Stress Tracking and Gut Health: The Vagus Nerve Connection
The vagus nerve connects gut and brain; tracking gut symptoms alongside stress can reveal this connection and guide interventions like breathing exercises.
The vagus nerve connects gut and brain; tracking gut symptoms alongside stress can reveal this connection and guide interventions like breathing exercises.
You know that feeling. A knot in your stomach before a big presentation. Butterflies before a first date. A sinking gut feeling when something is wrong. We’ve long used the language of our gut to describe our emotional state, but we’ve treated it as mere metaphor. What if it’s not metaphorical at all? What if your stomach is literally churning because of stress, and that stress is systematically eroding your health from the inside out?
For decades, we’ve treated the mind and the gut as separate entities—one handled by therapists and meditation apps, the other by gastroenterologists and probiotics. But a revolutionary understanding in neuroscience and physiology is shattering that divide. At the center of this paradigm shift is a wandering, meandering nerve known as the vagus nerve. This biological superhighway is the physical link between your brain’s stress centers and your gut’s complex ecosystem, and it holds the key to understanding why chronic stress doesn’t just make you anxious—it can make you profoundly, physically ill.
Today, we stand at the precipice of a new era in personalized wellness, where technology like advanced smart rings allows us to move beyond simply feeling stressed to objectively tracking its physiological footprint. This isn't about counting steps; it's about measuring the very rhythms of your nervous system and its impact on your core health. This article will explore the profound connection between the stress you track and the gut health you experience, demystifying the vagus nerve’s role and providing a roadmap for using modern technology to heal this critical axis. We’ll journey from the ancient understanding of the gut as the seat of emotion to the cutting-edge science of the gut-brain axis, and reveal how quantifying your body’s stress response is the first, crucial step toward reclaiming your vitality.
We often think of our brain as the command center, issuing orders to the passive organs below. But this hierarchical model is dangerously outdated. A more accurate picture is one of a constant, dynamic, two-way conversation. This is the gut-brain axis: a complex, bidirectional communication network linking your central nervous system (your brain and spinal cord) with your enteric nervous system (the intricate network of neurons embedded in the walls of your gastrointestinal tract).
This “second brain” in your gut, containing over 100 million neurons, doesn’t just handle digestion. It’s in continuous dialogue with the brain above, using a sophisticated language of hormones, immune messengers, and neural signals. The primary channel for this neural chat is the vagus nerve, a cranial nerve that acts as a direct telephone line running from your brainstem to your abdomen, touching your heart, lungs, and nearly every major organ along the way.
But the conversation isn’t just between two “brains.” A critical third party is always at the table: your gut microbiota. This vast community of trillions of bacteria, viruses, and fungi isn’t just along for the ride. It’s an active participant, producing a plethora of neuroactive compounds—like serotonin, dopamine, and gamma-aminobutyric acid (GABA)—that directly influence brain function. In fact, an estimated 90% of your body’s serotonin, a key neurotransmitter for mood regulation, is produced in the gut. Your microbes are literally sending chemical messages that shape your thoughts, emotions, and stress resilience.
When this three-way dialogue flows smoothly, the result is homeostasis: balanced digestion, stable mood, effective immune response, and restorative sleep. Stress, however, is the static on the line. It disrupts the signal, garbles the messages, and can eventually lead to a complete breakdown in communication, with dire consequences for both mental and physical health. Understanding this axis is the foundation for everything that follows, as we explore how the wearables on our fingers can now listen in on this ancient, vital conversation. For those looking to dive deeper into the science of wellness tracking, our Oxyzen blog features a wealth of resources on how modern technology interprets these biological signals.
So, what exactly is this vagus nerve, and why is it so crucial? Its name comes from the Latin word for “wandering,” and it is the longest and most complex of the cranial nerves. It’s not a single wire but a vast, sprawling network of fibers that serve as the main component of the parasympathetic nervous system—your body’s “rest and digest” counterbalance to the “fight or flight” stress response.
Think of your nervous system as a car. The sympathetic nervous system is the accelerator, revving you up for action. The parasympathetic, largely governed by the vagus nerve, is the brake. It slows your heart rate, stimulates digestion, promotes nutrient absorption, and signals the body to repair and regenerate. It is the physiological state of calm, connection, and restoration.
The vagus nerve’s influence is astonishingly broad:
When your vagus nerve is strong and active—a state known as high vagal tone—you are more resilient to stress. You recover quicker from setbacks, both physically and emotionally. Your digestion is efficient, your mood is more stable, and your body is in a constant state of subtle repair. Low vagal tone, conversely, leaves you stuck in low-grade fight-or-flight: digestion halts, inflammation rises, anxiety persists, and your gut ecosystem begins to suffer. The story of this nerve is the story of your body’s capacity for balance, and as we’ll see, it’s a story we can now learn to read through data.

We all experience acute stress—it’s a survival mechanism. But when stress becomes chronic, a low-grade, persistent background hum, it shifts from a temporary state to a disease-causing condition. This chronic stress acts like a corrosive agent on the delicate wiring and communication of the gut-brain axis, with the vagus nerve as its primary target.
