Workplace Stress and Physical Health: Preventing Stress-Related Illness
Create structure and physical/ temporal boundaries at home to separate work and personal life, reducing seepage of stress.
Create structure and physical/ temporal boundaries at home to separate work and personal life, reducing seepage of stress.
You know the feeling. The tightness in your shoulders at 3 PM. The dull headache that arrives right before a major deadline. The restless night of sleep after a tense meeting, followed by the bleary-eyed morning fueled by caffeine and sheer will. We’ve all brushed these sensations aside as just “part of the job,” the unavoidable tax on a modern professional life. But what if these weren’t just fleeting annoyances? What if they were the earliest warning signals—the distant tremors of a seismic health crisis building within your body?
Workplace stress has quietly escalated from a manageable occupational hazard to a full-blown public health emergency. The World Health Organization now officially classifies burnout as an occupational phenomenon, driven by chronic workplace stress. Yet, we continue to misunderstand its true impact, compartmentalizing it as a “mental” or “emotional” issue. This is our critical error. Stress is not a spectator in the theater of your health; it is the director, the playwright, and the stage manager all at once, orchestrating a cascade of physiological events that directly manifest as physical disease.
The link between a demanding boss, an overflowing inbox, and a future diagnosis of hypertension, gastrointestinal disorder, or autoimmune condition is not hypothetical—it is biochemical, direct, and alarmingly common. The human body’s brilliant, ancient stress response, designed to sprint from predators, is being triggered by quarterly reports, Slack notifications, and passive-aggressive emails, and it’s being held in the “on” position for 40, 50, 60 hours a week. The result is a slow, systemic corrosion.
This article is not another list of superficial “stress-busting” tips. It is a deep, evidence-based exploration into the hidden pathways that convert psychological pressure into physical pathology. We will dissect the science, trace the invisible connections, and, most importantly, focus on actionable, prevention-first strategies. In an era of quantified self-care, technology like advanced wellness wearables, such as the smart rings from innovators like Oxyzen, provides us with an unprecedented window into these internal processes, transforming subjective feelings of "being stressed" into objective, actionable data. By understanding the mechanisms and monitoring our physiological baseline, we can move from being passive victims of stress to empowered architects of our own resilience, preventing illness before it ever takes root.

To combat an enemy, you must first know its name and its nature. "Stress" is an overused, umbrella term that often obscures a critical distinction: the difference between acute stress and chronic stress. Understanding this dichotomy is the foundational step in preventing its physical fallout.
Acute stress is your body's brilliant, time-tested survival mechanism. It's the jolt you feel when a car swerves into your lane, the surge before a major presentation, or the intense focus during a critical negotiation. This is the "fight-or-flight" response, masterminded by the sympathetic nervous system. Hormones like adrenaline and cortisol flood your system. Your heart rate and blood pressure spike, shunting blood to your muscles and brain. Your pupils dilate. Digestion halts. You become, momentarily, faster, stronger, and sharper. This response is self-limiting; once the threat passes, your parasympathetic nervous system engages the "rest-and-digest" mode, returning your body to homeostasis. Acute stress is not just normal; it's essential and even performance-enhancing.
Chronic workplace stress, however, is a pathological perversion of this system. It occurs when the demands of the work environment consistently and perpetually exceed an individual’s ability to cope, with insufficient opportunity for recovery. The "threat" is no longer a saber-toothed tiger but a ceaseless barrage of digital pings, unrealistic deadlines, ambiguous roles, and a pervasive culture of "always-on" availability. The problem is that your hypothalamus, the ancient alarm bell in your brain, cannot distinguish between a predator and a pressing email from your manager sent at 10 PM.
When this alarm rings incessantly, the stress response becomes maladaptive. Instead of a sharp, healthy spike, cortisol levels plateau at a persistently high baseline. The body remains in a low-grade state of emergency, a simmering physiological rebellion. This is the silent killer. You may not feel the intense panic of acute stress, but your cardiovascular, immune, endocrine, and nervous systems are under constant siege.
The sources of this chronic stress are multifaceted and often systemic:
Recognizing chronic stress is the first battle. It often masquerades as normalcy. The key is to shift from subjective feeling ("I'm just busy") to objective observation. This is where modern biofeedback technology becomes revolutionary. A device like a smart ring from Oxyzen can track physiological markers like Heart Rate Variability (HRV)—a key indicator of your nervous system's resilience and stress load—24/7. By monitoring trends in your HRV, sleep quality, and resting heart rate, you gain an unbiased report card of your body's true stress state, long before it escalates into debilitating symptoms. It makes the invisible, visible.
How does a feeling—anxiety about a performance review, frustration with a colleague—translate into a physical ulcer, a spike in blood pressure, or a compromised immune system? The process is not mystical; it is a well-mapped series of biological events. Chronic stress acts as a systemic toxin, and its delivery mechanisms are our own hormones and neural pathways.
The command center for this process is the Hypothalamic-Pituitary-Adrenal (HPA) Axis, a complex feedback loop between your brain and your adrenal glands. Under perceived threat, the hypothalamus secretes corticotropin-releasing hormone (CRH), which signals the pituitary gland to release adrenocorticotropic hormone (ACTH). This, in turn, commands the adrenal glands (sitting atop your kidneys) to produce and release the primary stress hormone: cortisol.
In short bursts, cortisol is incredibly useful. It mobilizes glucose for immediate energy, modulates inflammation, and helps control metabolism. However, under the constant drip-feed of chronic stress, elevated cortisol wreaks havoc:
Beyond the HPA axis, chronic stress keeps the sympathetic nervous system in a state of overdrive. This leads to elevated levels of adrenaline and norepinephrine, which further strain the heart, increase muscular tension (leading to chronic pain, especially in the back, neck, and shoulders), and contribute to anxiety and sleep disturbances.
