workouts or stress? Does your REM increase on weekends when you sleep in? These are the patterns you’re seeking. For more insights on interpreting this data, our resource hub offers additional resources and related articles.
Sleep Consistency: The Power of Routine: Perhaps more impactful than any single night’s perfect score is the consistency of your sleep schedule. Your body’s internal clock, the circadian rhythm, thrives on predictability. A smart ring can track your "sleep midpoint" (the halfway point between falling asleep and waking) and your bedtime/waketime variability. In week two, shift your focus from just how long you sleep to how regularly you do it. Going to bed and waking up within a 30-minute window every day—even on weekends—can dramatically improve sleep quality over time. This consistency reinforces your circadian rhythm, making falling asleep easier and wake-ups more natural.
By establishing a clear baseline of your sleep architecture, you create a stable foundation. You move from wondering "Did I sleep well?" to knowing exactly how your sleep is structured. This knowledge sets the stage for the next layer of insight: understanding the physiological symphony playing beneath the surface of those sleep stages.
Once you’ve mapped the landscape of your sleep stages, it’s time to listen to the music of your nervous system. This is where heart rate (HR) and, more importantly, Heart Rate Variability (HRV) become your most insightful metrics. While you sleep, your body shifts into "rest and digest" mode, governed by the parasympathetic nervous system. A smart ring provides an unparalleled, continuous look at this shift throughout the night.
Nightly Resting Heart Rate (RHR): Your resting heart rate during sleep is typically the lowest and most truthful reflection of your cardiovascular fitness and recovery state. A well-recovered body allows the heart to slow down significantly. Track your sleeping RHR trend over weeks, not days. A consistent downward trend or a stable low number is a positive sign of improving fitness and recovery. Conversely, a spike in your sleeping RHR that persists for several nights can be an early warning sign of impending illness, excessive stress, or overtraining.
The Master Metric: Heart Rate Variability (HRV): If you focus on only one advanced metric, let it be HRV. It measures the subtle variations in time between each heartbeat. Higher HRV generally indicates a more resilient, adaptable nervous system—your body is poised to handle stress effectively. During deep, restorative sleep, your HRV should rise as parasympathetic activity dominates.
Connecting HR/HRV to Sleep Stages: Now, synthesize this data. Look at nights with high deep sleep percentages. Do they correlate with your highest HRV readings? They likely will. Notice how during REM sleep, your heart rate may become more variable and increase slightly—this is normal. By weeks three and four, you’ll start to see a beautiful correlation: quality sleep architecture (plenty of deep sleep) drives physiological recovery (high HRV), which in turn prepares you for better wakeful function. This feedback loop is the core of intelligent biohacking. Many users share how this insight changed their approach to rest; you can read real customer reviews and user experiences to see this in action.
Understanding your nocturnal HR and HRV transforms sleep tracking from a simple sleep report card into a dynamic recovery dashboard. It tells you not just how you slept, but how recovered you are from the previous day’s demands. This leads us naturally to another critical, and often overlooked, nocturnal metric: the oxygen levels in your bloodstream.

While heart metrics tell the story of your nervous system, your blood oxygen levels—or SpO2—provide a direct readout of your respiratory health during sleep. For most healthy individuals, oxygen saturation remains stable and high (95-100%) while awake. During sleep, a slight dip of 1-2% is normal. However, significant or frequent drops can be indicative of disruptions that fragment sleep and strain the cardiovascular system, even if you don’t consciously wake up.
Establishing Your Baseline SpO2: Your first task is to establish your personal, healthy baseline. Over a week of normal health (not during a cold or respiratory illness), note your average nightly SpO2 and the typical range. Most smart rings will give you an average and sometimes a "low" value. Knowing your baseline is critical; it turns a generic number into a personal health marker.
Understanding SpO2 Dips and Fluctuations: Not all dips are cause for alarm. Brief, minor fluctuations can occur during shifts in sleep stages or changes in position. What you’re monitoring for are trends:
The Connection to Sleep Quality: Repeated oxygen desaturations trigger a stress response—your brain receives an "oxygen alert" and partially arouses you to reopen airways. This breaks the natural progression of sleep cycles, stealing precious deep and REM sleep. You may never remember waking, but you’ll feel the effects in morning fatigue, brain fog, and a high resting heart rate. Tracking SpO2 over weeks can reveal patterns linked to lifestyle factors like evening alcohol consumption, allergies, or sleeping position.
