The Relationship Between Sleep Stages and Body Temperature
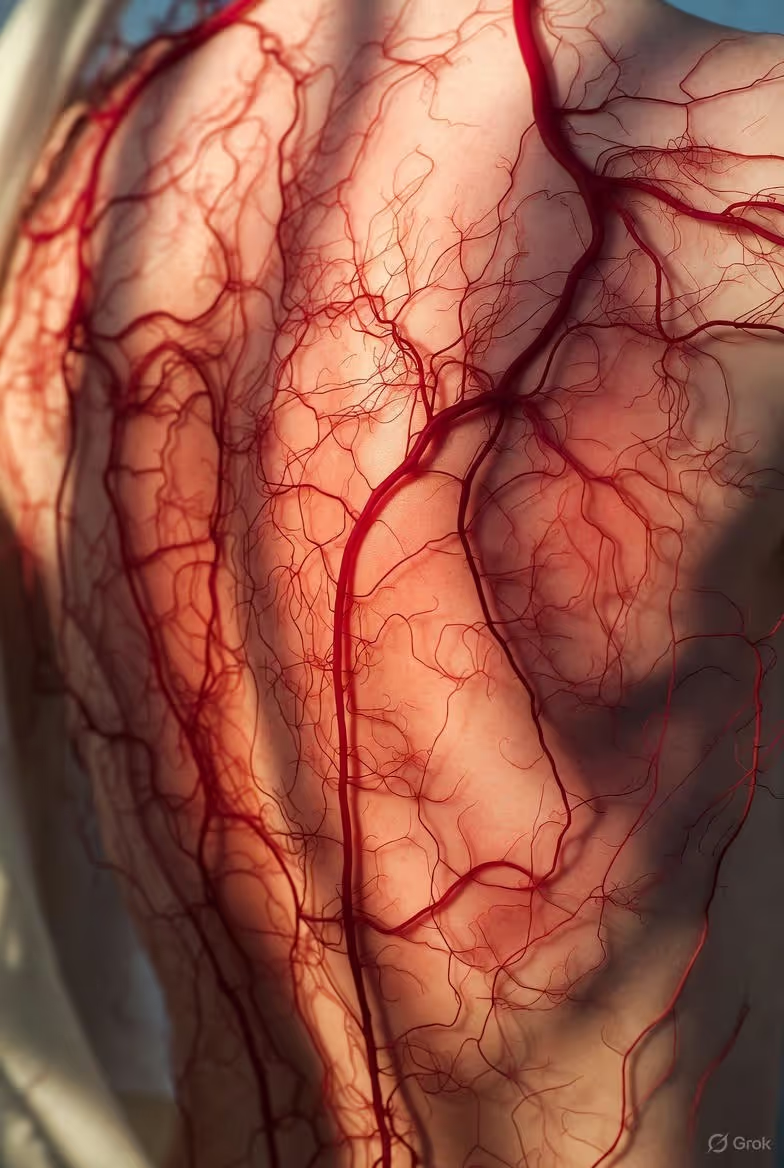
The body's core temperature cycle is tightly linked to the sleep-wake cycle, dropping to facilitate sleep onset and deep sleep.
The body's core temperature cycle is tightly linked to the sleep-wake cycle, dropping to facilitate sleep onset and deep sleep.
Have you ever tossed and turned on a hot summer night, desperately chasing a cool spot on the pillow? Or curled into a tight ball, shivering under the covers, unable to drift off? These common experiences are more than just minor discomforts—they are glaring signs of a fundamental, biological truth: sleep and body temperature are locked in an intricate, inseparable dance.
For centuries, we’ve understood sleep as a passive state, a simple absence of wakefulness. But modern science reveals it as a dynamic, highly orchestrated physiological process, and at the very center of this nightly performance is the careful regulation of your core temperature. This relationship is not a mere correlation; it is a causal mechanism. Your body’s internal thermostat doesn’t just adjust during sleep—it actively initiates it, guides its progression, and ultimately signals its end.
Every night, as you journey through the distinct stages of light sleep, deep sleep, and dream-rich REM sleep, your body undergoes a precise thermal ballet. A subtle, pre-sleep drop in core temperature is your biological invitation to slumber. This cooling trend continues as you plunge into the restorative depths of slow-wave sleep. Then, in a fascinating twist, during REM sleep, your body’s ability to thermoregulate is almost entirely switched off, leaving you as vulnerable as a reptile to the environment. This cyclical pattern is as crucial to your health as the sleep stages themselves.