The takeaway is unambiguous: chronic stress is not "in your head." It is in your arteries, your gut lining, your pancreatic cells, and your white blood cells. It is a whole-body experience. The persistent ache in your neck or the cold you can’t seem to shake may not be random misfortunes; they may be the physical invoices your body is presenting for psychological debts incurred at work. For a deeper dive into how specific bodily systems are affected, our resource hub at the Oxyzen blog offers continuous updates on the latest research in psychoneuroimmunology—the study of how our thoughts and feelings directly shape our physical health.
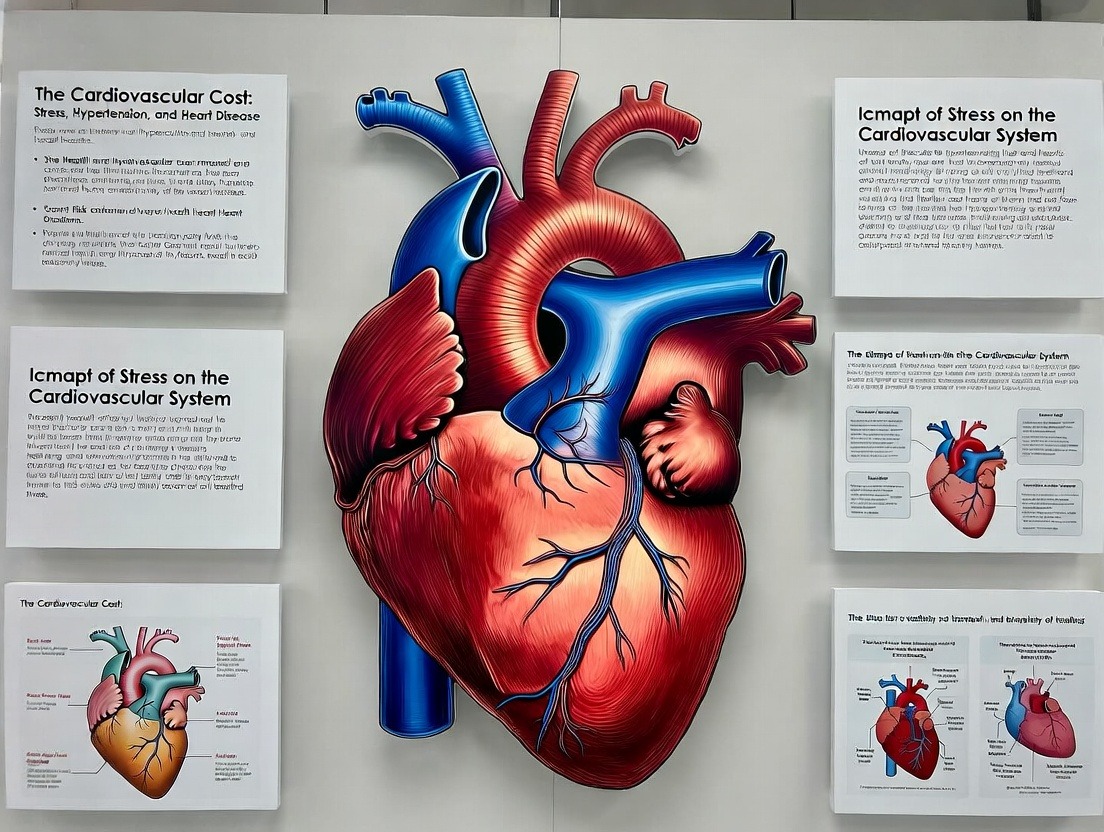
If one system bears the most direct and devastating brunt of chronic workplace stress, it is the cardiovascular system. The connection between a high-pressure job and a struggling heart is not anecdotal; it is one of the most robustly documented relationships in occupational medicine.
The mechanism is a perfect storm of physiological insults. As outlined, stress hormones like cortisol and adrenaline directly increase heart rate and cause vasoconstriction—the tightening of blood vessels. Think of it as running your car engine at high RPMs while simultaneously stepping on the brake. Over time, this forces your heart to work harder against greater resistance, leading to hypertension. Hypertension is aptly called the "silent killer" because it often has no symptoms while it inflicts damage, scarring artery walls and forcing the heart muscle to thicken and weaken.
But the damage extends far beyond blood pressure. Chronic stress contributes to:
Landmark studies, such as the Whitehall II studies of British civil servants, have consistently shown that employees with lower job control and higher job demands face a significantly elevated risk of coronary heart disease. The risk profile isn't limited to traditionally "high-stakes" jobs like CEOs or surgeons. It is profoundly influenced by the psychosocial environment: a lack of autonomy, unfair treatment, and effort-reward imbalance.
The Modern Metric: Heart Rate Variability (HRV)
This is where understanding shifts from the theoretical to the personal. Heart Rate Variability (HRV) has emerged as a critical, non-invasive window into cardiovascular and autonomic nervous system health. HRV measures the subtle variations in time between each heartbeat. A high HRV indicates a healthy, resilient heart and a nervous system that can flexibly switch between stress (sympathetic) and recovery (parasympathetic) modes. A low, rigid HRV is a strong indicator of chronic stress, autonomic imbalance, and an elevated risk for cardiovascular events.