Monitoring nocturnal SpO2 empowers you with proactive knowledge. It moves the conversation from "I’m tired" to "my data shows possible breathing disruptions." This objective information can be invaluable for discussing sleep health with a professional. For any technical questions on how this tracking works, our comprehensive support and FAQ section is available.
With a firm grasp on the internal symphony of heart, nerves, and breath, we now turn outward. Your body’s movement during sleep holds its own treasure trove of clues about restlessness, environment, and routine.
You might think perfect sleep means lying completely still. In reality, the body makes dozens of minor postural shifts throughout the night to prevent pressure sores and maintain comfort. However, excessive movement or restlessness is a primary indicator of disrupted, shallow sleep. Your smart ring’s accelerometer quantifies this nightly dance, offering insights into sleep continuity and environmental disturbances.
Interpreting Movement Data: The movement graph is not about judging fidgeting; it’s about identifying disruptions. Look for:
Correlating Movement with Other Metrics: The true power of movement data is revealed in synthesis. Cross-reference your movement spikes.
Environmental and Lifestyle Triggers: Over several weeks, use the movement data as a detective tool. Experiment and observe:
By tracking movement trends, you move from passively experiencing a "bad night" to actively identifying potential causes. It shifts the question from "Why did I sleep poorly?" to "What happened at 2:47 AM that caused that major movement and heart rate spike?" This forensic approach allows for targeted adjustments. To learn more about the philosophy behind creating technology for such deep self-understanding, you can explore our brand journey and founding story.
Now that we’ve explored the core physical metrics, it’s time to add a crucial, subjective layer to our objective data: the qualitative experience of sleep and wakefulness.
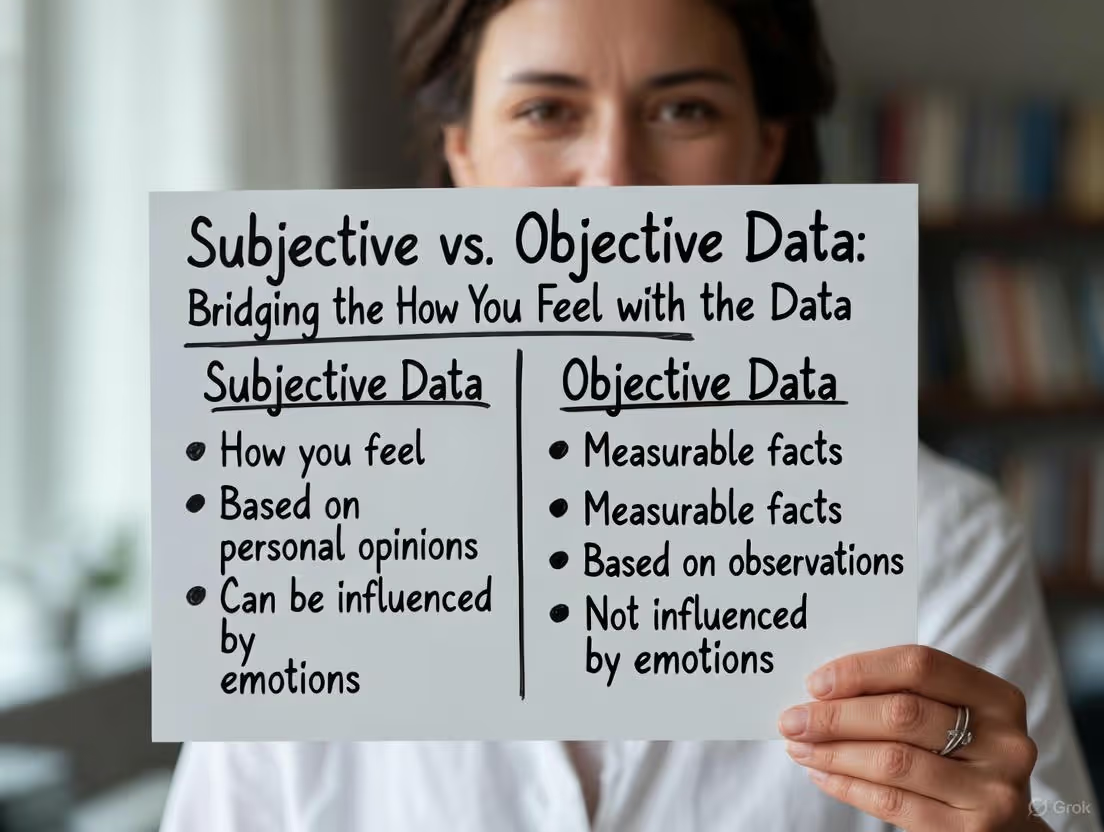
Here lies one of the most profound aspects of week-by-week sleep tracking: the dialogue between the quantitative (the numbers from your ring) and the qualitative (your lived experience). The data is meaningless if it doesn’t connect to how you feel. Conversely, your feelings can be misleading without data. Bridging this gap is where true insight and personalization happen.