Understanding this relationship is no longer just academic. It is the key to unlocking profoundly better sleep, recovery, and overall wellness. With the advent of wearable technology like advanced smart rings, we can now move beyond guessing and into the realm of precise, personalized insight. Devices such as the Oxyzen smart ring track subtle physiological signals, including distal body temperature, offering a window into this hidden rhythm. By decoding the language of your body’s nightly temperature cycle, you gain the power to optimize your environment, habits, and ultimately, your health. This journey into the thermal heart of sleep begins with a fundamental question: what, exactly, is orchestrating this complex, vital performance?

At the helm of your sleep-wake cycle, and intrinsically tied to your body temperature, is a master conductor known as your circadian rhythm. This 24-hour internal clock, residing within the suprachiasmatic nucleus (SCN) of your brain’s hypothalamus, governs the temporal pattern of virtually every physiological process in your body—from hormone release and metabolism to the critical ebbs and flows of alertness and sleepiness. It is the foundational metronome to which your sleep-temperature dance is set.
Your circadian rhythm is endogenously generated, meaning it runs on its own intrinsic, roughly 24-hour schedule. However, it is exquisitely sensitive to external cues, primarily light and darkness, which synchronize or “entrain” it to the solar day. When light enters your eyes, specialized cells signal the SCN, which then suppresses the production of melatonin, the “hormone of darkness,” and promotes wakefulness. As evening falls and light diminishes, the SCN signals the pineal gland to release melatonin, easing you toward sleep.
Here is where temperature plays its first pivotal role. Your core body temperature does not remain constant throughout the day; it follows a distinct circadian wave. Typically, it begins to rise in the early morning, continues to increase throughout the day, peaks in the late afternoon or early evening, and then—crucially—begins a steady decline about 1-2 hours before your habitual bedtime. This pre-sleep降温 is not a passive cooling but an active process driven by your circadian system. Blood vessels in your skin dilate (a process called vasodilation), particularly in your hands and feet, increasing blood flow to the body’s surface to radiate heat away from the core. This is why you might notice your hands and feet feel warmer as you get sleepy—they are acting as radiators to cool your central engine.
The minimum point of your core body temperature rhythm usually occurs in the second half of your night’s sleep, around 4-5 AM. From that nadir, it begins its slow climb back up, a rise that contributes to the increasing likelihood of waking as morning approaches. This temperature rhythm is so robust that it persists even in the absence of sleep, and sleep deprivation studies show that the drive to sleep is strongest at the circadian temperature minimum.
Understanding this master clock is the first step to hacking your sleep. Disruptions to this rhythm—such as those caused by jet lag, shift work, or excessive blue light exposure before bed—directly disturb the thermal signaling for sleep onset. You can feel tired, but if your core temperature hasn’t begun its descent, falling asleep will be a struggle. This is why maintaining a consistent sleep schedule is so powerful; it strengthens the circadian signal for that critical evening cool-down. For those looking to dive deeper into the science of circadian health and practical synchronization strategies, our comprehensive resources on the Oxyzen.ai blog offer a wealth of actionable guidance.
The circadian rhythm sets the stage, but it is not the only player. Another powerful, sleep-specific force builds throughout the day, interacting with your internal clock to determine the precise moment you succumb to slumber.

While your circadian rhythm provides the when—the scheduled timing of sleep—another biological system governs the need—the mounting pressure to sleep based on how long you’ve been awake. This system is called sleep homeostasis, and its primary chemical messenger is adenosine.
Adenosine is a neuromodulator that accumulates in your brain, particularly in the basal forebrain, with every waking hour. Think of it as a natural sleep “debt” molecule. As you expend mental and physical energy throughout the day, adenosine levels steadily rise, increasing your feeling of sleep pressure, or homeostatic sleep drive. This drive builds until it becomes a powerful force compelling you to sleep.
The fascinating intersection between homeostasis and circadian rhythm is where the magic of sleep initiation happens. In the evening, as your circadian-driven signal for sleepiness rises (coinciding with the drop in core temperature), it converges with the high level of adenosine-driven sleep pressure. This dual-system peak creates the optimal window for easy, rapid sleep onset. In the morning, the opposite occurs: your circadian alerting signal strengthens, core temperature begins to rise, and adenosine has been cleared away during sleep, resulting in refreshed wakefulness.