Monitoring your HRV is no longer confined to clinical settings. Advanced wellness wearables, like the smart ring developed by Oxyzen, provide continuous, clinically-validated HRV tracking during both day and night (where the most reliable readings are often taken). By observing your HRV trends, you can see in real time how a stressful week at the office depresses your resilience score. More importantly, you can objectively measure the impact of stress-management interventions—like meditation, a walk in nature, or improved sleep—as your HRV recovers. It transforms heart health from an abstract future concern into a daily, manageable metric. Real users have documented this journey; you can read their transformative experiences in the Oxyzen testimonials section, where many highlight how data-driven insights led to proactive changes that improved their cardiovascular markers.
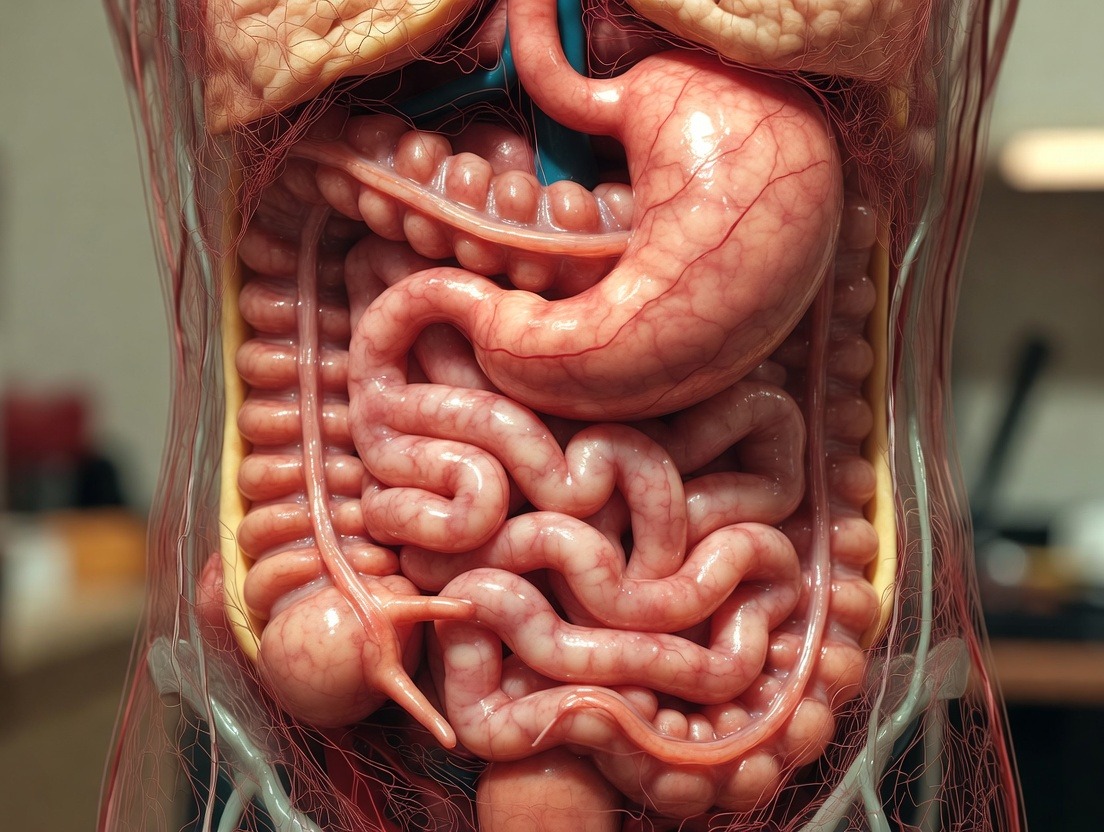
We intuitively understand the link between stress and our stomach. We get "butterflies" before a big event or feel nauseous after bad news. This gut-level intuition is rooted in a sophisticated biological communication network: the gut-brain axis. This bidirectional highway, comprised of neural, hormonal, and immune pathways, means your brain and gastrointestinal tract are in constant, intimate conversation. When chronic stress hijacks the brain's end of the line, the gut suffers profoundly.
The primary pathway is, once again, the HPA axis and the flood of cortisol. Under threat, the body prioritizes survival over digestion. Blood flow is shunted away from the gut to the muscles and brain. This can lead to:
Furthermore, a significant portion of the body's serotonin—a neurotransmitter crucial for mood regulation—is actually produced in the gut. An unhappy, inflamed gut can impair serotonin production, potentially feeding back into feelings of anxiety and depression, creating a vicious cycle where stress damages the gut, and the damaged gut exacerbates stress.
Breaking the Cycle with Awareness
Managing stress for gut health goes beyond avoiding spicy food. It requires systemic nervous system regulation. Techniques that engage the vagus nerve—the main component of the parasympathetic "rest-and-digest" system—are particularly potent. These include deep, diaphragmatic breathing, humming, singing, and meditation.
Here, technology can serve as a powerful biofeedback tool. By using a device that tracks physiological markers of stress and recovery, you can begin to correlate subjective feelings of digestive discomfort with objective data. For instance, you might notice that a day with particularly low HRV and restless sleep (as tracked by a comprehensive wellness wearable) is followed by a morning of bloating and discomfort. This data empowers you to make proactive choices—perhaps committing to a breathing exercise before a known stressful event or prioritizing sleep during a demanding project week—to protect your gut. Exploring the connection between biometric data and digestive wellness is a topic we frequently cover in our detailed guides on the Oxyzen blog.

The belief that you "get sick after a big project finishes" is more than folklore; it's a documented immunological phenomenon, often called the "let-down effect." Chronic stress acts as a potent immunosuppressant, dismantling your body's defenses in multiple, synergistic ways.