The Morning Feelings Check-In: Before you even look at your sleep score, practice a mindful self-assessment. Use a simple 1-5 scale for:
Comparing Sensation to Scores: Now, compare your subjective ratings to the night’s objective data. This is where patterns emerge over weeks.
Refining Your Personal Algorithm: Your unique biology is the ultimate authority. Over weeks of comparison, you will start to identify which objective metrics most strongly predict your subjective well-being. For one person, HRV might be the king predictor. For another, it might be the number of movement events. For a third, it could be the stability of their SpO2. This process allows you to personalize the importance of each metric, moving from a generic sleep score to a truly individualized recovery index.
This practice of bridging subjective and objective data fosters body literacy. It teaches you to trust the data as a guide while also honoring your own perceptions. It turns sleep tracking from an external judgment into an internal conversation. This holistic view naturally extends beyond the night and into the choices you make during the day.
Your sleep is not an isolated event; it is the nightly report card on your daytime life. The food you eat, the stress you manage (or don’t), and the timing of your physical activity send powerful signals to your circadian biology. Week-by-week tracking allows you to become a scientist of your own habits, running experiments to see their clear impact on your nocturnal data.
Exercise Timing and Sleep Impact: Physical activity is a potent sleep promoter, but its timing matters.
Nutritional and Hydration Effects: What you consume is information for your body’s nightly repair processes.
Stress and Wind-Down Routines: Daytime stress that isn’t processed can follow you to bed, keeping your nervous system in a sympathetic ("fight or flight") state. Your HRV data is the perfect barometer for this.
By methodically observing these daytime influences over weekly blocks, you move from guesswork to cause-and-effect understanding. You stop saying "I slept badly" and start saying "The spicy meal and late work stress likely caused my high restlessness and low deep sleep." This empowerment is at the heart of our mission and company information.
With an understanding of how day affects night, we must also consider a powerful, external force that orchestrates our entire sleep-wake cycle: light.
Your sleep is governed by a master clock in your brain's hypothalamus—the suprachiasmatic nucleus (SCN). This circadian rhythm is not a suggestion; it’s a biological mandate that influences everything from hormone release to cellular repair. The most powerful cue that sets and syncs this clock is light. Week-by-week tracking of your sleep timing, especially when combined with light exposure habits, can unlock a new level of rhythm optimization.
Sleep Midpoint and Social Jet Lag: Your sleep midpoint (the halfway point between sleep onset and wake time) is a brilliant, simple metric for circadian alignment. A consistent midpoint suggests a well-anchored rhythm.
The Power of Morning Light: Exposure to bright, natural light within 30-60 minutes of waking is the most potent signal to tell your SCN that "daytime has begun." This starts a countdown for the evening release of melatonin, the sleep hormone. Over a week of prioritizing morning light, you may observe an earlier, more natural decline in evening heart rate and improved sleep latency.
Evening Light Avoidance: Conversely, blue and bright light in the evening (from phones, computers, TVs) tricks your SCN into thinking it’s still daytime, suppressing melatonin and delaying sleepiness. Observe your data on nights after heavy screen use vs. nights with a "digital sunset" (using blue light blockers or avoiding screens for 90 minutes before bed). The impact on sleep latency and the first deep sleep cycle can be significant.
Aligning Sleep with Your Chronotype: Are you a natural "lark" (morning person) or "owl" (evening person)? Your data will reveal this over time. Owls will naturally have a later sleep midpoint and may struggle with early-morning deep sleep. Larks will have an early midpoint and may experience evening sleepiness. Respecting your chronotype by scheduling your sleep window as consistently as possible within its natural bounds is more effective than fighting it. The goal is regularity within your own biological framework.
Tracking your sleep over weeks with a focus on timing and light exposes the macro-rhythms of your life. It reveals the disconnect between social demands and biological needs, allowing you to make intentional compromises and protect your rhythm where it matters most. This foundational rhythm sets the stage for the ultimate goal: using all this data to craft not just better nights, but better, more energized days.