Crucially, adenosine and body temperature are not independent actors. Research indicates that adenosine may play a role in facilitating the pre-sleep drop in core temperature. It influences the thermoregulatory centers in the hypothalamus, promoting the vasodilation needed for heat loss. Furthermore, sleep itself, particularly deep non-REM sleep, is the primary mechanism for clearing adenosine from the brain. This creates a beautiful, self-regulating loop: rising adenosine promotes sleep and cooling; sleep clears adenosine and allows temperature to reach its nadir; waking begins the cycle anew.
This is why substances that block adenosine receptors, like caffeine, are such potent disruptors of sleep. They artificially dampen the feeling of sleep pressure, but they do not stop its accumulation or its interaction with your thermal rhythm. You may feel alert, but your body’s underlying need for sleep and its thermal preparation for it are still in motion, leading to a mismatch that can result in lying awake with a "tired but wired" feeling.
The homeostatic system explains why, after a poor night’s sleep, the pressure to sleep the next night is stronger. It also highlights the non-negotiable nature of sleep debt. While you can somewhat influence your circadian timing with light, the homeostatic drive must be paid with sleep. Tracking this balance is a complex task, but it’s one that modern technology is making accessible. By monitoring physiological markers like temperature variability and heart rate, devices like the Oxyzen smart ring can provide insights into how these two systems—circadian and homeostatic—are aligning in your own body, a topic we explore in detail for our community at Oxyzen.ai.
With the stage set by these two governing systems, we can now step into the theatre of the night itself and witness how temperature changes define the very architecture of sleep.

Sleep is not a monolithic state of unconsciousness. It is a carefully structured progression through distinct stages, each with unique brain wave patterns, physiological characteristics, and, as you may have guessed, thermal profiles. These stages cycle every 80 to 120 minutes throughout the night, in a pattern known as sleep architecture. The two primary types of sleep are Non-Rapid Eye Movement (NREM) sleep and Rapid Eye Movement (REM) sleep.
NREM Sleep is further divided into three stages, progressing from light to deep sleep:
REM Sleep typically occurs after a period of NREM sleep, about 90 minutes after falling asleep.
The proportion of these stages shifts throughout the night. The first half of the night is dominated by deep N3 sleep, crucial for physical restoration. As the night progresses, REM sleep periods become longer and more frequent, while N3 sleep diminishes. This architecture is not rigid; it is dynamically shaped by age, prior sleep history, and external factors. But running through all of it, like a colored thread through fabric, is the changing pattern of your body’s thermoregulation. To understand your own unique sleep architecture, consistent tracking is key. Many users of the Oxyzen smart ring share in our testimonials how seeing their sleep stages visualized has transformed their approach to nightly recovery.
Now, let’s trace the thermal narrative that unfolds across this architectural landscape, beginning with the very first signal that tells your brain it’s time to shut down.
The journey into sleep is not an abrupt switch but a gradual descent, and the first step on that path is a deliberate, physiological cool-down. Approximately 60 to 90 minutes before your natural bedtime, your body initiates a proactive drop in core temperature. This pre-sleep dip, orchestrated by the circadian rhythm, is arguably one of the most potent natural sleep signals you have.
The mechanism is one of heat redistribution. Your core temperature—the temperature of your vital organs—needs to decrease by about 1-2 degrees Fahrenheit (0.5-1 degree Celsius) to initiate and maintain sleep. To achieve this, your body increases blood flow to the extremities—your hands, feet, and skin surface. The blood vessels in these areas dilate, a process called distal vasodilation. Warm blood from your core flows to these “radiators,” where heat is dissipated into the environment. This is why, paradoxically, having warm hands and feet (indicating good blood flow) actually helps you cool down your core and fall asleep faster.
This process is highly sensitive to environmental and behavioral cues:
When this thermal signal is disrupted, sleep initiation falters. Insomniacs often show a blunted or delayed pre-sleep temperature drop. Their bodies fail to efficiently shift heat from the core to the periphery, leaving them in a state of physiological “readiness” incompatible with sleep.
Harnessing this knowledge is a powerful tool. It moves “sleep hygiene” from a list of abstract rules to a science of thermal management. Creating a routine that supports distal vasodilation—a cool room, warm feet (with socks if needed), and avoiding late thermal stressors—can be transformative. For individuals seeking to optimize this process with data, tracking the subtle nighttime temperature trends with a wearable device provides unparalleled feedback, a principle central to the design philosophy behind Oxyzen. As you successfully traverse this thermal gateway into sleep, you immediately begin the descent into its most physically restorative phase.

Once you cross the threshold from wakefulness into sleep, the thermal narrative continues to deepen, literally and figuratively. As you progress through the lighter N1 and N2 stages and into the profound depths of N3 slow-wave sleep, your body’s thermoregulatory precision remains impressively intact—but with a clear goal: to reach and maintain a lower thermal set point.