The relationship between stress and immunity is complex and paradoxical. In the very short term (minutes to hours), acute stress can actually boost certain parts of the immune system, an evolutionary adaptation to prepare for potential injury and infection during a physical confrontation. However, when stress becomes chronic, the sustained elevation of cortisol and other mediators has a profoundly suppressive effect:
The consequences are measurable and significant. Studies show that individuals reporting high psychological stress are more susceptible to the common cold, experience more severe viral infections (like influenza or herpes outbreaks), and have slower wound healing times. For individuals with autoimmune conditions—such as rheumatoid arthritis, lupus, or multiple sclerosis—periods of high stress are consistently linked to disease flares.
The Critical Role of Sleep
This immune suppression is catastrophically compounded by the sleep disruption that almost universally accompanies chronic stress. Sleep is when the immune system does its most vital repair and regeneration work. Cytokines, which are crucial for fighting infection, are released during deep sleep. Chronic stress leads to hyperarousal and fragmented sleep, robbing the immune system of its prime recovery time. It’s a double assault: stress chemically handicaps your immune cells, and then the resulting poor sleep denies them the opportunity to regroup.
Monitoring your physiological data provides crucial insight into this vulnerability. A wellness tracker that measures parameters like resting heart rate, HRV, and sleep architecture (time spent in light, deep, and REM sleep) can show you when your body is in a depleted state. A persistently elevated resting heart rate and poor deep sleep scores are strong indicators that your recovery systems are overwhelmed and your immune resilience is likely compromised. This data serves as an early warning to prioritize restorative practices—like enforcing strict sleep hygiene, taking a rest day, or saying no to extra commitments—before your body forces the issue with an illness. For those curious about how specific sleep metrics correlate with immune function, our FAQ section delves into the science behind the data points these advanced devices provide.
The link between chronic stress and changes in body composition is often misunderstood as a simple failure of willpower. In reality, it is a hormonally-driven process that actively subverts your best dietary and exercise intentions. Stress doesn't just make you reach for comfort food; it reprograms your metabolism to store fat, particularly the most dangerous kind.
The master manipulator here, again, is cortisol. Its evolutionary purpose is to ensure you have enough energy to fight or flee. Under chronic stress, it executes this mandate with devastating efficiency:
This creates a metabolic trap. The more stressed you are, the more your body is hormonally primed to gain weight, particularly around the midsection. The weight gain itself, and the associated health risks, then become a new source of stress and poor body image, perpetuating the cycle.
Data-Driven Metabolic Awareness
Breaking free requires more than just calorie counting; it requires stress management. By tracking physiological markers, you can start to identify your personal stress triggers and their metabolic ripple effects. For example, you might see a pattern where periods of low HRV and poor sleep (indicating high stress and poor recovery) correlate with intense sugar cravings or a plateau in your fitness progress.
Wearable technology provides an objective lens on this process. A smart ring that tracks activity, sleep, and stress-recovery metrics like HRV offers a holistic picture. You can see how a stressful workweek not only affects your nervous system but also correlates with changes in your body's readiness and energy expenditure. This integrated view empowers you to intervene strategically—perhaps by incorporating stress-reducing yoga on high-pressure days or understanding that a poor recovery score means it’s a day for gentle movement, not an intense, cortisol-spiking workout. To understand how the founders of such technology envisioned this holistic approach to health, you can explore Oxyzen's story and the vision behind creating a device that connects these disparate dots.
The physical manifestation of stress that most people recognize immediately is muscle tension. That stiff neck, those tight shoulders, the clenched jaw—these are the body's literal armoring against a perceived threat. When this tension becomes the default state, it evolves from transient discomfort into chronic pain and legitimate musculoskeletal disorders.
The pathway is both neurological and biochemical. Under stress, the brain sends continuous signals via the sympathetic nervous system to prepare the muscles for action. This leads to sustained contraction. Over time, this constant tension:
Furthermore, the inflammatory chemicals released systemically under chronic stress (like cytokines) can sensitize the entire nervous system, a condition known as central sensitization. This means the pain-processing centers in the brain and spinal cord become hyper-reactive, interpreting normal signals as painful and amplifying pain signals from the periphery. In this state, even light touch or normal movement can be perceived as painful, and conditions like fibromyalgia can be triggered or worsened.
The Mind-Body Feedback Loop of Pain
Chronic pain is exhausting and limiting, which in itself becomes a massive source of psychological stress, anxiety, and often depression. This creates a brutal feedback loop: Stress → Muscle Tension & Inflammation → Pain → More Stress & Anxiety → Worse Pain. Breaking this cycle requires addressing both the physical tension and the underlying nervous system dysregulation.
Interventions like mindfulness-based stress reduction (MBSR), progressive muscle relaxation, and gentle movement (like yoga or tai chi) are powerfully effective because they work on both fronts. They physically release contracted muscles while simultaneously engaging the parasympathetic nervous system to lower the overall stress volume.
Here, biometric feedback is invaluable. A device that monitors your stress levels through HRV can help you identify the times of day or specific tasks that trigger your highest tension states. You may learn, for instance, that your stress metrics skyrocket during long periods of sitting at your computer. This data can prompt you to set reminders for micro-breaks, stretching, or deep breathing exercises before the tension locks in. It shifts pain management from a reactive (treating pain after it starts) to a proactive (preventing the physiological state that causes it) model. For practical strategies on using data to manage tension and pain, our resource library at the Oxyzen blog offers evidence-based techniques and user case studies.
"Brain fog"—that feeling of mental murkiness, forgetfulness, and an inability to concentrate—is one of the most common and debilitating complaints of chronically stressed professionals. Far from being a minor inconvenience, it is a visible symptom of stress-induced changes in brain structure and function.
