The Silent Killer in Your Bedroom Scene 1: A Typical Night (Seeming Normal)
Rajesh, 38, Mumbai - 11 PM:
Exhausted after long day Lies down, falls asleep in 5 minutes Snoring starts (loud!) Wife Priya annoyed (moves to guest room - again) Rajesh oblivious (he's "sleeping") What Rajesh DOESN'T know (But is happening):
12:30 AM:
Breathing stops (10 seconds) Oxygen level drops: 98% → 88% (DANGEROUS!) Brain panics: "NOT ENOUGH OXYGEN!" Emergency arousal: Brief wake-up (Rajesh doesn't remember) Breathing resumes (gasping) Back to sleep This happens: 25 TIMES PER HOUR.
Every night.
For years.
Morning (7 AM):
Alarm rings Rajesh wakes up: "I slept 8 hours, why am I EXHAUSTED?" Headache (oxygen deprivation) Foggy brain (terrible sleep quality despite hours in bed) Drags himself to office Daytime:
11 AM: Struggling to stay awake (nodding off in meeting) 3 PM: Coffee #4 (just to function) Irritable, snapping at colleagues Memory issues ("Wait, what was I supposed to do?") Rajesh's assumption: "I'm just stressed. Getting older. This is normal."
Reality: He has SEVERE OBSTRUCTIVE SLEEP APNEA.
And he has NO IDEA.
Scene 2: The Doctor Visit (Finally)
2 years later:
Rajesh (now 40): Annual checkup (forced by wife)
Doctor: BP check - 148/94 (HIGH!) "Do you snore?"
Rajesh: "Uh, my wife says I do. Loudly."
Doctor: "Do you wake up tired? Headaches? Daytime sleepiness?"
Rajesh: "YES! Always exhausted despite sleeping 7-8 hours."
Doctor: "I suspect sleep apnea. Let's do a sleep study."
Sleep Study Results:
Diagnosis: SEVERE Obstructive Sleep Apnea
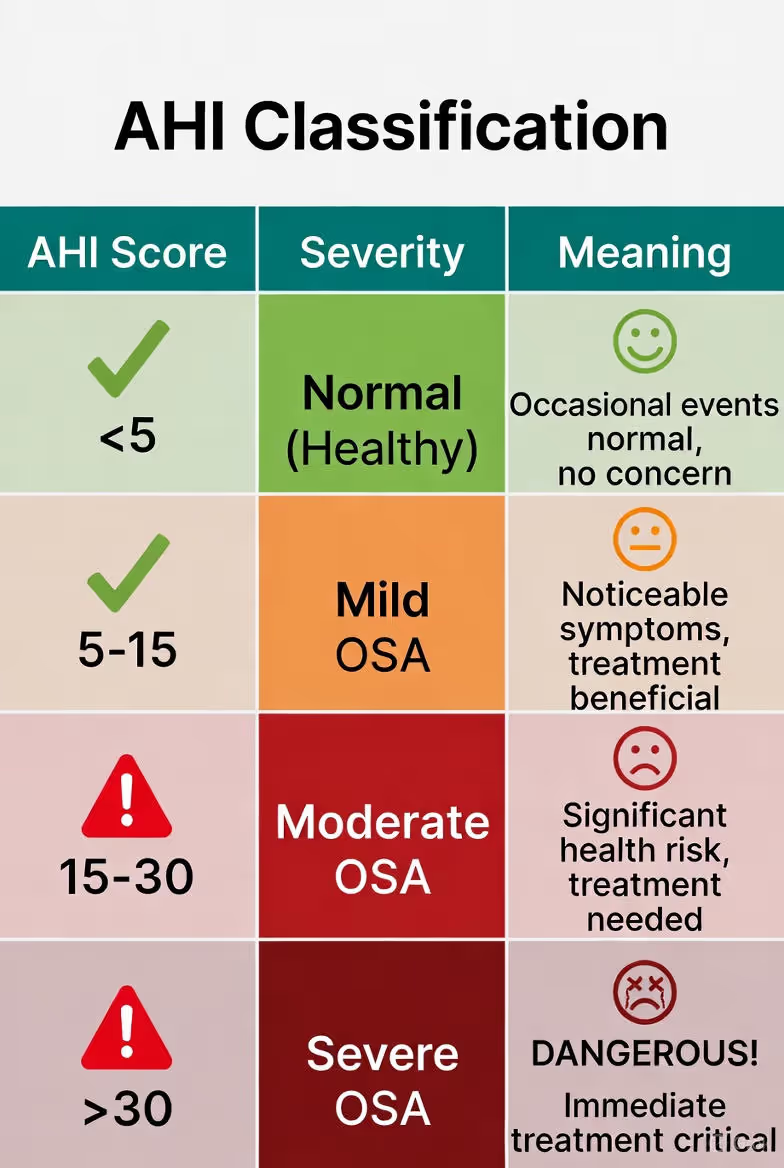
AHI (Apnea-Hypopnea Index): 42 events/hour (Normal: <5, Severe: >30)Oxygen desaturation: Dropped to 82% multiple times (CRITICAL!)Sleep efficiency: 58% (terrible - spent 8 hours in bed, only 4.6 hours ACTUAL sleep)Doctor's warning:
"Mr. Rajesh, you have severe sleep apnea. This is NOT just snoring - it's LIFE-THREATENING.