During NREM sleep, and particularly in deep N3 sleep, your body’s hypothalamic thermostat is not only functional but actively engaged in promoting a cooler internal state. The heat loss initiated during the pre-sleep dip continues and stabilizes. Core body temperature continues its gradual decline, reaching its lowest point typically during the later sleep cycles, in the early morning hours.
This co-occurrence of deep sleep and lowered temperature is not a coincidence; it is a synergistic relationship critical for restoration:
Your body maintains this cool, stable state through precise autonomic control. If you begin to get too cold, mechanisms like vasoconstriction (narrowing blood vessels in the skin) can be engaged even while asleep to conserve heat. If you get too warm, vasodilation and sweating are the primary responses. This is why the quality of your deep sleep is so dependent on a stable, cool sleep environment. A room that is too hot can prevent you from reaching the optimal thermal set point for deep sleep, fragmenting this crucial stage and leaving you feeling unrefreshed.
The integrity of NREM thermoregulation is a hallmark of healthy sleep. Disruptions, such as those caused by sleep disorders like sleep apnea, can be detected in part by abnormal temperature and heart rate patterns during this phase. By monitoring these subtle physiological shifts, modern wellness technology provides a window into the depth and quality of your restorative sleep, a topic frequently discussed in our FAQ by users curious about what their data means. After the profound, cool restoration of deep sleep, the brain prepares for a dramatic and thermally chaotic shift.
If NREM sleep is a state of precise thermal regulation, REM sleep is its polar opposite—a period of profound thermoregulatory chaos. During REM sleep, your body undergoes a fascinating and potentially vulnerable transformation: it becomes largely poikilothermic.
Poikilothermy, often associated with reptiles, describes an organism’s inability to internally regulate its body temperature; it fluctuates with the environment. During REM sleep, humans exhibit a form of this. The brain’s primary thermoregulatory responses—shivering to generate heat and sweating to cool down—are effectively switched off. Your body loses the ability to maintain a constant core temperature in the face of environmental challenges.
This paradoxical state is a result of the intense brain activity and muscle atonia that define REM sleep. The neural pathways that control thermoregulation are believed to be inhibited, perhaps to preserve the brain’s energy for the intense cognitive processes of dreaming and memory consolidation, and to ensure the paralysis necessary to keep you from acting out dreams.
The consequences of this are significant:
This thermal paradox underscores why a consistently controlled sleep environment is non-negotiable for quality sleep. The temperature that helped you fall asleep and nurtured deep sleep must remain stable to protect the fragile, environmentally sensitive REM periods that dominate the latter half of the night. The discovery of this REM poikilothermy was a landmark in sleep science, revealing just how complex and vulnerable the sleep process is. It’s insights like these that drive our mission at Oxyzen, detailed in our story, to create technology that helps guard these delicate biological processes. As the night cycles between thermal precision and thermal chaos, another key player enters the scene to modulate the entire process.
The circadian and homeostatic systems don’t operate in a vacuum; they express their commands through a powerful endocrine (hormonal) orchestra. Two key conductors in this symphony, melatonin and cortisol, have a direct and profound influence on body temperature and, consequently, on the structure of your sleep.
Melatonin: The Cooling Hormone of Darkness
Often called the “hormone of sleep,” melatonin’s role is more precisely that of a “hormone of darkness” or a circadian timing signal. Its primary function is to convey information about the light-dark cycle to bodily systems. As daylight fades, the SCN directs the pineal gland to release melatonin. This surge does not put you to sleep outright but opens the “sleep gate” by promoting conditions conducive to sleep—most notably, by lowering core body temperature.
Melatonin facilitates the pre-sleep dip by enhancing peripheral vasodilation. It acts on the blood vessels in your skin, particularly in the hands and feet, to promote heat loss. This is why supplemental melatonin, when timed correctly, can be effective for circadian rhythm disorders like jet lag or shift work sleep disorder—it helps realign the thermal preparation for sleep with a new desired bedtime. However, its effect is subtle and works best in conjunction with proper light hygiene.
Cortisol: The Warming Hormone of Awakening
Cortisol, often labeled the “stress hormone,” follows a robust circadian rhythm inversely related to melatonin. It is at its lowest point around midnight, begins to rise in the early morning hours (around 2-4 AM), and peaks shortly after waking—a phenomenon called the Cortisol Awakening Response (CAR). This morning surge is crucial for promoting alertness, mobilizing energy, and, relevantly, raising core body temperature.