The ultimate purpose of understanding and optimizing your sleep is to enhance your waking life—your energy, focus, mood, and performance. This section connects the nocturnal dots we’ve been tracking to your daytime reality. It’s about closing the loop and proving that the investment in sleep pays dividends in every aspect of your life.
Predicting Daytime Readiness: Your previous night’s sleep data, particularly composite scores and HRV, can be powerful predictors of your capacity for the day ahead. A week of high HRV and strong deep sleep should correlate with a week of stable energy, better workout performance, and emotional resilience. Conversely, a trending dip in your weekly HRV average is a data-backed reason to schedule a lighter workout day or prioritize stress-management techniques.
Cognitive Metrics and Sleep: While current smart rings don’t measure brainwaves, they proxy cognitive recovery through other metrics.
Physical Performance and Recovery: This is the most direct connection for athletes and active individuals.
The Subjective-Objective Performance Loop: This is where it all comes together. You feel energetic (subjective), you have a great, focused work session and a strong workout (performance), and your ring data from the night before shows high deep sleep and excellent HRV (objective). This positive reinforcement loop makes the value of sleep tangible. You’re not just "getting sleep"; you’re fueling performance. For stories of how others have made this connection, our community shares their journeys in our testimonials and user experiences.
By consciously linking your weekly sleep trends to your weekly performance outcomes, you elevate sleep from a passive state to an active tool for personal and professional mastery. This holistic view prepares us to address one of the most common pitfalls in the tracking journey: what happens when the data isn’t what we want it to be, and anxiety creeps in.
In the quest for perfect sleep, a paradox can emerge: the very act of tracking can become a source of stress that degrades sleep. Watching your live HRV dip as you lie awake worrying about it is a self-defeating cycle. The goal of week-by-week tracking is to foster awareness, not anxiety. This section provides the mindset shifts needed to use your data as a gentle guide, not a harsh judge.
Embracing Trends Over Nightly Scores: This is the cardinal rule. A single night of poor sleep is meaningless noise in the context of your health. Your body operates on cycles, not 24-hour snapshots. Train yourself to care about your 7-day and 30-day averages for key metrics like Total Sleep, Deep Sleep %, and HRV. A bad night is just a data point; a bad week-long trend is information you can act upon.
The "Good Enough" Sleep Mindset: The pressure to achieve a perfect "90+" sleep score every night is unrealistic and counterproductive. Sleep needs and quality naturally vary. Adopt a "good enough" mindset—aiming for consistency and general alignment with your targets, not perfection. Sometimes, 7 hours of decent sleep with a stable rhythm is more valuable than 8.5 hours of fragmented sleep achieved with obsessive rituals.
When to Take a Break from Tracking: If you find yourself feeling anxious at bedtime about your "score," or compulsively checking the app in the middle of the night, it’s time for a detox. Wear your ring for continuity of data, but hide the app from your phone’s home screen. Commit to not looking at your scores for a full week. Instead, focus solely on your subjective feeling upon waking and practicing good sleep hygiene. This breaks the neurotic connection and resets your relationship with the tool.
Using Data for Curiosity, Not Judgment: Reframe your interaction with the data. Instead of: "My deep sleep was terrible last night, I failed," try: "Fascinating. My deep sleep was low. I had that late coffee and stressful work call before bed. Let’s experiment with cutting caffeine after 2 PM and doing a 10-minute meditation tomorrow night and see what happens." This shifts you from a passive victim of your data to an active, curious investigator of your own biology.
This mindful approach ensures that your smart ring remains what it was designed to be: an empowering tool for self-knowledge, not another source of digital stress. It allows you to step back and see the broader narrative that is unfolding over the weeks and months of your life, which is where the most profound insights await.
Theory and metrics are essential, but application is everything. Let’s translate everything we’ve discussed into a practical, actionable 4-week protocol. This journey is designed to move you from data collection to baseline establishment to initial experimentation, all while cultivating a sustainable, informed relationship with your sleep.
Weeks 1 & 2: The Observation Phase – "Collect Don’t Correct"
Week 3: The Connection Phase – "Spot the Patterns"
Week 4: The First Experiment Phase – "One Gentle Intervention"
By the end of this first month, you will have moved from being a passive sleeper to an informed self-observer. You will have a clear, personal baseline and have taken the first step in using data to guide positive change. This foundational work prepares you for the long-term journey of refinement and mastery, where you learn to adapt your sleep to life’s changing circumstances. For ongoing support and ideas as you continue this journey, remember that you can always explore our blog for more wellness tips.