The brain is both the source of the stress response and one of its primary targets. Elevated cortisol over extended periods has several neurotoxic effects:
The cognitive result is the familiar experience of workplace brain fog: walking into a room and forgetting why, struggling to follow a complex thread in a meeting, rereading the same paragraph repeatedly, and feeling mentally exhausted after tasks that used to be simple.
Protecting Your Cognitive Capital
Safeguarding your brain from stress is non-negotiable for long-term professional performance and personal well-being. The cornerstone of this protection is sleep and recovery. During deep sleep, the brain's glymphatic system activates, flushing out metabolic waste products that accumulate during the day, including beta-amyloid plaques associated with Alzheimer's disease.
Monitoring your sleep and recovery metrics provides direct insight into your brain's maintenance schedule. A wearable that tracks sleep stages can show you if you're getting sufficient deep (slow-wave) sleep and REM sleep, both vital for memory consolidation and cognitive repair. A consistently low HRV score is a proxy for a nervous system under siege, indicating that your brain is operating in a suboptimal state. By using this data to prioritize and improve sleep quality, manage stress through proven techniques, and take true mental breaks, you are not just feeling sharper tomorrow—you are actively investing in the long-term health of your most vital organ. Understanding the full scope of how our technology is designed to support this cognitive protection is part of the mission detailed on Oxyzen's about page.
The endocrine system is a delicate, interconnected orchestra of glands and hormones that regulate everything from your metabolism and sleep-wake cycle to your reproductive health and mood. Chronic stress, acting as the HPA axis conductor gone rogue, doesn't just elevate cortisol; it throws the entire hormonal symphony into disarray.
The principle is called pregnenolone steal. Pregnenolone is a master hormone precursor, the starting material for manufacturing cortisol, estrogen, progesterone, testosterone, and DHEA. Under chronic stress, the body prioritizes survival, shunting the vast majority of pregnenolone down the pathway to produce more and more cortisol. This "steals" the raw material away from the synthesis of other essential sex hormones.
The downstream effects are system-wide:
This hormonal chaos manifests in a vague but debilitating cluster of symptoms: relentless fatigue unrelieved by sleep, unexplained weight changes, loss of motivation and drive, and a diminished sense of well-being. It's often misattributed to "aging" or "burnout" without recognizing the underlying endocrine disruption.
Restoring Balance Through Rhythm
Correcting stress-induced hormonal imbalance begins with restoring rhythm and signals of safety to the nervous system. Consistent sleep, balanced nutrition (avoiding blood sugar spikes that further stress the system), regular moderate exercise (not chronic intense overtraining), and mindfulness are foundational.
Biometric data provides a crucial feedback loop for this restoration. Tracking your body temperature can reveal subtle shifts related to your menstrual cycle or thyroid function. Monitoring your sleep continuity and HRV shows whether your body is entering the deep, restorative states necessary for hormonal repair and production. Seeing positive trends in these metrics as you implement stress-reduction strategies offers powerful affirmation that you are not just feeling better—you are physiologically rebalancing. For individuals navigating the complex intersection of stress and hormonal health, the community experiences shared in places like Oxyzen testimonials can provide relatable insights and motivation.
The most profound and alarming link between chronic stress and physical health lies in its ability to dysregulate the immune system to the point of provoking or exacerbating autoimmune disease. Autoimmune conditions—such as rheumatoid arthritis, lupus, Hashimoto's thyroiditis, psoriasis, and multiple sclerosis—occur when the immune system loses its ability to distinguish "self" from "non-self" and launches an attack on the body's own tissues.
Chronic stress is a key environmental trigger in this "friendly fire" scenario, primarily through its dual impact on inflammation and immune function:
The evidence is compelling. Numerous studies have found that a high proportion of patients with autoimmune diseases report experiencing unusual emotional stress before disease onset. Furthermore, periods of significant stress are frequently linked to disease flares in those already diagnosed.
This underscores a critical paradigm shift: managing chronic stress is not merely about improving quality of life or productivity; for many, it is a fundamental, non-negotiable component of managing a serious, lifelong physical disease. Stress reduction becomes as essential as medication.
Biomarkers as a Guide
For those with or at risk for inflammatory conditions, monitoring internal biomarkers becomes even more critical. While a wellness wearable cannot diagnose an autoimmune disease, it can track the physiological terrain that fuels it. Persistent deviations in metrics like resting heart rate, HRV, and sleep quality can serve as early warning signs of rising systemic stress and inflammation, potentially preceding a symptom flare. This data empowers individuals to proactively double down on their anti-inflammatory and stress-resilience practices—be it through diet, meditation, or rest—in partnership with their healthcare provider. It represents the pinnacle of preventive, personalized health management. The vision for creating tools that empower this level of personal insight is rooted in a commitment to holistic wellness, a principle you can learn more about in Oxyzen's story.
In the war against stress-related illness, ignorance is not bliss—it is vulnerability. The traditional model of healthcare is reactive: you feel symptoms, you see a doctor, you receive a diagnosis, and you begin treatment. For stress-induced conditions, which develop silently over years, this model often means the battle begins after significant damage has already occurred. The new paradigm is preventive, proactive, and data-informed.
This is the revolutionary promise of personal biometric monitoring. By consistently tracking key physiological signals, you move from guessing about your internal state to knowing it. You gain an objective, personalized baseline, allowing you to see deviations caused by stress long before they crystallize into disease.
The Core Metrics of Resilience:
Modern wearable technology, particularly in the form of smart rings like those developed by Oxyzen, has made this continuous, comfortable monitoring a seamless part of daily life. Worn on the finger, they capture precise physiological data from the rich vasculature at the fingertip, 24/7, without the obtrusiveness of a wrist device during sleep or typing.