The rising cortisol level in the second half of the night contributes to the gradual increase in core temperature from its nadir. This thermal climb, alongside the clearing of adenosine, helps bring you closer to the threshold of wakefulness with each sleep cycle. It’s part of the reason why your final REM period often occurs just before you wake up—the brain is in a more active, “near-wake” state. Dysregulation of this rhythm, such as elevated nighttime cortisol due to chronic stress, can directly interfere with the cooling needed for sleep onset and maintenance, leading to fragmented sleep and early morning awakenings.
This hormonal-thermal interplay is a perfect example of the body’s integrated systems. It’s not that one causes the other in a linear way; rather, melatonin secretion, cortisol suppression, core temperature drop, and sleep onset are all simultaneous, coordinated outputs of a healthy circadian system operating in a dark environment. Optimizing this symphony involves managing light exposure, stress, and timing—principles that form the cornerstone of modern sleep science and are a constant focus for content and tools shared on the Oxyzen.ai blog.
While hormones set the rhythm, the physical structure through which temperature is managed—the skin and its blood vessels—plays the most direct and dynamic role of all.
The abstract concepts of core cooling and heat loss are made tangible through a simple, elegant physiological process centered on your skin and circulatory system. Your skin is not just a covering; it is your body’s primary thermoregulatory organ, and its state dictates the success of your sleep initiation.
At the heart of this is the balance between vasoconstriction and vasodilation.
The shift from vasoconstriction to vasodilation, particularly in the extremities (hands, feet, and ears)—a process called distal vasodilation—is the physical execution of the pre-sleep cooling command. When your circadian clock signals that it’s time to sleep, it triggers this vascular change. Warm blood from your core circulates to the skin’s surface in your hands and feet. Because these areas have a high surface area-to-volume ratio, they are exceptionally efficient radiators.
This is why monitoring distal temperature can be such a powerful proxy for understanding sleep readiness and quality. A rise in skin temperature on the fingers or toes in the evening is a direct indicator of vasodilation and, therefore, of the body’s active attempt to cool the core for sleep. Conversely, cold hands and feet at bedtime suggest vasoconstriction is still dominant, signaling that your body is not yet in a sleep-ready thermal state.
Modern smart rings, worn on the finger, are uniquely positioned to capture this signal. By tracking the subtle temperature changes of the finger skin throughout the night, they can infer the timing and effectiveness of your body’s vasomotor activity. This data can reveal:
Having explored the intricate internal dance between sleep stages and temperature, we now arrive at the most practical and powerful lever you can pull: your sleep environment. Your bedroom is not merely a place you sleep; it is a critical life-support system for your circadian rhythm and homeostatic processes. Optimizing it for thermal harmony is the single most effective action you can take to translate this complex biology into tangible, restorative sleep.
The cornerstone of this environment is ambient air temperature. The scientific consensus points to a relatively cool room—typically between 60-67°F (15.5-19.5°C)—as optimal for most people. This range is not arbitrary. It is the thermal "Goldilocks zone" that facilitates the core body cooling process without triggering a defensive stress response. A room within this range:
However, ambient temperature is just the starting point. The concept of "thermal load" encompasses all factors that add or remove heat from your body. Your bedding is a primary component of this equation.
Bedding as a Thermoregulatory Tool:
Your mattress, pillows, sheets, and blankets create a microclimate around your body. The goal is to choose materials that aid temperature regulation rather than fight it.
Technology and the Modern Sleep Sanctuary:
We no longer have to rely on guesswork and static thermostats. A suite of "sleep tech" can actively manage your thermal environment:
Creating your sanctuary is an iterative process of observation and adjustment. The data from a wearable device can be invaluable here. By correlating nights of reported good sleep with recorded room temperature and your own distal temperature trends, you can pinpoint your personal ideal. This empirical approach takes the guesswork out of creating a truly restorative space, a principle we champion in our resources at Oxyzen.ai.
Your environment sets the stage, but your daily behaviors are the actors that either harmonize with or disrupt the thermal rhythm of sleep.
Your body’s thermal readiness for sleep is not determined in the hour before bed; it is cultivated throughout the entire waking day. From the moment you open your eyes, your choices—regarding light, food, movement, and stress—send cascading signals to your hypothalamus, shaping the slope and timing of your evening temperature drop. Mastering these daytime habits is the art of thermal sleep hygiene.
Light: The Prime Synchronizer
Light exposure is the most potent cue for your circadian clock, and thus, for your temperature rhythm.