Having completed your foundational 4-week journey, you now possess something invaluable: a personalized sleep baseline. You are no longer guessing; you have a data-driven understanding of your unique sleep architecture, nervous system rhythms, and how your daily choices echo through the night. This knowledge marks the transition from passive observation to active optimization. The next eight weeks are about refinement, mastery, and learning to adapt your sleep to the dynamic flow of life. We will delve into advanced correlation tracking, tackle specific sleep challenges, explore environmental fine-tuning, and build a resilient sleep practice that endures.
In the initial phase, you learned to observe individual metrics. Now, it's time to become fluent in the language they speak together. Sleep metrics are not isolated silos; they exist in a dynamic, interconnected ecosystem. Understanding their interplay—how a dip in one can trigger a cascade in others—provides a holistic picture of your health that is greater than the sum of its parts. This week-by-week synthesis is where the deepest insights are found.
The Stress Cascade: A Classic Pattern: Follow this common negative loop across a week:
The Recovery Symphony: A Positive Feedback Loop: Conversely, observe the beautiful synergy of a positive cycle:
Spotting Compensatory Patterns: Your body is always seeking balance. Look for compensatory actions over a multi-day period.
By spending weeks 5-8 mapping these complex interactions, you graduate from reading single data points to interpreting the full story of your recovery. You learn to see your body as an intelligent system, constantly adapting and communicating its needs. This systemic understanding is central to the vision and values behind creating technology that fosters this kind of deep self-awareness.
Armed with an understanding of your baseline and the interplay of metrics, you can now move from general observation to targeted problem-solving. Most people face one or two persistent sleep challenges. Use your weekly trends to diagnose the root cause, not just the symptom, and run focused 2-3 week experiments to address them.
Challenge 1: Difficulty Falling Asleep (High Sleep Latency)
Challenge 2: Frequent Night Wakings (Sleep Fragmentation)
Challenge 3: Waking Up Tired (Unrefreshing Sleep)
By dedicating blocks of time to address specific challenges, you move from feeling helpless about poor sleep to being an empowered problem-solver with a clear, data-informed action plan. For more personalized strategies and community insights, our blog is a repository of related articles and deep dives on these very topics.
Your sleep environment is the stage upon which the nightly drama of restoration plays out. Even with perfect habits, a poor environment can sabotage your efforts. Over several weeks, use your ring’s data—particularly the movement and restlessness metrics—to conduct a forensic audit of your bedroom and make incremental, evidence-based improvements.
Temperature Optimization: This is arguably the most critical environmental factor. Core body temperature must drop to initiate and maintain sleep.
Light Pollution and Darkness: Even small amounts of light can fragment sleep and suppress melatonin.
Noise Disruption and Soundscaping: Intermittent noise is a prime cause of sleep fragmentation, even if you don't remember waking.
The Bed Itself: Your mattress, pillows, and bedding contribute directly to physical comfort, measured as restlessness.
Treating your bedroom as a laboratory over an 8-week period allows you to build a sanctuary scientifically tailored to your body’s needs. This creates a foundation so solid that it supports great sleep even when other life factors are in flux. It’s an investment in your nightly recovery that pays off for years to come.
Life is not a controlled laboratory. The true test of your sleep mastery is how well your understanding and habits hold up during disruptions: business trips, periods of intense stress, holidays, or illness. This phase of tracking is about resilience—using your data not to maintain perfection, but to navigate turbulence and guide a faster return to baseline.
Managing Jet Lag and Travel: Travel is a brutal assault on circadian rhythms. Use your ring strategically.
Navigating Periods of High Stress: During a work crunch or family crisis, sleep optimization feels frivolous. Shift your goal from "great sleep" to "protective sleep."
Illness and Recovery: Your biometrics provide an early-warning system and a recovery roadmap.
By tracking through life’s ups and downs, you develop a flexible, compassionate relationship with your sleep. You learn that the goal is long-term rhythm and resilience, not nightly perfection. This adaptable mindset is what sustains a lifelong practice of sleep health. For support and answers during challenging transitions, our FAQ and support section is a valuable resource.