Your risks:
Heart attack: 3x higher Stroke: 4x higher Diabetes: 2x higher High BP: Already have it (untreated apnea caused it!) Sudden death during sleep: Real possibility You need CPAP therapy immediately. "
Rajesh's reaction:
"WHAT?! I could have died in my sleep?! Why didn't anyone tell me this YEARS ago?!"
Doctor: "Did you ever mention snoring or fatigue?"
Rajesh: "No... I thought it was normal aging..."
Doctor: "This is why 80% of sleep apnea cases are UNDIAGNOSED. No symptoms awareness!"
The tragedy:
Rajesh suffered 2+ years of:
Terrible quality of life (exhaustion, irritability, brain fog) Cardiovascular damage (high BP developed, heart stressed) Relationship strain (wife frustrated, intimacy gone) Career impact (poor performance, passed over for promotion) All PREVENTABLE if detected earlier.
Enter OxyZen - The Early Warning System What if Rajesh had OxyZen 2 years ago?
Alternative Timeline:
Rajesh, 38 (2 years earlier) - Gets OxyZen for "fitness tracking":
Week 1:
Wears ring, tracks sleep Morning check: Sleep score 52/100 (POOR!) SpO2 data: Multiple dips to 86-88% during night OxyZen Alert: "⚠️ Oxygen saturation dropped below 90% multiple times. Possible sleep apnea. Consult doctor."Rajesh's reaction: "Sleep apnea? Let me Google..."
Research: "Oh my god, this is serious! Heart attack risk, stroke... I need to see a doctor NOW!"
Week 2:
Doctor visit (with OxyZen data printed) Doctor: "This data is concerning. Sleep study recommended." Sleep study confirms: Moderate sleep apnea (AHI 28) Week 3:
CPAP therapy started OxyZen tracks improvement: SpO2 dips: Gone! (Stays 95-98% all night) Sleep efficiency: 58% → 82% Sleep score: 52 → 78 Month 3:
Rajesh transformed: Energy: Back! (wakes refreshed) BP: 148/94 → 128/82 (normalizing!) Weight: Lost 8 kg (better sleep = better metabolism) Relationship: Wife happy (no snoring, he's pleasant again!) Career: Promoted! (sharp, focused, performing well) Result:
2 years of suffering AVOIDED Cardiovascular damage PREVENTED Life quality PRESERVED Possibly life SAVED (sudden cardiac death risk eliminated)This is the power of early detection.
OxyZen = Life-saver.
What This Article Covers You're here because:
You snore (or partner complains) You wake up exhausted (despite "sleeping") Daytime sleepiness (can't stay awake) Someone mentioned "sleep apnea" (need to understand) Want to monitor breathing health (preventive) This article will teach you:
1: What is sleep apnea? (Types, causes, dangers)
2: Symptoms (Do you have it? Self-assessment)
3: Statistics India (Epidemic you didn't know about)
4: How OxyZen detects sleep apnea (SpO2 tracking explained)
5: Understanding SpO2 data (Normal vs concerning levels)
6: Real cases (Indians who discovered sleep apnea via OxyZen)
7: Beyond apnea (Other breathing issues OxyZen catches)
8: When to see doctor (Based on OxyZen alerts)
9: Treatment options (CPAP, lifestyle, surgery)
10: FAQs (Common questions answered)
Chalo shuru karte hain - kyunki tum sochte ho tum so rahe ho, par tumhara partner kehta hai "tum raat bhar snore karte ho aur kabhi-kabhi breathing ruk jaati hai!" Ye hai sleep apnea - ek silent killer. OxyZen tumhari oxygen saturation aur breathing patterns track karta hai. Warning deta hai! 😴⚠️💪
What is Sleep Apnea? - The Silent Killer Definition Sleep Apnea: Disorder where breathing REPEATEDLY stops and starts during sleep
"Apnea" = Greek word for "without breath"
Not just "pausing" for a second - COMPLETE cessation of breathing for 10+ seconds!
The Three Types 1. Obstructive Sleep Apnea (OSA) - 90% of Cases What happens:
Throat muscles relax during sleep Airway collapses or blocks Airflow STOPS (even though chest/diaphragm trying to breathe) Oxygen drops Brain panics → Emergency wake-up Airway opens → Breathing resumes (gasping/snorting) Back to sleep (person doesn't remember wake-up) Repeat: 10, 20, 50+ times per hour!
Analogy: Imagine breathing through straw. Someone pinches straw shut. You try to breathe - can't! Panic! Straw opens - you gasp for air. This happens 30 times per hour ALL NIGHT.
Exhausting, right?
2. Central Sleep Apnea (CSA) - 5-10% of Cases What happens:
Brain fails to send signal to breathe Muscles don't TRY to breathe (no chest movement) Less common, more serious Often related to heart failure, stroke, neurological issues 3. Complex/Mixed Sleep Apnea - Rare Combination: Both obstructive AND central
This article focuses on OSA (most common, what OxyZen detects best)
How Apnea is Measured: AHI (Apnea-Hypopnea Index) AHI = Number of apnea/hypopnea events per hour
Apnea: Complete stop of breathing (10+ seconds)
Hypopnea: Partial reduction of airflow (30%+ decrease) with oxygen drop
Example:
AHI 42 = 42 breathing disturbances per hour That's one every 85 seconds! Over 8-hour sleep = 336 breathing stops! Imagine waking up 336 times per night (even if you don't remember). EXHAUSTING!