Nutrition and Meal Timing: The Thermic Effect
The process of digesting food—the thermic effect of digestion—increases core body temperature and metabolic rate.
Exercise: A Double-Edged Sword
Physical activity is a powerful modulator of body temperature and sleep architecture, but timing is everything.
Stress and the Overheated Mind
Psychological stress activates the sympathetic nervous system (the "fight-or-flight" response), which is fundamentally incompatible with the parasympathetic-driven state needed for sleep. Stress elevates cortisol at the wrong times and promotes peripheral vasoconstriction, directly opposing the vasodilation required for sleep onset. Chronic stress can effectively "overheat" your physiological state, making it impossible to achieve the cool, quiescent state of sleep. Practices like mindfulness, meditation, and controlled breathing are not just mental exercises; they are thermal therapies that promote the vascular shift necessary for sleep.
Integrating these habits creates a daylong runway for an effortless thermal landing at bedtime. For those navigating the complexities of shift work, jet lag, or modern digital life, detailed strategies to realign these rhythms can be found in our curated content on the Oxyzen.ai blog. Sometimes, despite our best efforts, our body's own thermal signaling can go awry, pointing to deeper health issues.
The exquisite precision of the sleep-temperature relationship means that when sleep breaks down, thermal dysregulation is often both a cause and a symptom. Several clinical sleep disorders manifest clear disruptions in normal body temperature patterns, offering both diagnostic clues and avenues for novel treatments.
Insomnia and a Blunted Thermal Signal
Individuals with chronic insomnia often exhibit a fundamental dysregulation in their circadian thermal rhythm. Research using core body temperature monitoring has consistently shown:
This creates a vicious cycle: anxiety about sleep increases sympathetic arousal (and vasoconstriction), which prevents cooling, which prevents sleep, which increases anxiety. Interventions like Temperature-Biofeedback Therapy and Cognitive Behavioral Therapy for Insomnia (CBT-I) can help break this cycle by teaching individuals to recognize and promote the physiological sensations associated with cooling and relaxation.
Sleep Apnea and the Strain of Fragmentation
Obstructive Sleep Apnea (OSA), characterized by repeated pauses in breathing during sleep, causes severe sleep fragmentation and intermittent hypoxia (low oxygen). This constant arousal has a dramatic effect on thermoregulation:
Restless Legs Syndrome (RLS) and Peripheral Discomfort
RLS is characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations, that worsens at rest and in the evening. While its primary mechanism is dopaminergic, a thermal component is well-established:
Night Sweats and Hormonal Shifts
While not a disorder per se, severe night sweats are a common symptom of thermal dysregulation, most notably during menopause due to declining estrogen. Estrogen influences the hypothalamic thermostat; its fluctuation can cause the set point to become unstable, triggering inappropriate vasodilation and sweating (a hot flash) to cool a body that isn't actually overheated. This can occur during sleep, causing profound disruptions.
Understanding these disorders through the lens of temperature underscores that sleep is a whole-body physiological state. For individuals struggling with sleep, tracking nocturnal temperature trends can provide objective data to bring to a healthcare provider, moving the conversation beyond subjective description. It’s this potential for empowerment through data that lies at the heart of our mission at Oxyzen, which you can learn more about in our story. While disorders represent a breakdown of the system, at the other end of the spectrum, we can leverage this knowledge to not just sleep, but to sleep better—enhancing recovery and performance.
For athletes, biohackers, and anyone seeking to maximize their waking potential, sleep is the ultimate performance-enhancing drug. And within sleep, the thermal dimension offers a sophisticated toolkit for deepening restorative processes, accelerating recovery, and fine-tuning cognitive function. This is the frontier of applied thermophysiology.
Targeted Temperature Manipulation for Deep Sleep Enhancement
Deep NREM sleep is the cornerstone of physical repair. Since this stage is associated with the lowest core temperatures, could proactive cooling enhance it?
Cognitive Detoxification and Brain Temperature
The discovery of the glymphatic system has revolutionized our understanding of sleep’s role in brain health. This waste-clearance system is most active during deep NREM sleep. While research is ongoing, the leading hypothesis suggests that the slight reduction in brain temperature and the changes in blood flow during this stage may facilitate the efficient flushing of metabolic byproducts like beta-amyloid. Therefore, strategies that promote robust, cool, deep sleep are not just about feeling sharp tomorrow; they are potential long-term investments in cognitive resilience.
Chronotype Optimization and Personal Thermal Curves
Not everyone’s thermal rhythm is identical. Your chronotype—whether you’re a natural "lark" (morning type), "owl" (evening type), or somewhere in between—is reflected in your temperature curve. Owls typically have a later temperature peak and a later temperature minimum than larks.