As you accumulate months of consistent data, a new, powerful perspective emerges: the macro view. Zooming out from weekly trends to monthly and quarterly overviews reveals the slow, rhythmic cycles of your biology and provides profound insights into your long-term health trajectory. This is where sleep tracking transitions from a wellness tool to a preventative health asset.
Seasonal Variations: You may discover your body has seasonal rhythms.
Lifestyle Change Validation: Making a major lifestyle change? Your long-term sleep data is the ultimate validation.
Aging and Your Sleep Baseline: Sleep architecture changes naturally with age. Deep sleep percentage gradually decreases. The value of long-term tracking is that you understand your personal rate of change. You can differentiate between a natural, gradual shift and a sudden deviation that might indicate a health issue. Maintaining high sleep consistency and circadian alignment becomes increasingly important to compensate for these natural changes.
Proactive Health Conversations: Your long-term data portfolio is powerful in a clinical setting. Instead of saying "I'm tired," you can say: "Over the past six months, my nocturnal SpO2 has shown an increasing number of dips below 88%, correlating with more nighttime restlessness. Here are the graphs." This objective, longitudinal data can help healthcare professionals make more precise assessments.
This macro view fosters a sense of stewardship over your health. You are no longer tracking for a score, but curating a long-term dataset that tells the story of your life in biometrics. It underscores the profound mission of empowering individuals with knowledge that was once inaccessible.
Sleep does not exist in a vacuum. It is one critical pillar in the temple of your overall well-being. To truly master your health, the final step is to integrate your weekly sleep insights with other streams of data from your life. This creates a holistic dashboard, allowing you to see the cause-and-effect relationships between movement, nutrition, and recovery in high definition.
The Activity-Sleep Feedback Loop: Syncing your ring data with your fitness tracker or workout app is essential.
Nutrition Logging and Sleep Quality: While tedious long-term, periodic 1-2 week deep dives into nutrition can be illuminating.
Stress Tracking and HRV Correlation: Use a simple daily stress score (1-10) in a journal app. Plot this against your nightly HRV. The correlation is often stark and teaches you which types of stress (e.g., work deadlines vs. social conflict) have the greatest physiological impact on your recovery. This makes your HRV data emotionally intelligible.
The Unified Dashboard Mindset: The goal is not to become a data zombie, but to periodically synthesize. Once a month, look at your weekly averages side-by-side: Sleep, Activity, subjective Stress, and any dietary notes. Ask: "What is the story of my last month? Did my intense training block pay off in better fitness (lower RHR) despite lower HRV? Did that stressful project leave a clear fingerprint on my deep sleep?" This integrated analysis turns disparate data points into a coherent narrative of your health journey.
By connecting these dots, you achieve a systems-level understanding of yourself. You can make informed decisions like, "I have a big presentation tomorrow, so I'll prioritize sleep consistency over a late workout today," based on how you know each factor influences your recovery. For those looking to dive deeper into holistic tracking methodologies, we encourage you to explore our blog for more wellness tips and advanced guides.
After months of tracking, experimenting, and integrating, a subtle but profound shift occurs. The constant checking of the app diminishes. The anxiety over a single red metric fades. You internalize the rhythms. You become a Sleep Master—not because you always sleep perfectly, but because you have cultivated a deep, intuitive partnership with your body's need for rest. This final section is about transcending the tool to embody the practice.
Data as a Guide, Not a Gospel: The ring is a mirror, reflecting your state. It is not the truth itself. The ultimate authority is your subjective feeling of well-being. A Sleep Master knows when to trust a "good feeling" over a mediocre score and when to heed a "bad score" even when feeling okay. They use data to inform intuition, not replace it.
Embracing Natural Variation: The master understands that sleep, like the weather, has fronts and systems. There will be storms (nights of poor sleep) and dry spells (periods of high stress). They do not panic. They observe the patterns, make gentle adjustments, and trust in the body's resilient ability to return to its mean. They care for the soil (consistent habits) and don't fret over a single fruit (a single night).
The Ritual Over the Result: The focus shifts from the morning's sleep score to the evening's wind-down ritual. The pleasure is in the hot tea, the pages of a book, the feeling of cool sheets, the deliberate act of breathing. The master knows that by honoring the ritual, the result—restorative sleep—becomes a natural byproduct, not a forced outcome.
Sharing the Journey: Finally, the Sleep Master often becomes a gentle guide for others. They share not dogma, but curiosity. They might show a partner how their snoring correlates with SpO2 dips, or help a friend see the impact of late-night screens on their sleep latency. The knowledge becomes a gift, offered without pressure. They embody the principles behind our company's story and vision: that understanding our own biology is the first step toward living a more conscious, vibrant life.