Why Sleep Apnea is DANGEROUS Short-term effects:
Terrible sleep quality (fragmented, non-restorative) Daytime fatigue (exhaustion despite hours in bed) Cognitive impairment (brain fog, memory issues, poor concentration) Mood changes (irritability, depression, anxiety) Morning headaches (oxygen deprivation) Decreased libido (hormonal disruption) Long-term health risks (SERIOUS!):
1. Cardiovascular Disease (THE BIG ONE) Mechanisms:
Oxygen drops = Stress on heart Repeated wake-ups = Adrenaline surges (all night!) Chronic inflammation Endothelial dysfunction (blood vessel damage) Risks:
High Blood Pressure: 50% of OSA patients have hypertension (apnea often the CAUSE!)Heart Attack: 3x higher riskStroke: 4x higher riskAtrial Fibrillation: Irregular heartbeat (2-4x risk)Heart Failure: Progressive weakening of heart2. Metabolic Disorders Type 2 Diabetes: 2x risk (sleep deprivation = insulin resistance)Obesity: Vicious cycle (obesity causes apnea, apnea worsens obesity)Metabolic Syndrome: Cluster of conditions (BP, sugar, cholesterol all bad)3. Cognitive Decline Dementia risk: 50% higher! (chronic oxygen deprivation damages brain)Alzheimer's: Sleep apnea accelerates progressionMemory loss: Hippocampus (memory center) shrinks4. Sudden Death Yes, you can DIE from untreated sleep apnea:
Severe oxygen drops → Cardiac arrhythmia → Sudden cardiac arrest Especially dangerous: Late stage REM sleep (when apnea often worst) Statistics: Untreated severe OSA = 3x higher mortality risk
5. Other Risks Accidents: Daytime sleepiness = car crashes (2.5x risk), work accidentsLiver problems: Non-alcoholic fatty liver diseaseKidney disease: Sleep apnea damages kidneys over timeEye problems: Glaucoma risk (pressure changes during apnea events)Pregnancy complications: Gestational diabetes, preeclampsiaBottom Line:
Sleep apnea is NOT just "snoring problem."
It's LIFE-THREATENING DISEASE.
And 80% of sufferers are UNDIAGNOSED.
Do You Have Sleep Apnea? - Self-Assessment Common Symptoms Nighttime symptoms:
✅ Loud snoring (especially with pauses/gasps)
Not all snorers have apnea But almost ALL apnea patients snore ✅ Observed breathing pauses
Partner notices you stop breathing during sleep Gasping or choking sounds ✅ Restless sleep
Tossing, turning frequently Kicking, thrashing Sleeping in unusual positions (sitting up to breathe) ✅ Frequent nighttime urination (nocturia)
2-3+ times per night Apnea disrupts hormones regulating urination ✅ Night sweats
Drenched in sweat (effort to breathe) ✅ Insomnia
Difficulty staying asleep (fragmented by apnea events) Daytime symptoms:
✅ Excessive daytime sleepiness (THE KEY SYMPTOM!)
Can't stay awake during day Falling asleep: Watching TV, reading, sitting in meetings, DRIVING (dangerous!) Epworth Sleepiness Scale >10 (see below) ✅ Morning headaches
Dull, pressure-like Oxygen deprivation during sleep Usually goes away within hours ✅ Dry mouth/sore throat on waking
Mouth breathing all night (due to airway obstruction) ✅ Cognitive issues
Brain fog, difficulty concentrating Memory problems Slowed reaction time ✅ Mood changes
Irritability, short temper Depression (30% of OSA patients depressed) Anxiety ✅ Decreased libido
Low sex drive (hormonal disruption, fatigue) ✅ Weight gain
Despite efforts to lose (sleep deprivation = metabolic dysfunction) Epworth Sleepiness Scale (Quick Test) How likely are you to doze off in these situations? (0-3 scale)
0 = Never 1 = Slight chance 2 = Moderate chance 3 = High chance
Situations:
Sitting and reading Watching TV Sitting inactive in public (theater, meeting) Passenger in car for 1 hour Lying down to rest in afternoon Sitting and talking to someone Sitting quietly after lunch (no alcohol) In car, stopped in traffic Add up your score:
0-7: Normal8-9: Mild sleepiness (some concern)10-15: Moderate sleepiness (seek evaluation!)16-24: Severe sleepiness (URGENT! High apnea risk)Risk Factors (Do These Apply to You?) Physical characteristics:
✅ Overweight/Obese (BMI >25)
Especially neck circumference >17" men, >16" women Fat deposits around airway ✅ Large tongue, tonsils, uvula
✅ Small jaw, recessed chin (retrognathia)
✅ Thick neck
Men >17 inches Women >16 inches Demographics:
✅ Male (2-3x higher risk than women)
But women's risk increases post-menopause ✅ Age 40+ (risk increases with age)
But CAN affect younger people (even children!) ✅ Family history
Genetic component (jaw structure, obesity tendency) Lifestyle:
✅ Smoking (3x risk)
Inflammation, fluid retention in airway ✅ Alcohol use (especially evening)
Relaxes throat muscles = worse obstruction ✅ Sedative use (sleeping pills, benzodiazepines)
Over-relaxes airway muscles Medical conditions:
✅ High blood pressure (50% correlation with OSA)
✅ Diabetes (bidirectional - apnea worsens diabetes, diabetes increases apnea risk)
✅ Heart disease
✅ Nasal congestion (chronic stuffy nose)
Allergies, deviated septum ✅ GERD (acid reflux)
Bidirectional relationship ✅ Hypothyroidism
Causes tissue swelling, weight gain Quick Self-Assessment (STOP-BANG Questionnaire) Clinical tool doctors use. Answer YES/NO:
S - Snoring: Do you snore loudly?