The Future: Personalized Thermal Sleep Profiles
The convergence of continuous physiological monitoring (via rings, patches, or bedding) and machine learning is paving the way for truly dynamic sleep environments. Imagine a system that:
For millennia, our understanding of sleep was limited to subjective experience: how long it took to fall asleep, how many times we woke, and how we felt in the morning. The relationship with body temperature was felt, not measured—a vague sensation of being too hot or too cold. Today, we are in the midst of a silent data revolution. Wearable technology, particularly the advent of advanced smart rings and sensors, is acting as a translator, decoding the hidden language of our nocturnal physiology and making the intricate dance between sleep and temperature visible for the first time.
At the forefront of this revolution is the ability to track distal body temperature continuously and unobtrusively. Unlike core temperature, which requires invasive or highly inconvenient measurement (e.g., rectal probes, ingestible pills), distal temperature—the temperature of your skin, particularly on extremities like your fingers—provides a powerful and accessible proxy. As we've established, the rise and fall of skin temperature on your finger is a direct readout of vasodilation and vasoconstriction, the very processes that regulate core cooling for sleep.
How Wearables Capture the Thermal Narrative:
Modern smart rings, worn on the finger, are uniquely positioned for this task. They employ sensitive infrared sensors and thermistors to monitor the skin temperature of the finger 24/7. This data stream is then processed through sophisticated algorithms that filter out "noise" (like momentary changes from handling a cold glass) and identify meaningful patterns:
But temperature is rarely interpreted in isolation. Its true power is unlocked through multi-modal sensing. The most insightful devices combine temperature data with other key physiological signals:
By fusing these data streams, the wearable creates a rich, multi-dimensional picture of your sleep physiology. It's not just telling you that you slept poorly; it's offering clues as to why. Was your distal temperature high and unstable all night, suggesting an overly warm room? Did your temperature fail to drop at your usual time, indicating a delayed circadian rhythm from late screen exposure? This is the shift from descriptive tracking to diagnostic insight.
From Raw Data to Actionable Wisdom:
The value isn't in the gigabytes of data collected; it's in the translation. The best platforms don't just show graphs; they provide contextual interpretation and personalized feedback.
This feedback loop is transformative. It empowers you to become a scientist of your own sleep, running gentle experiments (cooler room, earlier dinner, no evening alcohol) and observing the objective results in your physiological data. It moves wellness from prescriptive to participatory. For those eager to understand the full capabilities and science behind this kind of tracking, our detailed FAQ addresses the most common questions from our community of data-informed users.
As this technology evolves, it is not only changing individual habits but also reshaping entire industries, from professional sports to corporate wellness.
The implications of understanding the sleep-temperature nexus extend far beyond the individual seeking a better night's rest. This knowledge is rippling through sectors as diverse as elite sports, healthcare, workplace design, and even architectural engineering, driving a new appreciation for sleep as a pillar of human performance and safety.
Elite Athletics and Precision Recovery
For professional athletes, sleep is the ultimate legal performance enhancer. Teams and organizations are now investing heavily in sleep science, with temperature management as a core component.
Healthcare and Chronic Disease Management
The bidirectional link between sleep dysregulation and chronic disease is well-established. Temperature tracking offers a new vital sign for long-term health monitoring.
Corporate Wellness and Human Performance
Forward-thinking companies are recognizing that exhausted, sleep-deprived employees are less safe, less creative, less collaborative, and more prone to error and illness. Investing in sleep literacy is becoming a competitive advantage.
The Built Environment: Architecture for Sleep
Our ancestors slept in environments largely dictated by the natural thermal cycle of the outdoors. Modern HVAC has liberated us, but often without consideration for sleep biology. A new field of "neuroarchitecture" is considering how building design affects occupant health.
This broad adoption signifies a paradigm shift: sleep is no longer viewed as personal downtime but as a critical, measurable component of human capital, safety, and longevity. The companies leading this charge, like Oxyzen, are driven by a mission to make this science accessible, as detailed in our foundational our story. With this expansive view in mind, let's cast our gaze forward to where this convergence of biology and technology is headed next.
Our understanding of the sleep-temperature relationship, while already deep, is far from complete. Cutting-edge research is pushing the boundaries, exploring novel connections, developing innovative interventions, and raising profound ethical questions. The future of sleep science is not just about measuring more data, but about understanding more deeply and intervening more precisely.