The path to sleep mastery is not a linear journey with a definitive endpoint. It is a spiral of deepening understanding, where each cycle—each week, each month, each season—reveals new layers of connection between your daily life and your nocturnal restoration. Having moved from foundational tracking to targeted optimization and holistic integration, you now stand at a point of empowered fluency. The final portion of our exploration looks forward. We will examine how to maintain this practice for the long term, explore the emerging frontiers of sleep science and technology, and solidify the philosophy that turns sleep tracking from a temporary project into a sustainable, lifelong pillar of well-being.
Without a structured approach, even the most dedicated tracker can fall into data drift—wearing the device out of habit but losing the conscious connection to the insights. The solution is not daily obsession, but deliberate, periodic reflection. Instituting a formal Quarterly Sleep Review transforms your accumulated data from a passive log into an active guide for the coming season.
Setting Your Review Cadence: Every 13 weeks, block 60-90 minutes in your calendar for a personal health audit. This timeframe is long enough to reveal meaningful trends but frequent enough to allow for course correction. Approach it with curiosity, not judgment.
What to Analyze in Your Quarterly Review:
Setting Intentions for the Next Quarter: Based on your review, set one or two simple, seasonal intentions.
This ritual of review keeps you engaged without being overwhelmed. It ensures your smart ring remains what it was designed to be: a tool for conscious living, not just passive tracking. For new ideas to incorporate into your quarterly reviews, our blog is continually updated with the latest research and strategies.
The field of consumer sleep technology is advancing at a breathtaking pace. While today’s smart rings provide a revolutionary window into our physiology, the next five years promise even deeper, more nuanced, and more actionable insights. Understanding these horizons helps you contextualize your current data and anticipate the future tools that will further personalize your sleep journey.
Moving Beyond Staging to Sleep Quality: Current algorithms are excellent at estimating sleep stages based on movement and heart patterns. The next frontier is assessing sleep quality within those stages. Future sensors may be able to detect the stability of your deep sleep (the "slow-wave" activity) or the density of your REM sleep, offering a finer-grained picture of restoration than stage percentages alone.
Integrated Metabolic and Glucose Insights: The relationship between metabolic health and sleep is bidirectional. Emerging non-invasive or minimally invasive biosensors aim to provide continuous glucose monitoring (CGM) data alongside sleep metrics. Imagine correlating your nocturnal heart rate variability with nighttime glucose stability, or seeing how a late meal directly impacts your sleep architecture and morning fasting glucose. This would create a powerful feedback loop for metabolic and sleep health.
Advanced Respiratory Analysis: While current SpO2 sensors detect blood oxygen dips, future iterations may analyze breathing patterns themselves—detecting the subtle signatures of different types of sleep-disordered breathing, from classic apnea to UARS (Upper Airway Resistance Syndrome). This could provide much earlier, more accessible screening tools.
Cognitive Readiness Scores: The ultimate goal of sleep is to prepare the brain for the day. Future devices may integrate simple, morning reaction-time tests or voice analysis to provide an objective "cognitive readiness" score that correlates with your sleep data, closing the loop between last night’s rest and today’s actual mental performance.
The Role of AI and Personalized Coaching: The true power of long-term data sets will be unlocked by artificial intelligence. Instead of you spotting trends, an AI could analyze your year of data and say: "Based on your historical patterns, when your HRV drops for three days and your sleep latency increases, you have an 80% likelihood of coming down with a cold. Suggesting: reduce activity, increase hydration, and prioritize sleep extension for the next 48 hours." This moves from tracking to true predictive, personalized health guidance.
As these technologies evolve, the core principles you’ve mastered—observing trends, correlating lifestyle, and listening to your body—will remain essential. The tools will get smarter, but your role as the conscious interpreter of your own data will only become more important. Staying informed on these developments is part of the journey; you can discover how Oxyzen works to see our approach to evolving technology.
One of the most responsible outcomes of diligent self-tracking is knowing when to hand off the data to a professional. Your smart ring is a powerful screening tool and a source of objective evidence, but it is not a diagnostic device. Understanding the red flags and patterns that warrant a professional consultation is a critical aspect of sleep mastery.
Persistent, Unexplained Trends: Data is most valuable in revealing patterns that defy your lifestyle adjustments.