The mechanism is a cascade of physiological misfires. When your brain perceives a threat (whether a looming deadline or a traffic jam), your hypothalamus triggers the release of cortisol and adrenaline. In the short term, these hormones are lifesavers. But under chronic stress, elevated cortisol directly:
The result is a vicious, self-perpetuating cycle. Stress → disrupts gut function → alters microbiota → increases inflammation → sends distress signals to the brain → increases feelings of anxiety and stress. It’s a feedback loop from hell, explaining why conditions like Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD), and chronic anxiety so frequently coexist. You cannot address gut health without addressing stress, and you cannot manage stress effectively without understanding its impact on the gut. Breaking this cycle requires insight, and that insight begins with measurement. This is the core philosophy behind our approach at Oxyzen, where we believe true wellness starts with understanding these hidden connections.
For generations, our understanding of stress was purely subjective. We relied on vague, self-reported feelings of being “overwhelmed,” “anxious,” or “burnt out.” While these feelings are valid, they are imprecise and often recognized too late, after the damage is already underway. The wellness revolution of the past decade has been about moving from subjective feeling to objective data—from counting steps to monitoring heartbeats. Now, we are entering the next frontier: tracking the physiological signature of stress and nervous system balance itself.
Early wearables gave us heart rate. Advanced ones gave us Heart Rate Variability (HRV)—the subtle, millisecond variations in time between each heartbeat. HRV is now widely recognized as one of the most powerful, non-invasive windows into autonomic nervous system function. A higher HRV generally indicates strong vagal tone and good adaptability; your heart can quickly and efficiently respond to changes. A low, rigid HRV suggests your system is stuck in a stressed, inflexible state.
Modern smart rings, like those developed with a focus on comprehensive wellness, take this several steps further. By sitting on a finger rich in capillaries, they can continuously and passively capture a suite of biomarkers:
The power isn’t in any single metric, but in their synthesis. By correlating spikes in resting heart rate with dips in HRV, alongside poor sleep data, the technology doesn’t just tell you you’re stressed—it shows you when, how severely, and in response to what potential triggers (a late meal, a tough workout, a difficult meeting). It translates the invisible language of your nervous system into a clear, actionable dashboard. This objective feedback is the essential first step in breaking the stress-gut cycle, because you can’t manage what you don’t measure. To see how real people have used this data to transform their health, you can explore their journeys in our user testimonials.
To leverage stress tracking, we must understand its cornerstone metric: Heart Rate Variability. It’s a concept that often confuses people—isn’t a steady, metronomic heartbeat a sign of health? In fact, the opposite is true. A healthy heart is dynamically responsive, like a skilled drummer subtly adjusting tempo to the music of your body’s needs.
HRV is the measure of the variation in time between successive heartbeats. If your heart beats exactly 60 times per minute, it’s not beating once every second. The intervals might be 0.95 seconds, then 1.05 seconds, then 0.98 seconds. This variability is controlled by the constant tug-of-war between your sympathetic (“accelerator”) and parasympathetic (“brake,” largely vagus nerve) nervous systems. When your vagus nerve is strong and active (high parasympathetic tone), it injects more variability, creating a higher HRV.
Why is a high HRV desirable?
It’s a marker of resilience and adaptability. It means your body has a wide range of responses to challenge and can efficiently return to baseline afterward. It’s associated with:
What lowers HRV?
Chronic stress is public enemy number one. Other factors include poor sleep, dehydration, overtraining, inflammatory foods, and alcohol. A consistently low HRV is a flashing warning light that your body is under excessive allostatic load and that your vagus nerve may not be getting enough “airtime.”
Smart rings and other advanced wearables calculate HRV (often using the rMSSD or SDNN methods) throughout the night to give you a clean, resting baseline score each morning. This daily number isn’t for day-to-day obsession, but for observing trends. Is your 7-day average climbing? That’s a sign your lifestyle interventions are working. Is it plummeting? It’s an objective cue to prioritize rest, hydration, and stress-management techniques. By making the invisible visible, HRV tracking empowers you to make informed, proactive choices for your nervous system and, by extension, your gut health. For a deeper exploration of how metrics like HRV are captured and interpreted, our FAQ page offers detailed explanations.
The true magic of physiological tracking emerges when you learn to connect the dots between your biometric data and your subjective experience. This is where you move from passive observation to active insight. You become a detective on the case of your own well-being.
Let’s walk through a hypothetical, yet very common, data story:
Another powerful correlation is between nocturnal HRV/dip and next-day digestive comfort. Many users report that on nights when their HRV is particularly low or their sleep is disturbed, they are more likely to experience IBS flare-ups, constipation, or acid reflux the following day. This isn’t coincidence; it’s causality. The body needed the deep, vagus-nerve-dominated state of sleep to repair and regulate the gut, and it didn’t get it.