Microvascular Dynamics and the Glymphatic Link
One of the most exciting frontiers is the direct investigation of how changes in blood flow during sleep facilitate brain cleansing. Advanced imaging techniques are being used to study the cerebral vasculature in real-time during sleep.
Personalized Chronotherapy and Disease Treatment
The field of chronotherapy—timing medical treatments to coincide with the body's biological rhythms—is gaining traction. Since body temperature is a robust marker of circadian phase, it could be used to personalize treatment timing for maximum efficacy and minimum side effects.
The Gut-Brain-Thermal Axis
Emerging research points to a powerful connection between the gut microbiome, sleep, and thermoregulation. Certain gut bacteria produce metabolites that influence the production of sleep-regulating neurotransmitters like serotonin and melatonin. They may also influence systemic inflammation, which can affect the hypothalamic thermostat. Future probiotics or dietary regimens may be designed specifically to support a healthy circadian thermal rhythm and improve sleep quality.
Ethical Considerations and the Data Dilemma
As wearables generate ever more intimate physiological data, including our vulnerable nocturnal patterns, important questions arise:
The Integration of AI and Predictive Environments
The ultimate frontier is a fully adaptive sleep ecosystem. Imagine an AI that learns your unique physiology over years, integrates real-time data from your ring, your bed, and your room, and then not only adjusts the environment but also predicts and preempts disruptions.
This is not science fiction; it is the logical endpoint of the data revolution currently underway. To stay abreast of these rapidly evolving developments and their practical applications, following resources like the Oxyzen.ai blog can provide a continuous stream of insights. As we stand at this precipice of discovery, it’s valuable to reflect on how far we’ve come in our understanding, and what timeless wisdom we can reclaim.
The quest to understand sleep and its connection to our physical state is as old as humanity itself. While we now have polysomnography labs and infrared sensors, our ancestors observed the same phenomena and devised their own ingenious, if sometimes imperfect, explanations and interventions. Examining this history reveals a thread of intuitive understanding about the thermal nature of sleep, now being validated by modern science.
Pre-Modern Observations and Practices
Across cultures, a connection between coolness and rest was instinctively recognized.
The Dawn of Scientific Inquiry
The formal scientific study of sleep and body temperature began in earnest in the 19th and early 20th centuries.
The Modern Synthesis and the Wearable Era
The latter part of the 20th century saw the pieces come together: the mapping of sleep architecture, the formal description of the circadian system, and the understanding of the two-process model of sleep regulation. Body temperature was recognized not as a bystander but as a central player in this model. The last decade, however, has been defined by democratization. The miniaturization of sensors and the proliferation of smartphones have moved sleep and temperature monitoring out of the sleep lab and into the home. For the first time in history, millions of people can observe their own physiological rhythms, creating a massive dataset and a public that is more literate in sleep science than ever before.
This journey from intuition to data underscores a profound truth: our bodies have always been communicating the importance of thermal balance for sleep. We felt it in our desire for a cool pillow. We built for it. We medicined for it. Now, we can measure it. This blend of ancient wisdom and modern validation is a powerful narrative, one that resonates with our holistic approach to wellness technology, an approach rooted in our core vision and values at Oxyzen, which you can explore here. With this comprehensive understanding—spanning biology, technology, application, and history—we are now equipped to synthesize it all into a cohesive, actionable framework for life.
Understanding the complex relationship between sleep stages and body temperature is fascinating, but its true value is realized only when translated into tangible change. This final synthesis distills the key principles from every preceding section into a clear, tiered action plan. Think of it as your personal blueprint for harnessing your internal thermostat to engineer better sleep, starting with foundational pillars and progressing to advanced fine-tuning.
Tier 1: The Non-Negotiable Foundation
These actions address the most powerful environmental and behavioral disruptors. Master this tier before moving on.
Tier 2: Data-Informed Personalization
This tier involves using feedback, either subjective or from technology, to refine the foundation.
Tier 3: Advanced Lifestyle Integration
These are nuanced habits that synchronize your entire day with your nocturnal thermal goals.
Tier 4: Troubleshooting and Long-Term Optimization
When problems persist, use a diagnostic approach.
Remember, consistency is more important than perfection. Progress, not perfection, is the goal. This journey is about building a collaborative relationship with your body's innate wisdom. For ongoing support, community experiences, and deeper dives into each of these strategies, our library of resources at Oxyzen.ai is continually updated. By internalizing and acting on this knowledge, you cease to be a passive passenger in your sleep. You become the architect, using the timeless, reliable blueprint of your own body temperature to build a foundation of truly restorative rest, night after night.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/