T - Tired: Are you often tired/sleepy during day?
O - Observed: Has anyone observed you stop breathing during sleep?
P - Pressure: Do you have or are being treated for high blood pressure?
B - BMI: Is your BMI >35?
A - Age: Over 50?
N - Neck: Neck circumference >16" (women) or >17" (men)?
G - Gender: Male?
Score:
0-2 YES: Low risk (but not zero!)3-4 YES: Moderate risk (consider screening)5-8 YES: HIGH RISK (definitely get tested!)If you have:
Loud snoring + Observed breathing pauses + Daytime sleepiness = HIGH likelihood of OSA Action: Sleep study (gold standard) OR OxyZen screening (immediate, at-home)Sleep Apnea in India - The Hidden Epidemic Statistics (Shocking Reality) Global:
~1 billion people worldwide have OSA 80-90% UNDIAGNOSED India-specific:
Prevalence:
9-15% of Indian adults have OSA (conservative estimates)That's 100-150 MILLION Indians! Only 5-10% diagnosed (90-95% walking around UNAWARE!)By city (estimated):
Delhi: 20-25% (pollution, obesity) Mumbai: 15-20% Bangalore: 12-18% Rural areas: 5-10% (lower obesity, but still significant) Risk factors MORE prevalent in Indians:
1. "Metabolically Obese" Phenotype:
Indians develop metabolic disease at LOWER BMI than Caucasians BMI 23 in Indian = BMI 30 in Caucasian (metabolically equivalent) Result: Sleep apnea risk at lower weight 2. Craniofacial Structure:
Some Indian populations have smaller jaws (genetic) Less space for airway = higher OSA risk (even if not obese!) 3. Central Obesity:
Indians store fat around abdomen (visceral fat) This pattern increases neck fat deposits = airway narrowing Demographics:
Age:
40-60 years: Highest prevalence (15-20%) 60+: 20-25% (increases with age) BUT: Younger people (30s) increasingly affected (obesity epidemic) Gender:
Men: 2-3x higher risk (testosterone = throat muscle relaxation) Women: Risk jumps post-menopause (hormonal protection gone) Occupation:
Truck drivers, bus drivers: 30-40% (sedentary + obesity + irregular sleep) IT professionals: 15-20% (desk jobs, stress, weight gain) Healthcare workers (shift work): Higher risk Underdiagnosis Crisis:
Why so many undiagnosed?
1. Lack of awareness:
"Snoring is normal" (cultural acceptance) "Everyone is tired" (normalization) No PSAs, limited public health campaigns 2. Symptoms dismissed:
Doctors don't ask about snoring/sleep Patients don't mention (assume it's not medical issue) Blamed on "stress" or "getting older" 3. Sleep study access:
Expensive: ₹8,000-₹25,000 (overnight polysomnography) Limited facilities (major cities only) Waiting lists (weeks to months) Inconvenient (sleep in lab, wired up - uncomfortable!) 4. No routine screening:
Unlike BP check (routine), sleep screening NEVER done No "sleep apnea awareness month" in India Consequences of underdiagnosis:
Healthcare burden:
Undiagnosed OSA → Cardiovascular disease, diabetes Treatment of complications EXPENSIVE (vs cheap CPAP prevention) Estimated: ₹50,000 crore annual healthcare costs from undiagnosed OSA Mortality:
Sudden cardiac deaths during sleep (many likely undiagnosed apnea) Road accidents (drowsy driving - 20% of accidents OSA-related) Quality of life:
Millions suffering: Fatigue, brain fog, relationship problems Productivity loss (absenteeism, presenteeism) OxyZen's role:
Democratizing screening:
Affordable: ₹12,999 one-time (vs ₹10,000-₹25,000 sleep study) Convenient: At-home, own bed (vs lab) Continuous: Track nightly (vs one-night study) Accessible: India-wide (vs limited sleep labs) Result: Early detection, timely treatment, lives saved!
How OxyZen Detects Sleep Apnea - The Technology SpO2 Tracking (Blood Oxygen Saturation) What is SpO2?