By journaling brief notes on diet, mood, and digestive symptoms alongside this data, patterns begin to scream from the page. You might discover that your gut isn’t “just sensitive,” but is exquisitely reactive to specific stress patterns that you can now see and, therefore, manage. This process of correlation turns a wellness device into a powerful diagnostic tool for the gut-brain axis.
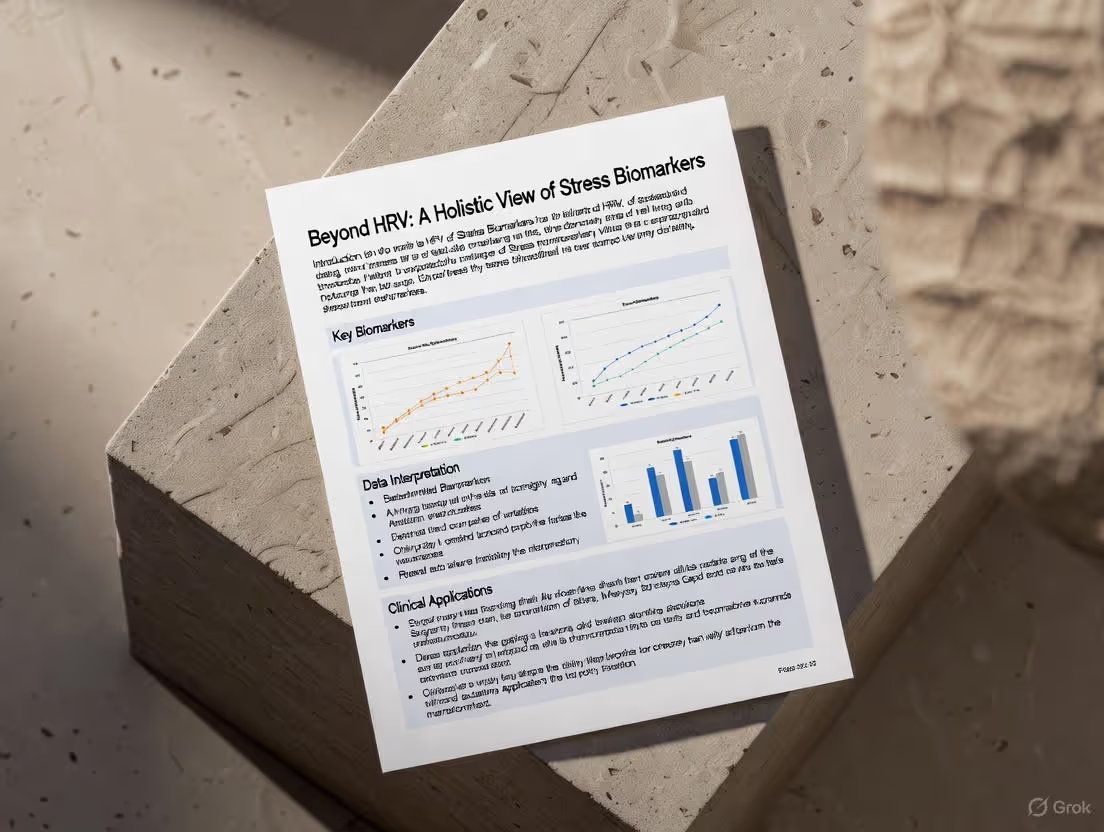
While HRV is the star player in stress and recovery tracking, it doesn’t tell the whole story alone. A comprehensive understanding requires a holistic dashboard of interconnected metrics. Modern smart rings are powerful because they synthesize these data streams to paint a complete picture of your autonomic nervous system state.
Resting Heart Rate (RHR): Your heart’s baseline idle speed. A sustained elevation of 5-10 BPM above your personal norm is one of the clearest objective signs of accumulated stress, poor recovery, or impending illness. It’s your body running its engine too hot, too often.
Sleep Architecture: Stress and poor vagal tone sabotage sleep. Specifically, they rob you of deep (N3) sleep and rapid eye movement (REM) sleep. Deep sleep is critical for physical repair and immune function, while REM is essential for memory consolidation and emotional processing. A device that tracks sleep stages can show you how stress is literally fragmenting your night, depriving your gut and brain of essential repair time.
Respiratory Rate: The number of breaths you take per minute, especially during sleep. Chronic stress often leads to a faster, shallower breathing pattern. An elevated nocturnal respiratory rate is a subtle but significant marker of a nervous system stuck in a heightened state of alert.
Skin Temperature & Blood Oxygen (SpO2): Deviations from your personal baseline in nighttime skin temperature can indicate inflammation or an overactive stress response. Similarly, dips in blood oxygen (nocturnal desaturation) can signal sleep-disordered breathing, which is both a cause and a consequence of stress, and is profoundly disruptive to systemic health.