From Data to Wisdom to Action
The true power lies not in the data collection itself, but in the interpretation and application. A comprehensive wellness platform translates raw numbers into actionable insights:
This approach demystifies wellness. It replaces generic advice with personalized intelligence, empowering you to become the expert on your own body's response to the pressures of modern work. It transforms stress management from a vague concept into a tangible, daily practice of self-preservation. To explore the full capabilities of how such a system works and how it can be integrated into a proactive health strategy, visit the Oxyzen homepage for a detailed overview.
Understanding the pathways of stress-induced damage is only half the battle. The other, more empowering half, is building resilience: the capacity to prepare for, recover from, and adapt in the face of stress, trauma, and adversity. Resilience is not a magical trait you're born with; it is a physiological state you can cultivate. It is the difference between a twig that snaps under pressure and a bamboo stalk that bends and rebounds.
At its core, biological resilience is governed by the autonomic nervous system (ANS). A resilient nervous system is like a skilled driver: it can accelerate smoothly into action (sympathetic "fight-or-flight") when needed and then brake effectively to return to a calm, restorative state (parasympathetic "rest-and-digest"). Chronic stress essentially jams the accelerator to the floor while cutting the brake lines. Building resilience is about repairing those brakes and regaining masterful control of the vehicle.
The key metric here, once again, is Heart Rate Variability (HRV). Think of HRV as the indicator of your nervous system's flexibility and bandwidth. High HRV signifies a robust, agile system that can respond powerfully to challenge and then recover quickly. Low HRV indicates a rigid, exhausted system stuck in survival mode. The goal of any resilience-building practice is to improve your HRV over time.
The Pillars of Physiological Resilience:
Building resilience is an active, daily process of sending "signals of safety" to your body, convincing your ancient brain that you are not, in fact, in mortal danger because of an overflowing inbox. This process moves us from a state of passive endurance to one of active fortification. For a deep exploration of specific, science-backed resilience techniques, our curated library of resources on the Oxyzen blog is continually updated with the latest findings.
Knowledge of resilience is useless without application. The modern workplace serves up micro-doses of stress continuously. To prevent them from accumulating into a toxic dose, you need a toolkit of practical, immediate techniques that can intercept the stress response in real time. These are not weekend retreat solutions; they are tactical interventions for the middle of a chaotic Tuesday.
The objective is to activate the parasympathetic nervous system, shifting the body from "fight-or-flight" to "rest-and-digest." Here are the most effective, evidence-based methods:
1. Diaphragmatic (Belly) Breathing:
This is the most potent and accessible tool you have. Shallow, chest-based breathing is linked to anxiety. Deep, diaphragmatic breathing stimulates the vagus nerve.
2. The Physiological Sigh:
Discovered by Stanford researchers, this is a fast-acting pattern that is our body's natural reset button for stress.
3. Box Breathing (Tactical Breathing):
Used by Navy SEALs to stay calm under extreme pressure, this technique adds structured mental focus to breath control.
4. Sensory Grounding (The 5-4-3-2-1 Technique):
This cognitive technique pulls you out of anxious thoughts and into the present moment by engaging your senses.
5. Brief Progressive Muscle Relaxation (PMR):
You can target key stress-holding areas in under a minute.
Measuring Your Progress
The power of these techniques multiplies when you can see their direct physiological impact. This is where biometric feedback creates a powerful reinforcement loop. Using a smart ring like Oxyzen, you can perform a one-minute breathing exercise and literally watch as your live HRV reading improves and your heart rate drops on the accompanying app. This transforms an abstract relaxation exercise into a tangible, rewarding skill. You learn which techniques work best for your unique physiology, turning stress management into a personalized science. Many users first discover the power of this feedback loop through the Oxyzen FAQ, which details how to interpret real-time data during mindfulness practices.
If you must prioritize one thing in your battle against workplace stress, it must be sleep. Sleep is not a luxury; it is the most critical period of physiological and psychological restoration. It is when your body repairs cellular damage, consolidates memories, clears metabolic waste from the brain, and rebalances hormones like cortisol and growth hormone. Skimping on sleep is like taking out a high-interest loan on your health—the debt compounds quickly with devastating effects.
Chronic stress and poor sleep are locked in a vicious cycle. Stress causes hyperarousal, making it difficult to fall and stay asleep. Poor sleep, in turn, lowers your emotional threshold, making you more reactive to stress the next day, further impairing cognitive function and decision-making. Breaking this cycle is paramount.
The Architecture of Restorative Sleep:
Actionable Strategies for Sleep Hygiene:
Seeing this data provides the motivation to defend your sleep boundaries rigorously. When you can correlate a night of high sleep consistency and balanced stages with a high "Readiness" score and stable energy the next day, sleep shifts from a passive activity to an active, non-negotiable performance strategy. The team at Oxyzen built their technology with this principle at its core, recognizing that quality sleep is the foundational metric for all other health outcomes.
The phrase "stress eating" exists for a reason, but we have the power to flip the script. Instead of eating because of stress, we can learn to eat for stress resilience. Food is not just fuel; it is information that directly influences your hormonal balance, gut health, and inflammatory state. The right nutritional choices can fortify your body against the biochemical onslaught of cortisol, while poor choices can amplify it.
The Stress-Busting Diet Framework:
1. Stabilize Blood Sugar: Cortisol is a key player in blood sugar regulation. When you eat refined carbs and sugars, you cause a rapid spike and subsequent crash in blood glucose. This crash is itself a stressor, prompting the release of more cortisol to mobilize more glucose, creating a rollercoaster of energy, mood swings, and cravings.