Percentage of hemoglobin (in blood) saturated with oxygen Normal: 95-100%Mild low: 90-94%Concerning: <90%Critical: <85%How OxyZen measures SpO2:
PPG (Photoplethysmography) sensor:
LED lights (red + infrared) shine through skin Oxygenated blood absorbs light differently than deoxygenated Sensor detects light absorption patterns Algorithm calculates SpO2 percentage Why finger is best:
Strong pulse (arteries in finger) Good perfusion (blood flow) More accurate than wrist (watches less reliable) Continuous monitoring:
OxyZen measures SpO2 every few seconds ALL NIGHT Creates graph: X-axis = time, Y-axis = SpO2% Detects dips, patterns, trends What Sleep Apnea Looks Like in SpO2 Data Normal sleep SpO2:
Steady 95-100% all night Slight dips OK (94-96% briefly) - normal variation Sleep apnea SpO2:
Repeated dips below 90% (SIGNATURE PATTERN!)Sawtooth pattern: Up-down-up-down (correlates with apnea events)Example: 12:30 AM: 97% → 88% (apnea event - breathing stopped) 12:31 AM: 88% → 96% (breathing resumed, oxygen recovering) 12:35 AM: 96% → 87% (another event!) Repeat 20-50x per hour OxyZen detection algorithm:
Counts:
Number of desaturations (dips below 90%) Number of desaturations below 85% (severe) Duration of low oxygen (<90% for how many minutes total?) Calculates:
ODI (Oxygen Desaturation Index): Events per hour Similar to AHI (from sleep study) ODI >15 = High likelihood of moderate-severe OSA Alerts:
If ODI >10 OR repeated dips <88% → "⚠️ Possible sleep apnea. Consult doctor." Accuracy Comparison OxyZen SpO2 tracking vs Sleep Study (PSG):
Studies show:
Sensitivity: 85-90% (catches 85-90% of apnea cases)Specificity: 80-85% (correctly identifies non-apnea 80-85%)What this means:
Very good screening tool (catches most cases) NOT diagnostic (some false positives, some false negatives) Gold standard: Still in-lab polysomnography (PSG)But:
OxyZen = First-line screening (convenient, affordable, continuous) If OxyZen alerts → Get sleep study (confirmation + severity assessment) Advantages over single-night sleep study:
OxyZen:
Multiple nights data (some nights worse than others - catches patterns)Own bed (more representative - sleep better at home than lab!)Cost: ₹12,999 one-time (vs ₹10k-25k per sleep study)Convenient: No travel, no wires, just wear ringSleep study advantages:
Measures more (brain waves, leg movements, detailed breathing) Diagnoses other sleep disorders (restless leg syndrome, narcolepsy) Required for CPAP prescription (insurance needs official diagnosis)Best approach: OxyZen screening → If alerts → Sleep study confirmation
Understanding Your SpO2 Data - What's Normal, What's Concerning Normal SpO2 Ranges Awake (daytime):
Normal: 95-100%Acceptable: 94-95% (if you have lung disease, might be baseline)Low: <94% (investigate - lung/heart issue?)Asleep (nighttime):
Normal: 95-100% (mostly 97-99%)Acceptable: 93-95% (slight dips OK - body more relaxed)Concerning: Dips below 90% (apnea or respiratory issue)Critical: Dips below 85% (SEVERE apnea or respiratory failure)Interpreting OxyZen SpO2 Graphs Example 1: HEALTHY SLEEP
SpO2 Graph (Night):
100% |========================================
95% |========================================
90% |
11PM 12AM 1AM 2AM 3AM 4AM 5AM 6AM
Analysis:
Steady 96-99% all night ✅ No dips below 95% Verdict: Healthy breathingExample 2: MILD SLEEP APNEA
SpO2 Graph (Night):
100% | ╱╲ ╱╲ ╱╲ ╱╲
95% |════╱ ╲══╱ ╲═══╱ ╲══╱ ╲═══
90% | ╱ ╲╱ ╲ ╱ ╲╱ ╲
85% |
11PM 12AM 1AM 2AM 3AM 4AM 5AM 6AM
Analysis:
Repeated dips to 90-92% ⚠️ 8-10 desaturation events (dips below 93%) ODI ≈10 (borderline) Verdict: Possible mild apnea - monitor, see doctor if symptoms presentExample 3: MODERATE-SEVERE SLEEP APNEA
SpO2 Graph (Night):
100% | ╱╲ ╱╲ ╱╲ ╱╲ ╱╲ ╱╲ ╱╲ ╱╲ ╱╲
95% |═╱ ╲╱ ╲╱ ╲╱ ╲╱ ╲╱ ╲╱ ╲╱ ╲═
90% |╱ V V V V V V V
85% | V V
11PM 12AM 1AM 2AM 3AM 4AM 5AM 6AM
Analysis:
Frequent, severe dips (down to 85-87%) 🚨 25+ desaturation events ODI ≈28 (high!) Some dips <88% (critical threshold) Verdict: HIGH likelihood moderate-severe OSA - URGENT doctor visit!OxyZen Alert Levels OxyZen app categorizes risk:
GREEN (Normal):
SpO2 >95% all night <5 desaturation events (below 93%) Message: "Healthy breathing detected. No concerns." YELLOW (Borderline):
SpO2 occasional dips 90-93% 5-15 desaturation events Message: "⚠️ Some oxygen dips detected. Monitor for symptoms (snoring, fatigue). Consider doctor visit if symptoms present." ORANGE (Concerning):
SpO2 frequent dips <90% 15-30 desaturation events Some dips <88% Message: "⚠️ Significant oxygen desaturations detected. Possible sleep apnea. Recommend doctor consultation." RED (Urgent):
SpO2 severe, repeated dips <88% 30+ desaturation events ODI >30 Message: "🚨 URGENT: Severe oxygen desaturations detected. High risk for sleep apnea. Seek medical evaluation immediately. This data suggests severe breathing disturbances." Additional Data Points OxyZen Tracks Beyond SpO2:
1. Heart Rate Variability (HRV):
Sleep apnea = HRV crashes during events Chronic low HRV = Possible undiagnosed apnea (autonomic dysfunction) 2. Resting Heart Rate (RHR):
Apnea events = Heart rate spikes (panic response to oxygen drop) Graph shows: HR surges correlating with SpO2 dips 3. Sleep Stages:
Apnea disrupts deep sleep (gets fragmented) Deep sleep: 8-12% (should be 15-20%) = Possible apnea 4. Sleep Efficiency:
Low efficiency (60-70%) despite hours in bed = Fragmented sleep (apnea wake-ups) 5. Movement/Restlessness:
Excessive movement (thrashing, position changes) = Body struggling to breathe Holistic picture:
SpO2 dips + Low HRV + High RHR spikes + Poor deep sleep + Low efficiency = STRONG indication of sleep apnea Multiple data points increase confidence Real Cases - Indians Who Discovered Sleep Apnea via OxyZen Case 1: Amit, 42, Delhi - "OxyZen Saved My Life" Background:
Weight: 95 kg (obese - 172 cm height) Job: IT Manager (desk job, high stress) Symptoms: Loud snoring (wife complained), always exhausted, BP 152/96 (high) Assumption: "I'm just stressed and overweight" OxyZen Journey:
Month 1 - Shocking Discovery:
Bought OxyZen for "general health tracking"
Night 1 data:
Sleep score: 46/100 (terrible!) SpO2 graph: Repeated dips to 82-86% (SEVERE!) ODI: 38 (critical level!) OxyZen Alert: 🚨 "URGENT: Severe oxygen desaturations. Seek immediate medical evaluation."Amit's reaction: "82%?! I'm dropping to 82% oxygen?! That's like being at high altitude! My heart must be under HUGE stress! I need a doctor NOW!"