When you view low HRV + high RHR + poor deep sleep + elevated respiratory rate together, you have an undeniable, multi-faceted biometric signature of a body under siege. This holistic view prevents you from misinterpreting a single data point. It confirms that the issue is systemic—affecting your nervous system, your sleep, your heart, and by direct extension, the environment of your gut. This integrated approach to biometrics is central to our mission at Oxyzen, which you can learn more about in our story.
Armed with the knowledge of how stress disrupts the gut and the data to prove it’s happening, the next logical step is intervention. The goal is not to eliminate stress—an impossible task—but to increase your resilience to it. This means actively working to strengthen your vagus nerve, to enhance your parasympathetic “brake,” and improve your vagal tone. The excellent news is that vagal tone is not static; it’s a trait you can cultivate through daily practice. Your tracking data becomes the feedback loop to see what works for you.
Here are the most potent, evidence-based vagus nerve stimulation techniques:
1. Diaphragmatic (Deep, Slow) Breathing:
This is the most direct and immediate method. Slow, deep breaths with a prolonged exhale directly stimulate the vagus nerve. Aim for a pattern like the 4-7-8 method (inhale for 4, hold for 7, exhale for 8) or simply ensuring your exhale is twice as long as your inhale. This is not “just breathing”; it’s a physiological lever that switches your nervous system state.
2. Cold Exposure:
A brief shock of cold—a 30-60 second cold shower splash or ice-cold water on the face—triggers the “diving reflex,” which immediately stimulates the vagus nerve, slows the heart rate, and promotes a calm, alert state. It’s a powerful, quick reset.
3. Humming, Chanting, and Singing:
The vagus nerve is connected to your vocal cords and the muscles at the back of your throat. Humming, chanting “Om,” or simply singing loudly in the car creates vibrations that directly massage and stimulate the nerve. It’s why these practices are central to many contemplative traditions.
4. Probiotic & Fermented Food Supplementation:
Certain probiotic strains, often called “psychobiotics,” have been shown to positively influence mood and stress response, partly through vagal pathways. Strains like Lactobacillus rhamnosus and Bifidobacterium longum show particular promise in animal and human studies. Consuming fermented foods like kimchi, kefir, and sauerkraut supports a diverse microbiome, which in turn supports healthy vagal signaling.
5. Meditation and Mindfulness:
Regular meditation, particularly loving-kindness (metta) meditation, has been shown to increase HRV and vagal tone over time. It trains the brain to observe stress without being hijacked by it, strengthening the prefrontal cortex’s inhibitory control over the amygdala, the brain’s fear center.
6. Social Connection and Laughter:
Genuine social engagement, warm physical contact (hugs), and deep, belly laughter all promote vagal activity. They signal safety to the nervous system, allowing the “rest and digest” state to flourish.
The key is consistency. A daily 5-minute breathing practice is more powerful than a 30-minute session once a month. Use your smart ring to track the impact: try a breathing exercise before bed and note if your deep sleep increases. Practice morning humming and see if your daytime HRV baseline slowly climbs over weeks. The device provides the proof that empowers the practice.
Strengthening the vagus nerve is one pillar of healing the gut-brain axis. The other is consciously building a lifestyle that creates an internal environment where your gut, and its microbial inhabitants, can thrive. This isn’t about a single “gut health diet,” but about fundamental principles that reduce stress on the system and support its natural rhythms.
Nutrition for the Gut-Brain Axis:
Movement as Medicine:
Regular, moderate exercise is a potent vagus nerve stimulant and gut motility booster. However, overtraining is a massive stressor that crushes HRV and disrupts gut integrity. The goal is consistent, enjoyable movement—brisk walking, cycling, yoga, swimming—not chronic, exhaustive punishment. Let your recovery metrics (HRV, RHR) guide your intensity. A restorative walk on a day of low HRV is far wiser than a high-intensity interval training session.
The Power of Circadian Rhythm:
Your gut and its microbes have their own daily clocks, synchronized by your exposure to light and dark, and by your eating patterns. Disrupting this rhythm (via late-night eating, irregular sleep, or blue light exposure after dark) causes dysbiosis and weakens the gut barrier.
This holistic approach—combining targeted vagal stimulation with a supportive lifestyle—creates a positive, self-reinforcing cycle. A healthier gut reduces inflammation and sends calmer signals to the brain via the vagus nerve, which in turn reduces perceived stress, further improving gut health. It’s the virtuous opposite of the stress-gut doom loop.
We are on the cusp of a transformative shift in preventive health. The future lies not in treating gut disorders or anxiety as isolated conditions, but in integrating continuous physiological data with personalized lifestyle and nutritional insights to preemptively manage the gut-brain axis.
Imagine a not-so-distant scenario: Your smart ring detects a sustained dip in your nightly HRV and a rise in resting heart rate, coupled with a slight increase in nocturnal skin temperature. This triage of data creates a “stress signature.” Instead of you guessing the cause, an integrated AI platform, informed by your personal history and continuous data stream, cross-references this signature.