2. Support the HPA Axis & Adrenals: Certain nutrients are directly involved in the production and regulation of stress hormones.
3. Heal the Gut: A healthy gut microbiome is essential for regulating the stress response via the gut-brain axis.
4. Combat Inflammation: Choose foods that lower, not raise, systemic inflammation.
The Role of Mindful Eating:
Stress often leads to distracted, rapid eating, which impairs digestion and satiety signals. Practice mindful eating: put away screens, chew slowly, and pay attention to hunger and fullness cues. This simple act is a form of parasympathetic nervous system activation.
Using Biometrics to Personalize Nutrition:
How do you know if your dietary changes are working? Biometric feedback provides answers. You might track how your afternoon HRV and energy levels differ after a lunch of grilled chicken and vegetables versus a sandwich and chips. You could monitor how your resting heart rate and sleep quality respond to cutting out late-night sugar. Anecdotal evidence from users, like those sharing their journeys in the Oxyzen testimonials, often highlights how data revealed personalized food sensitivities and optimal eating windows, allowing them to tailor their nutrition for maximal energy and calm.
Exercise presents a fascinating paradox in stress physiology. It is a controlled, self-induced stressor that, when applied correctly, makes the body more resilient to uncontrollable, psychological stress. The key lies in the principle of hormesis—a beneficial adaptive response to a mild stressor. Think of it as training your stress-response system.
How the Right Exercise Builds Resilience:
The Critical Caveat: Avoiding Overtraining
The relationship between exercise and stress follows an inverted U-curve. Too little leaves you deconditioned and vulnerable. Too much—overtraining—becomes a massive physical stressor that compounds life stress, leading to exhaustion, hormonal disruption (elevated cortisol, lowered testosterone), suppressed immunity, and a plummeting HRV. This is common in driven professionals who use intense exercise as their only outlet for work stress, inadvertently pushing their allostatic load into the danger zone.
Designing a Stress-Resilient Movement Plan:
By framing exercise as a tool for nervous system regulation rather than just calorie burning or muscle building, you can harness its true power as a cornerstone of stress prevention. For more on crafting a personalized, data-informed movement strategy that adapts to your stress load, explore the guides and discussions available on the Oxyzen blog.
Your physiological stress response is not triggered by events themselves, but by your perception of those events. Two people can face the same tight deadline: one perceives it as an insurmountable threat to their job security (triggering high cortisol), while another perceives it as a challenging but manageable task (triggering focused arousal). This difference is rooted in cognitive patterns—the habitual ways your brain interprets the world.
Cognitive reframing, a core component of Cognitive Behavioral Therapy (CBT), is the practice of identifying and changing these stress-inducing thought patterns. It is literal brain rewiring (neuroplasticity) for resilience.
Common Cognitive Distortions in the Workplace:
The Reframing Process in Action:
Building a Resilient Mindset:
Validating the Mind-Body Link
The effectiveness of cognitive reframing can be seen not just in felt calm, but in physiology. When you successfully reframe a stressful situation, you are down-regulating the amygdala and engaging the prefrontal cortex. This should manifest in real-time biometrics: a lower spike in heart rate during the stressful event, and a faster return to baseline HRV afterward. Using a device to observe this connection—seeing how a deliberate shift in perspective actually changes your body's response—powerfully reinforces the practice. It proves that your thoughts are not just ephemeral; they are biological commands. Understanding this deep connection between mind and body is central to the holistic vision behind tools like Oxyzen, as detailed in their our story page.
Your physical workspace is not a neutral container; it is an active participant in your stress physiology. Poor lighting, awkward posture, noise pollution, and clutter all act as low-grade, chronic stressors that drain your cognitive resources and keep your nervous system subtly on edge. Optimizing your environment is a direct form of stress prevention.
1. The Power of Light:
Light is the primary regulator of your circadian rhythm. Poor light exposure disrupts sleep and energy.
2. Ergonomics to Reduce Physical Stress:
Musculoskeletal tension from poor posture is a constant source of physical stress that feeds back into mental strain.
3. Soundscaping for Focus:
Unpredictable, uncontrollable noise (chatty colleagues, construction) is a major cognitive stressor, triggering a "What was that?" orienting response that fragments attention.
4. The Psychology of Clutter:
Visual clutter competes for your brain's attentional resources, increasing cognitive load and feelings of being overwhelmed.
5. Biophilic Design Elements:
Humans have an innate connection to nature (biophilia). Incorporating elements of nature reduces stress and improves cognition.
Using Biometrics to Test Your Environment:
Your body's data is the ultimate judge of your workspace efficacy. Experiment and observe:
By treating your workspace as a laboratory for well-being, you can engineer an environment that actively supports, rather than undermines, your physiological resilience. For more ideas on creating a holistic, health-supportive work life, from environment to routine, the resources at Oxyzen's blog offer continuous inspiration.
The very tools designed to make us more productive have become primary vectors of chronic workplace stress. The constant stream of notifications, the pressure to be perpetually available, and the endless context-switching fragment our attention and keep our nervous systems in a state of high alert. Managing your digital environment is not a tech hack; it is a critical stress-survival skill.
The Physiology of Notification Stress:
Each ping, buzz, or badge triggers a micro-dose of the "orienting response." Your brain wonders, "Is this important? Is this a threat or reward?" This causes a mini-release of cortisol and dopamine. Over dozens or hundreds of times a day, this creates a state of chronic, low-grade anxiety and cognitive fatigue, eroding your ability to focus deeply.