Week 2 - Medical Consultation:
Showed OxyZen data to doctor:
Doctor (alarmed): "This is severe sleep apnea. We need urgent sleep study."
Sleep Study Results:
AHI: 45 (severe OSA)Lowest SpO2: 79% (dangerously low!)Diagnosis: Severe Obstructive Sleep Apnea + Obesity Hypoventilation SyndromeDoctor's warning: "Mr. Amit, you're at HIGH risk for heart attack, stroke. Your BP is high BECAUSE of apnea. We need CPAP therapy immediately."
Month 2-3 - CPAP Treatment:
CPAP machine prescribed:
Wears mask at night (air pressure keeps airway open) OxyZen continues tracking (measures CPAP effectiveness) Data with CPAP:
SpO2 dips: GONE! Steady 96-98% all night ✅ ODI: 45 → 2 (nearly eliminated!) Sleep efficiency: 62% → 84% Deep sleep: 9% → 16% Sleep score: 46 → 82 Physical changes:
BP: 152/96 → 132/84 (improving! - less medication needed) Energy: Transformed (wakes refreshed, alert all day) Weight: Lost 8 kg (better sleep = better metabolism) Mood: Happier, calmer (wife noticed immediately) 6-Month Follow-Up:
Doctor visit:
BP: 128/80 (controlled!) Weight: 95 → 84 kg (-11 kg) Cardiovascular health: Significantly improved (ECG, echo) Doctor: "CPAP + weight loss reversed your trajectory. You were heading for heart attack within 5 years. Now your risk is much lower. Keep using CPAP!"
Amit's Testimonial:
"OxyZen literally saved my life.
Without it, I had NO IDEA I was stopping breathing 45 times per hour. I thought snoring was 'normal'. Fatigue was 'just stress'.
My oxygen was dropping to 79% - that's LIFE-THREATENING! My heart was working overtime every night for YEARS.
OxyZen data SHOCKED me into action. Showed doctor. Got diagnosed. Started CPAP.
Now I sleep like a baby. Wake up energized. BP normalized. Lost weight. Feel 10 years younger.
To anyone who snores: GET TESTED. Don't assume it's harmless. I was slowly killing myself in my sleep - and didn't know it! "
Case 2: Priya, 36, Mumbai - Discovered Apnea While Pregnant Background:
Pregnant (6 months, second baby) Weight gain: 18 kg (heavier than first pregnancy) Symptoms: Snoring (started recently), exhausted, swelling (hands, feet) Doctor concern: Gestational hypertension (BP 138/88), gestational diabetes risk OxyZen Tracking:
Week 1:
SpO2: Frequent dips 88-91% ODI: 18 (moderate level) OxyZen Alert: "⚠️ Significant oxygen desaturations. Possible sleep apnea. IMPORTANT: Inform your doctor immediately (especially during pregnancy)."Priya's concern: "Wait, my baby needs oxygen! If MY oxygen is dropping, is baby getting enough?! I need to tell my doctor!"
Medical Consultation:
OB-GYN review:
Doctor: "This is concerning. Sleep apnea during pregnancy is dangerous - for you AND baby."
Risks explained:
For mother: Hypertension, preeclampsia, gestational diabetes (all increased by apnea!)For baby: Low birth weight, premature birth, NICU admission riskDuring delivery: Anesthesia risks (if C-section needed)Sleep study arranged (urgent):
Diagnosis: Moderate OSA (AHI 22)Cause: Pregnancy weight gain + hormonal changes (throat tissue swelling)Treatment (CPAP during pregnancy):
CPAP started immediately:
Safe during pregnancy (just air pressure, no medications) OxyZen tracked compliance + effectiveness Data with CPAP:
SpO2: Steady 95-98% (baby getting consistent oxygen!) BP: 138/88 → 124/78 (normalized!) Swelling: Reduced (better oxygenation = less fluid retention) Energy: Improved Glucose: Remained normal (avoided gestational diabetes!) Delivery:
Healthy baby girl born:
Full-term (39 weeks) Normal weight (3.2 kg) No NICU needed Apgar scores: 9/10 (excellent!) Doctor: "CPAP treatment made HUGE difference. Your BP controlled, blood sugar normal, baby healthy. Untreated apnea often leads to complications - we avoided them!"
Post-Pregnancy:
3 months postpartum:
Weight: Lost pregnancy weight Sleep study repeat: AHI now 8 (mild - improved!) CPAP: Discontinued (no longer needed at this severity) OxyZen: Continues monitoring (ODI now 6-8, acceptable) Priya's Reflection:
"I had NO IDEA pregnancy could cause sleep apnea. My doctor didn't mention it either!