It might prompt you: *“Your biometrics suggest increased systemic stress and inflammation. This pattern has previously correlated with digestive discomfort for you. Considering your recent travel and dietary changes, here are three personalized suggestions: 1) Prioritize a 10-minute guided vagus nerve reset meditation today. 2) Consider a temporary reduction in fermentable fibers (FODMAPs) for 48 hours to ease gut burden. 3) Your data suggests a probiotic strain shown to support barrier function during travel may be beneficial. Would you like to learn more?”*
This is proactive, personalized, and systems-based healthcare. It moves us from generic wellness advice (“reduce stress, eat well”) to precise, context-aware interventions. The smart ring becomes the always-on guardian of your nervous system, and the insights derived from it guide your daily choices for gut and mental health.
This vision of seamless integration, where technology serves as an intuitive guide to our own biology, is what drives innovation in the wellness tech space. It’s about creating a future where we are no longer passive passengers in our health, but empowered pilots with a full, real-time instrument panel. To stay updated on these evolving possibilities and the technology that enables them, we invite you to follow our blog for the latest insights.
Armed with a foundational understanding of the gut-brain axis and the biomarkers that track its state, the crucial next step is becoming a fluent interpreter of your own data. This is the art of modern self-care: learning to read the subtle signals your body broadcasts 24/7. Vagus nerve dysfunction rarely announces itself with a siren; it whispers through patterns and trends. Here’s how to translate those whispers into actionable insight.
First, establish your personal baseline. Forget population averages. Your optimal HRV might be 35ms, while another person’s is 85ms. What matters is your own range. Use the first month of consistent wear as a data-gathering phase. Note your average morning HRV and resting heart rate during a relatively calm period. This is your “north star.”
Now, watch for these key patterns that suggest your vagus nerve is under siege and your gut may soon protest:
The Stress Overload Pattern:
The Inflammatory Spike Pattern:
The Recovery Deficit Pattern:
The Social-Emotional Correlation:
By learning these patterns, you move from being a passive observer of numbers to an active steward of your nervous system. You begin to anticipate your gut’s needs, intervening with vagus nerve resets and lifestyle tweaks before symptoms manifest. This predictive power is the cornerstone of building true gut resilience. For practical guidance on implementing these insights, our comprehensive FAQ section addresses many common user questions on data interpretation.
We’ve established that the gut microbiota is a key player in the gut-brain axis, but the sophistication of this microbial communication is nothing short of astonishing. It’s not a blunt chemical broadcast; it’s a targeted, nuanced dialogue with the vagus nerve acting as a dedicated secure line.
Beneficial gut bacteria, through their metabolic activities, produce a vast array of neuroactive molecules. Short-chain fatty acids (SCFAs) like butyrate, produced when good bacteria ferment dietary fiber, are powerhouse communicators. Butyrate doesn’t just nourish your colon cells; it:
Conversely, a dysbiotic gut—overrun with less-friendly species—produces a different chemical cocktail. It can generate lipopolysaccharides (LPS), endotoxins from the cell walls of certain bacteria. When the gut barrier is compromised (“leaky gut”), LPS can enter the bloodstream, triggering a systemic inflammatory firestorm. This inflammation is detected by the vagus nerve, which relays the alarm to the brain, contributing to feelings of anxiety, brain fog, and fatigue. It’s a literal “gut feeling” of unease.
Perhaps the most profound example is the production of neurotransmitters. Specific strains of Lactobacillus and Bifidobacterium can produce GABA, the brain’s primary calming neurotransmitter. Others influence serotonin and dopamine pathways. These microbial metabolites don’t cross the blood-brain barrier in large quantities, but they exert powerful effects by binding to receptors on the vagus nerve’s vast network of sensory fibers in the gut wall. The message is then whisked up to the brain at the speed of a nerve impulse, altering neural activity.
This means the state of your inner ecosystem directly dictates the quality of the signals traveling up your vagus nerve to your brain. A diverse, flourishing microbiome sends signals of calm, satiety, and well-being. A depleted, troubled one sends signals of inflammation, threat, and distress. When you use dietary strategies to support your microbiome, you are not just feeding your gut; you are programming the messages your vagus nerve delivers to your mind. This deep, biological interplay is a core focus of modern wellness science, a topic we frequently explore in-depth on the Oxyzen blog.
Irritable Bowel Syndrome (IBS) is perhaps the most clear-cut clinical manifestation of a disrupted gut-brain axis. It’s not a structural disease like Crohn’s, but a disorder of function—and that function is governed by the nervous system. For millions with IBS, stress isn’t just an exacerbating factor; it’s often the primary conductor of the painful symphony in their gut.
Let’s follow “Elena,” a hypothetical but archetypal case. Elena is a 32-year-old project manager diagnosed with IBS-M (mixed type). Her symptoms are unpredictable: alternating bloating, constipation, diarrhea, and abdominal pain, seemingly tied to her work cycle.