Presenting Your Data Effectively: When you schedule a consultation, come prepared. Do not just show daily graphs.
Collaborative Care: The ideal scenario is a partnership. Your data provides a longitudinal view no single night in a lab can capture. The professional provides clinical expertise and diagnostic tools. Together, you can form a more complete picture and a more effective treatment plan. This empowered patient approach is the future of healthcare. For any questions about the capabilities and limits of your device data, our support and FAQ section offers clear guidance.
Humans are social creatures, and behavior change is profoundly influenced by community. As you solidify your own practice, consider extending the benefits by cultivating a sleep-aware community in your circles. This isn’t about evangelizing or creating pressure; it’s about shared curiosity and mutual support.
Partner and Family Sync: Sleep is often a shared—and sometimes contested—resource in a household.
Workplace Wellness Advocacy: The impact of sleep on productivity, creativity, and workplace safety is well-documented. You can be a subtle advocate.
Online and Social Communities: Engaging with others on a similar journey can provide motivation, new ideas, and perspective.
Building these communities reinforces your own commitment and turns personal optimization into a positive social force. It reflects the collective journey we're all on, much like the one shared in our community’s real customer reviews and experiences.
As we invite increasingly intimate data into our lives, it’s imperative to pause and consider the broader implications. Sleep tracking, at its best, fosters autonomy and self-knowledge. At its worst, it can fuel obsession, anxiety, and a disconnection from our innate bodily wisdom. Navigating this space thoughtfully is the mark of a true practitioner.
Data Ownership and Privacy: Your sleep data is a biometric diary. It’s crucial to understand who owns it, how it is stored, and how it might be used. Read the privacy policies of your device makers. Choose companies that are transparent about data anonymization and give you control. Your intimate physiological patterns are not a commodity to be sold without your explicit, informed consent.
The Quantified Self vs. The Qualified Self: This is the core philosophical balance. The "Quantified Self" seeks to measure everything. The "Qualified Self" seeks meaning from those measurements. Your goal is to be both. The data (quantified) must always be in service of a richer, more vibrant lived experience (qualified). When tracking starts to diminish your joy, your spontaneity, or your trust in your own feelings, it’s time to step back and re-qualify your life.
Avoiding Neuroticism and Orthosomnia: "Orthosomnia" is a clinically recognized condition where the pursuit of perfect sleep via trackers creates insomnia and anxiety. The remedy is the mindset you’ve been cultivating: trend-watching over score-chasing, self-compassion over self-criticism, and ritual over result. Remember, the device is a tool for understanding your natural sleep, not an instructor dictating what it should be.
Sleep as a Biological Right, Not a Performance Hack: In our productivity-obsessed culture, it’s easy to frame sleep as just another biohack for getting more done. While the performance benefits are real, we must reclaim the deeper truth: Sleep is a fundamental biological necessity. It is a time for healing, integration, and dreaming. It is an act of being, not doing. Honoring it as such protects your practice from becoming just another form of optimized labor.
Embracing these ethical considerations ensures your journey remains healthy, balanced, and sovereign. It aligns with the deeper vision and values of using technology not to replace our humanity, but to help us live more fully within it.
We began this comprehensive guide with a simple premise: to understand what to monitor in your sleep, week by week. We’ve traversed from the foundational architecture of sleep stages to the subtle symphony of heart rate variability; from the silent signifiers of oxygen saturation to the tangible impact of light and lifestyle. We’ve explored how to target challenges, audit environments, integrate data, and maintain a healthy, long-term mindset.
The journey you’ve embarked upon is, in truth, unending. It is a lifelong conversation with the most restorative one-third of your life. The weeks will turn into months, the months into years. You will have seasons of pristine sleep and periods of tumultuous rest. Through it all, the framework you now possess—observe trends, correlate context, experiment gently, review periodically—will serve you.
The ultimate goal was never a perfect sleep score. It was sleep literacy. It is the ability to listen to the language of your own body, to understand the signals it sends through fatigue and alertness, and to respond with informed, compassionate choices. Your smart ring is merely the translator in this dialogue.
As you move forward, let the data inform you but not define you. Let it empower you to advocate for your health, to set boundaries that protect your rest, and to appreciate the profound, nightly miracle of restoration that is your birthright. Continue to explore our blog for more wellness tips as your journey evolves, and remember that this path of discovery is one you walk for yourself, guided by your own unique rhythms and nurtured by your own growing wisdom.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/