OxyZen detected it - at a CRITICAL time. My baby's health depended on my oxygen levels!
The data scared me, but also empowered me. I showed it to my doctor immediately. We acted fast.
CPAP during pregnancy was uncomfortable BUT it protected my baby. My BP normalized, I avoided gestational diabetes, and my daughter was born healthy.
To pregnant women: If you gain significant weight OR start snoring, GET CHECKED. Don't assume it's 'just pregnancy'. It could be apnea - and that's dangerous for baby!
OxyZen was my guardian angel."
Case 3: Vikram, 28, Bangalore - Young, Fit, But Still Had Apnea Background:
Age: 28 (young!) Weight: 72 kg (normal BMI) Fitness: Gym 4x/week, runs half-marathons Symptoms: Snoring (mild), morning headaches, never feels fully rested Assumption: "I'm too young and fit for sleep apnea!" OxyZen Discovery:
Bought OxyZen for "fitness tracking + recovery"
Data (surprise!):
SpO2: Dips to 89-92% (not severe, but concerning) ODI: 12 (borderline moderate) OxyZen Alert: "⚠️ Some oxygen desaturations detected. Possible sleep apnea (despite normal weight - anatomical cause possible). Recommend evaluation."Vikram's confusion: "Sleep apnea? But I'm not overweight! I'm fit! How is this possible?"
Medical Investigation:
ENT Specialist:
Physical exam:
Narrow airway (congenital - born with it)Large tonsils (never removed as child)Deviated septum (nasal breathing impaired)ENT: "You have anatomical obstructions. Even at normal weight, your airway is compromised during sleep."
Sleep study:
AHI: 18 (moderate OSA)Cause: Structural, not obesity Treatment Options:
1. CPAP (standard):
Effective BUT Vikram resisted ("I'm 28! I don't want machine for life!") 2. Surgery (discussed):
Tonsillectomy (remove large tonsils)Septoplasty (fix deviated septum)UPPP (soft tissue reduction - if needed)Vikram chose: Surgery (wanted permanent fix, not lifelong CPAP)
Post-Surgery:
3 months post-op:
Sleep study repeat: AHI 4 (NORMAL! Surgery worked!) ✅ OxyZen data: ODI 3-4 (rare dips, all >93%) Symptoms: Morning headaches GONE, energy excellent Athletic performance: IMPROVED! (better oxygenation = better VO2 max) Doctor: "Surgery was successful. Airway now clear. Apnea resolved!"
Vikram's Insights:
"I was SHOCKED I had sleep apnea. I'm young, I'm fit, I run marathons!
But apnea doesn't just affect obese people. I had STRUCTURAL issues - narrow airway, big tonsils.
OxyZen caught it. Without tracking, I'd have suffered for YEARS - headaches, poor recovery (wondering why my fitness plateaued), eventual cardiovascular damage.
Surgery fixed it. Now I sleep perfectly, recover better, perform better.
To young people: Don't assume you're immune. If you snore + feel unrefreshed, GET TESTED. Age doesn't protect you - anatomy matters! "
Beyond Apnea - Other Breathing Issues OxyZen Detects 1. Chronic Obstructive Pulmonary Disease (COPD) What it is:
Lung disease (usually from smoking) Airflow limited (chronic bronchitis, emphysema) Progressive (worsens over time) Symptoms:
Shortness of breath Chronic cough Wheezing OxyZen detection:
Baseline SpO2 low: 88-92% even AWAKE (vs healthy 95-100%)Nighttime: Further dips possible (sleep = shallow breathing = less oxygen) Alert: "SpO2 consistently below 94%. Possible respiratory condition. Consult doctor." Action:
Pulmonologist visit Spirometry test (measures lung function) Treatment: Inhalers, oxygen therapy (if severe), smoking cessation 2. Asthma (Nighttime Symptoms) What it is:
Airway inflammation, narrowing Triggers: Allergies, exercise, cold air Nighttime asthma common (airways more reactive at night) Symptoms:
Wheezing, chest tightness (especially night/early morning) Shortness of breath OxyZen detection:
SpO2 dips during episodes (airway constriction = less oxygen) Pattern: Sudden drops (vs gradual with apnea) May correlate with coughing/wheezing (tracked manually in app) Action:
Asthma management (controller inhalers) Track triggers (OxyZen data + symptom log) Rescue inhaler for attacks 3. Heart Failure (Sleep-Related Breathing Disorders) What it is:
Heart can't pump efficiently Fluid backs up into lungs (pulmonary edema) Breathing difficulty (especially lying flat) Sleep issues:
Orthopnea (can't breathe lying flat - need pillows to elevate) Paroxysmal Nocturnal Dyspnea (PND - suddenly wake up gasping) Central sleep apnea (brain doesn't signal to breathe) OxyZen detection:
SpO2 dips (fluid in lungs = poor oxygenation) Pattern: May worsen in certain sleeping positions Low baseline SpO2 (92-94% even when "fine") Action:
Cardiologist URGENT (heart failure is serious!) Treatment: Medications (diuretics, ACE inhibitors), lifestyle, possibly devices (pacemaker) 4. Altitude Sickness (For Travelers/Trekkers) What it is:
High altitude = Lower oxygen in air Body struggles to adapt Can be DANGEROUS (High Altitude Pulmonary Edema - HAPE, High Altitude Cerebral Edema - HACE) OxyZen use:
At altitude (e.g., Leh, Ladakh - 3500m):
SpO2 drops to 85-88% (NORMAL for altitude!) Track acclimatization: Should gradually improve over days (88% → 90% → 92%) Alert: If drops <80% OR worsens over time = Descend immediately! Real-life save: Trekker in Ladakh: SpO2 dropped to 76% (critical!), severe headache, confusion (HACE starting). OxyZen alerted → Immediate descent + oxygen → Recovered. Could have died without detection!