The Biometric Story:
The Vagus Nerve Intervention:
Elena, now using her data as a guide, doesn’t wait for full-blown symptoms. Seeing her HRV plummet, she initiates a proactive protocol:
The Outcome:
Within 3-4 days, her biometrics begin to stabilize. HRV climbs back toward her baseline. More importantly, the intensity and duration of her IBS flare are significantly muted. The data gave her an early warning system and a targeted action plan. Over months of using this feedback loop, Elena’s overall symptom frequency decreases. She has moved from being a victim of her unpredictable gut to a manager of her sensitive, but now understood, nervous system.
This case illustrates that for conditions like IBS, the most effective therapy often lies not in stronger gut drugs, but in smarter nervous system regulation. The vagus nerve is the treatment target. This patient-centric, data-informed approach to complex conditions reflects the core vision you can read more about in our company’s story.
Once foundational practices like deep breathing and cold exposure become habitual, you can explore more advanced methods to deepen vagal tone and its gut-healing benefits. These techniques offer more targeted or potent stimulation for those seeking to overcome deeply ingrained stress patterns or more severe gut dysfunction.
1. Transcutaneous Vagus Nerve Stimulation (tVNS):
This is a technology-assisted method gaining significant clinical traction. It involves a small, wearable device that delivers a mild, gentle electrical pulse to the auricular branch of the vagus nerve, located in the outer ear. Studies show tVNS can:
2. Resonance Frequency Breathing (Coherent Breathing):
This takes diaphragmatic breathing to a precise, scientifically optimized level. Everyone has a personal resonance frequency—a breathing rate (typically between 4.5 and 6.5 breaths per minute) that creates perfect synchrony between heart rate, blood pressure rhythms, and breathing, maximizing HRV and vagal influence. Apps and biofeedback devices can help you find your exact frequency. Practicing 10-20 minutes of resonant breathing daily is one of the most potent ways to systematically train your autonomic nervous system toward balance.
3. Gargling and Gag Reflex Stimulation:
Since the vagus nerve innervates the muscles of the soft palate and throat, vigorous gargling with water several times a day can provide a strong stimulus. Similarly, gently activating the gag reflex with a tongue depressor or toothbrush (carefully and without force) can trigger a vagal response. These are less elegant but surprisingly effective mechanical techniques.
4. Probiotic Strains with Direct Vagal Effects:
The science of psychobiotics is advancing rapidly. Specific strains are being identified for their direct impact on the vagus nerve. For example, the strain *Lactobacillus rhamnosus JB-1* was shown in pioneering rodent studies to exert profound anxiety-reducing and behavioral effects—but only in mice with an intact vagus nerve. When the vagus was cut, the benefits vanished. This proves certain probiotics work through this neural pathway. Seeking out supplements containing strains with documented psychoactive properties can be a targeted nutritional strategy.
5. Singing, Chanting, and Playing Wind Instruments:
Advanced, prolonged vocal practices like overtone singing or chanting mantras for extended periods provide deep, sustained stimulation. Similarly, playing a wind or brass instrument (like a didgeridoo, which also trains circular breathing) is a powerful workout for the vagus nerve and has even been studied as a therapy for sleep apnea due to its strengthening effect on upper airway muscles.
Integrating one or two of these advanced practices can be a game-changer, especially when your biometric data shows a plateau in your progress with basic techniques. They represent a deeper commitment to mastering your internal state, a commitment that pays dividends in gut stability and overall resilience.
The field of nutritional psychiatry is built on a simple, powerful premise: the food you eat directly shapes the structure and function of your brain and nervous system, largely via the gut. To heal the gut-brain axis, we must move beyond seeing food as merely calories or gut “fuel,” and instead view it as information and building material for the vagus nerve and the microbiome that influences it.
Key Nutrients for Vagus Nerve and Gut-Brain Health:
The Gut-Brain Plate:
Instead of a restrictive “diet,” think about constructing each meal to support this axis:
This nutritional strategy does three things simultaneously: 1) It provides the raw materials to build and maintain a healthy vagus nerve, 2) It cultivates a microbiome that sends positive signals via that nerve, and 3) It reduces the inflammatory burden that suppresses vagal activity. It’s a triple-action approach to healing from the inside out. For personalized guidance on integrating these principles, our community often shares their experiences and recipes on our blog.
Sleep is not a passive state of inactivity. It is an intensely active period of repair, detoxification, and neural reorganization. For the gut-brain axis, deep sleep is the most critical phase for vagus nerve dominance and gastrointestinal restoration.
During deep (N3) sleep, your parasympathetic nervous system is fully in command. Your heart rate and blood pressure drop to their lowest points, and vagal activity is high. This state of profound physical calm allows for:
When sleep is fragmented or deficient in deep stages, this essential maintenance shift is cut short. The result? A vagus nerve that hasn’t had its full restorative session, a gut lining that is less repaired, and a brain swimming in more metabolic debris. This directly manifests in data: Poor sleep efficiency and low deep sleep percentages are almost invariably followed by lower morning HRV and higher resting heart rate.