Strategic Digital Hygiene Practices:
1. Tame the Notification Beast:
2. Reclaim Deep Work:
3. Establish Digital Boundaries:
4. Mindful Consumption:
Quantifying Digital Detox:
The benefits of digital boundaries are not hypothetical; they are measurable. After implementing a strict "no screens 1 hour before bed" rule, check your sleep tracker. You will likely see an increase in deep sleep and a faster sleep onset. After a weekend of true digital disconnection, observe your Monday morning resting heart rate and HRV—they will often show significantly better recovery than after a weekend spent intermittently checking work email.
Technology, when used intentionally, can also be part of the solution. Using a smart ring to monitor your stress levels can actually alert you to the need for a digital break. If you see your HRV dipping and your heart rate rising during a long stretch of screen time, that's your body's data-driven cue to step away, stretch, and breathe. It’s about using technology to understand your limits, not to breach them constantly. For support in setting up these healthy digital habits, our FAQ section addresses common questions about integrating wellness tech into a balanced life.
Humans are neurologically wired for connection. Social support is not a soft "nice-to-have"; it is a biological imperative that dramatically buffers the impact of stress. Loneliness and social isolation, on the other hand, are themselves potent stressors, activating the same threat pathways in the brain as physical pain.
The Science of Social Buffering:
Positive social interaction and perceived support trigger the release of oxytocin (the "bonding hormone"), which has an anxiety-reducing effect and can dampen cortisol production. Knowing you have people you can rely on creates a psychological sense of safety, which directly signals to the amygdala that the environment is less threatening.
Cultivating Connection in a Hybrid/Remote World:
Modern work often undermines natural social connection. We must be intentional about building and maintaining our support networks.
1. Foster High-Quality Work Relationships:
2. Nurture Your Personal Network:
3. Seek Professional Support When Needed:
4. Be a Source of Support for Others:
The Data of Connection:
Remarkably, the strength of your social bonds can be reflected in your biometrics. Studies have linked strong social support to healthier HRV profiles and lower resting heart rates. Conversely, periods of loneliness or conflict can coincide with measurable dips in recovery metrics.
You can even use this data to guide your social choices. If you notice that your stress metrics are consistently better after a coffee chat with a certain colleague or an evening with close friends, you have objective evidence of that relationship's restorative value. It reinforces the importance of prioritizing those connections as a non-negotiable part of your health regimen. Hearing how others have leveraged community and technology in their wellness journey can be inspiring; the shared experiences in Oxyzen testimonials often highlight this social dimension of health.
We have traversed the landscape of stress physiology, from its damaging pathways to the multitude of buffers and interventions available. Now, we arrive at the most critical step: synthesis. Information overload is itself a stressor. The goal is not to implement every single strategy perfectly, but to create a personalized, sustainable plan that weaves key practices into the fabric of your life.
This plan is not static; it is a living system based on continuous feedback from your most trusted source: your own body.
Step 1: Establish Your Baseline with Data.
Before changing anything, observe. Use a biometric tracker for 1-2 weeks to establish your baseline. What is your average nightly HRV? Your resting heart rate? How much deep sleep do you typically get? This data is your starting point, free from guesswork.
Step 2: Implement ONE Keystone Habit.
Choose the one intervention you believe will have the greatest ripple effect. For most, this is either sleep hygiene or breathing breaks. Don't try to fix your diet, exercise, meditation, and digital habits all at once. Master one.
Step 3: Use Micro-Habits to Build Momentum.
Attach tiny, non-negotiable habits to existing routines (habit stacking).
Step 4: Schedule Your Resilience Practices.
If it's not scheduled, it's not real. Block time in your calendar for:
Step 5: Create Your Personal Feedback Loop.
This is where technology transforms effort into wisdom. Your plan is your hypothesis; your biometric data is the results report.
Embracing the Journey, Not the Perfection
Resilience is not about never feeling stressed. It is about recovering faster and with less systemic damage. Some days, your data will show poor recovery despite your best efforts. That's not failure; it's information. It tells you to be extra gentle with yourself that day.
Your personalized plan, guided by your unique data, turns the overwhelming challenge of "preventing stress-related illness" into a series of manageable, observable experiments in self-care. It empowers you to become the author of your own health story, making informed choices that protect your most valuable asset: your long-term physical well-being. To begin crafting a plan with the support of cutting-edge, personalized insights, learning more about the tools available at Oxyzen is an excellent first step on this proactive journey.
Your Trusted Sleep Advocate: Sleep Foundation — https://www.sleepfoundation.org
Discover a digital archive of scholarly articles: NIH — https://www.ncbi.nlm.nih.gov/
39 million citations for biomedical literature :PubMed — https://pubmed.ncbi.nlm.nih.gov/
Experts at Harvard Health Publishing covering a variety of health topics — https://www.health.harvard.edu/blog/
Every life deserves world class care :Cleveland Clinic - https://my.clevelandclinic.org/health
Wearable technology and the future of predictive health monitoring :MIT Technology Review — https://www.technologyreview.com/
Dedicated to the well-being of all people and guided by science :World Health Organization — https://www.who.int/news-room/
Psychological science and knowledge to benefit society and improve lives. :APA — https://www.apa.org/monitor/
Cutting-edge insights on human longevity and peak performance:
Lifespan Research — https://www.lifespan.io/
Global authority on exercise physiology, sports performance, and human recovery:
American College of Sports Medicine — https://www.acsm.org/
Neuroscience-driven guidance for better focus, sleep, and mental clarity:
Stanford Human Performance Lab — https://humanperformance.stanford.edu/
Evidence-based psychology and mind–body wellness resources:
Mayo Clinic — https://www.mayoclinic.org/healthy-lifestyle/
Data-backed research on emotional wellbeing, stress biology, and resilience:
American Institute of Stress — https://www.stress.org/