Furthermore, sleep deprivation itself is a massive physiological stressor. It elevates cortisol and ghrelin (the hunger hormone) while suppressing leptin (the satiety hormone), creating a double-whammy of increased stress and cravings for high-sugar, high-fat foods that further damage the gut.
Actionable Steps for Vagus-Supportive Sleep:
By prioritizing sleep, you are not just fighting fatigue; you are scheduling a non-negotiable, nightly therapy session for your vagus nerve and your gut. The consistency of this practice is what rebuilds resilience over time. The tangible proof of its importance is visible in your very own recovery metrics each morning.
While nutrition and vagus nerve exercises target the biology of the axis, psychological therapies target the software—the thoughts, beliefs, and conditioned responses that can perpetuate the stress-gut cycle. These therapies are evidence-based methods to “reprogram” maladaptive brain-gut communication.
Cognitive Behavioral Therapy (CBT) for Gut Disorders:
CBT helps individuals identify and change negative thought patterns and behaviors that exacerbate gut symptoms. For someone with IBS, a catastrophic thought like “This pain means something is terribly wrong” can trigger anxiety, which then amplifies pain perception via the gut-brain axis (visceral hypersensitivity). CBT teaches skills to:
Clinical trials show CBT can be as effective as some medications for reducing IBS symptom severity and improving quality of life, precisely because it calms the top-down stress signals from the brain.
Gut-Directed Hypnotherapy:
This specialized form of hypnotherapy, with protocols like the North Carolina Protocol, uses guided imagery and suggestion to directly influence gut function. A therapist might guide a patient to visualize their gut as a calm, smoothly flowing river, or to imagine placing a soothing, warm hand on a painful area of their abdomen. The goal is to bypass the conscious, anxious mind and communicate directly with the enteric nervous system, reducing sensitivity, normalizing motility, and decreasing pain signaling. Remarkably, studies show gut-directed hypnotherapy can produce lasting changes in gut function and even positively influence the microbiome, demonstrating the powerful top-down influence of the mind.
Mindfulness-Based Stress Reduction (MBSR):
Mindfulness trains non-judgmental awareness of the present moment. For gut-brain health, this is revolutionary. It teaches you to observe gut sensations (cramping, bloating) or anxious thoughts without immediately reacting to them with fear or avoidance. This breaks the “sensation → catastrophic thought → anxiety → worsened sensation” feedback loop. By changing your relationship to discomfort, you reduce the secondary suffering—the panic about the pain—which in turn lowers the stress response exacerbating the pain.
These therapies represent the other side of the coin from physiological tracking. Your smart ring data shows you when your nervous system is stressed; these therapies give you the cognitive and emotional tools to change your nervous system’s response. Together, they form a complete treatment package: technology provides the insight, and therapy provides the skills. This integrated model of care—honoring both the physical and the psychological—is the future of managing complex, axis-driven conditions. For those interested in the holistic philosophy behind such integration, you can learn more about our mission and values here.
Knowledge is power, but implementation is transformation. The preceding sections have provided the scientific map; this is your turn-by-turn navigation guide. The following 12-week protocol is designed to systematically reduce stress load, strengthen vagal tone, and cultivate a gut-healing environment. It is progressive, data-informed, and built on the principle of consistency over intensity. Use your biometric data (HRV, RHR, sleep) not as a judgment, but as your primary compass.
Weeks 1-2: The Foundation Phase – Awareness & Baseline
Weeks 3-6: The Building Phase – Habit Stacking & Correlation
Weeks 7-9: The Optimization Phase – Personalization & Refinement
Weeks 10-12: The Integration Phase – Autonomy & Resilience
This protocol is not rigid. If you get sick or face a major life stressor in Week 8, return to the practices of Weeks 1-2. The goal is progress, not perfection. The data from your device is the feedback that keeps this process honest and personalized. It transforms a generic wellness plan into your healing journey.
Healing the gut-brain axis does not happen in a vacuum. You are embedded in a social and physical environment that constantly sends signals to your nervous system. To truly thrive, you must become the architect of an environment that supports, rather than sabotages, your vagus nerve.
The Social Engagement System:
As polyvagal theory elucidates, the ventral vagal state (the state of safety and connection) is the foundation for health. It’s activated by:
The Digital Environment:
Our always-on, hyper-connected digital world is a minefield for the autonomic nervous system.
The Physical Environment:
By consciously designing your social circles, digital habits, and physical spaces, you create a “pro-vagal” ecosystem. This reduces the daily burden on your nervous system, making the active work of breathing, meditation, and nutrition even more effective. It’s about creating a life that doesn’t constantly demand recovery, but that inherently fosters balance. For inspiration on building a holistic wellness lifestyle, our community shares their environmental tips and journeys on our blog.
The path to healing is rarely linear. Expect plateaus, setbacks, and confusing data. How you navigate these is what determines long-term success. Here are common challenges and strategic responses.
Pitfall 1: Data Obsession and “Good Day/Bad Day” Thinking.
Pitfall 2: The “Doing Everything Right” Plateau.
Pitfall 3: Inconsistency and the “All-or-Nothing” Mindset.
Pitfall 4: Ignoring Subjective Feelings for Objective Data.
The journey is iterative. It requires curiosity, self-compassion, and the willingness to be a detective in your own life. Your biometric device is your lab partner, providing clues. Your task is to interpret them with wisdom and patience. For support and to see how others have overcome similar hurdles, our FAQ and community testimonials offer a wealth of shared experience.
We are standing at the dawn of a new paradigm in healthcare—one that moves from treating isolated symptoms to optimizing the core regulatory system of the body: the autonomic nervous system, with the vagus nerve as its centerpiece. The convergence of consumer biometrics, artificial intelligence, and advanced neuroscience is making this future tangible.
Next-Generation Biofeedback:
Imagine a smart ring that doesn’t just record your HRV, but provides real-time vagal tone feedback. As you practice your breathing, a gentle haptic pulse on your finger synchronizes with your exhale, guiding you into your optimal resonance frequency. The device learns your personal stress signatures and can prompt you with a customized, micro-intervention: “Your breathing pattern suggests rising stress. Try 90 seconds of humming now.”
AI-Powered Personal Health Assistants:
Platforms will integrate data from your ring, your food log, your calendar, and even your voice tone analysis to build a holistic model of your gut-brain axis health. It could predict: *“Based on your lowered HRV trend, elevated evening cortisol logs, and tomorrow’s packed schedule, you have an 82% likelihood of an IBS flare. Suggested protocol: Take your probiotic with breakfast, schedule two 5-minute breathing breaks at 11am and 3pm, and opt for the low-FODMAP lunch option.”* This moves us from reactive to genuinely predictive and preventive care.
Closed-Loop Neuromodulation:
Building on tVNS, future devices may become “closed-loop.” They would continuously monitor a biomarker like heart rate or HRV and deliver a precisely timed, subtle vagus nerve stimulus only when needed to nudge the nervous system back toward balance, all without conscious effort from the user. This could be a revolutionary tool for managing conditions like epilepsy, depression, and inflammatory diseases rooted in autonomic dysfunction.
Microbiome-Vagus Nerve Sequencing:
As microbiome science advances, we may see personalized probiotic and prebiotic formulations designed not just for gut composition, but for their specific neuroactive metabolite profiles—formulations engineered to optimize the chemical messages sent up the vagus nerve to support calm, focus, or resilience based on an individual’s genetic and lifestyle needs.
This future is not about replacing human intuition or the therapeutic relationship; it’s about augmenting it with unprecedented clarity. It democratizes access to deep physiological insight, putting the power to understand and influence the gut-brain axis directly into the hands of individuals. It represents a shift from a healthcare system that waits for you to break, to a wellness ecosystem that helps you optimize and thrive. This vision of empowered, data-informed well-being is at the heart of what drives innovation, a vision you can explore further in our company’s narrative.
Our journey through the labyrinth of the gut-brain axis brings us to a profound and simple truth: you are not a collection of separate systems. You are an integrated, dynamic conversation. The stress you feel, the data you track, the food you digest, and the thoughts you think are all participants in a continuous dialogue mediated by the wandering vagus nerve.
Chronic stress disrupts this dialogue, turning a symphony into cacophony. It manifests as anxiety in the mind, inflammation in the body, and dysfunction in the gut. But this is not a life sentence. The very existence of this intimate connection—the gut-brain axis—is also the source of our healing. It means we have multiple points of intervention. We can calm the mind to soothe the gut. We can nourish the gut to quiet the mind. We can exercise the vagus nerve to enhance the quality of the entire conversation.
The advent of sophisticated, accessible biometric tracking is the game-changer. It allows us to move from guessing to knowing. It transforms the vague sense of being “stressed and bloated” into a clear understanding of how a stressful Tuesday suppressed your vagal tone, spiked your heart rate, and led to Wednesday’s digestive distress. This objective feedback loop ends the cycle of frustration and self-blame. It replaces it with agency.
The protocol outlined here is not a quick fix. It is a pilgrimage back to your own biological rhythm. It is the deliberate cultivation of a resilient nervous system and a flourishing inner ecosystem. Some days you will have the energy for cold plunges and elaborate meals. Other days, your win will be a five-minute breathing session before bed. Both are valid. Both strengthen the connection.
Start where you are. Use what you have. Breathe deeply. Nourish intentionally. Connect meaningfully. Sleep restoratively. And let your data be the gentle, objective guide on your path to wholeness. The goal is not to never experience stress again, but to build a system so resilient that stress becomes a wave you surf, not a tsunami that drowns you.
Your gut feelings are real. Your body’s data is telling a story. It’s time to listen, to connect the dots, and to reclaim the vibrant health that arises when your brain, your gut, and the vital nerve that connects them are finally speaking the same, harmonious language. For continued support, deeper dives into each of these topics, and a community of like-minded individuals on the same journey, we invite you to become a part of our growing resource hub at the Oxyzen blog.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/