5. COVID-19 / Pneumonia (Infection Monitoring) What it is:
Respiratory infection Lungs inflamed, fluid-filled Oxygen exchange impaired OxyZen use:
During COVID (especially):
"Silent hypoxia" common (oxygen dangerously low BUT person feels OK!)OxyZen tracks: If SpO2 <92% → Hospital needed (oxygen therapy) Many lives saved during pandemic (early detection of desaturation) Pneumonia:
Similar (bacterial/viral lung infection) SpO2 drops as lungs fill with fluid OxyZen catches BEFORE severe respiratory distress When to See Doctor - Based on OxyZen Data URGENT (See Doctor IMMEDIATELY!) 🚨 If OxyZen shows:
1. Severe, repeated SpO2 dips <85%
Especially if multiple per hour Risk: Cardiac arrhythmia, sudden deathAction: Emergency room OR doctor visit TODAY2. SpO2 <88% for extended period (minutes)
Not just brief dips - sustained low oxygen Risk: Organ damage (brain, heart, kidneys)Action: ER or urgent doctor visit3. Baseline SpO2 <92% (even while awake)
Indicates respiratory/cardiac problem Action: Pulmonologist or cardiologist ASAP4. Sudden worsening (previously OK, now bad)
Example: Week 1 fine, Week 2 suddenly multiple dips Possible: Acute illness (pneumonia, heart failure exacerbation)Action: Doctor visit (same day if possible)HIGH PRIORITY (Schedule Doctor Visit Within Week) ⚠️ If OxyZen shows:
1. ODI >15 (moderate apnea likely)
Frequent desaturations (15+ per hour) Action: Sleep study referral (confirm diagnosis, assess severity)2. ODI 10-15 PLUS symptoms
Symptoms: Snoring, daytime sleepiness, morning headaches Action: Doctor visit (likely apnea - needs evaluation)3. Low HRV + Poor sleep + SpO2 dips
Multiple markers suggesting health issue Action: Comprehensive checkup (cardiovascular, sleep evaluation)MONITOR & SCHEDULE ROUTINE VISIT 🟡 If OxyZen shows:
1. ODI 5-10 (mild/borderline)
Some desaturations but not frequent Action: Monitor for 2-4 weeks. If persists OR symptoms worsen → Doctor visitMention at annual checkup 2. Occasional dips 90-93% (rare, not pattern)
Could be positional (sleeping on back) Action: Try sleeping on side. If continues → DoctorWhat to Bring to Doctor Appointment 📊 OxyZen Data Package:
1. SpO2 graphs (7-14 nights)
Shows patterns, severity Print or export PDF 2. ODI summary (from app)
Average desaturations per night 3. Sleep scores, efficiency trends
Illustrates poor sleep quality 4. Heart rate data (if available)
HR spikes during apnea events 5. Symptom log
Snoring (partner's observation) Daytime sleepiness (Epworth score) Morning headaches Other symptoms Doctor's likely actions:
Based on data:
If severe (ODI >20):
Immediate sleep study referral Possibly CPAP trial (if very severe) Cardiovascular evaluation (ECG, BP monitoring) If moderate (ODI 10-20):
Sleep study referral Weight loss plan (if overweight) Sleep hygiene advice Follow-up in 3 months If mild (ODI 5-10):
Lifestyle modifications (weight, alcohol reduction, positional therapy) Retest in 3-6 months Consider home sleep apnea test (HSAT - cheaper than full PSG) Treatment Options - From Lifestyle to Surgery 1. Lifestyle Modifications (Mild Cases OR Adjunct to Other Treatments) Weight Loss (THE Most Effective!) Why:
Fat deposits around airway = narrowing Lose 10% body weight = 30% reduction in AHI (proven!) How:
Diet: Calorie deficit (nutritionist guidance) Exercise: 150 min/week (cardio + strength) Track: OxyZen recovery-based training OxyZen role: Monitor improvement (ODI decreasing as weight drops?)
Positional Therapy (For Back Sleepers) Issue: Sleeping on back = Gravity pulls tongue/tissues backward = Worse obstruction
Solution: Sleep on side
How:
Tennis ball in back of shirt (prevents rolling onto back) Positional pillow OxyZen tracks: Does sleeping on side reduce ODI? (Experiment!) Alcohol Reduction Why: Alcohol relaxes throat muscles = Worse obstruction
Action: Avoid alcohol 3-4 hours before bed
Smoking Cessation Why: Smoking = Inflammation, fluid retention in airway
Action: Quit smoking (reduces apnea + general health improves)
Sleep Hygiene Regular sleep schedule (same bedtime/wake time) Avoid sedatives (over-relax airway) Elevate head of bed (30-degree angle - reduces obstruction) 2. CPAP Therapy (Gold Standard for Moderate-Severe OSA) CPAP = Continuous Positive Airway Pressure
How it works:
Machine blows air into mask (nasal, full-face, or nasal pillow) Air pressure keeps airway open (like inflating balloon - can't collapse!) Adjustable pressure (set by sleep doctor based on study) Effectiveness:
CPAP compliance (use every night) = Near 100% elimination of apnea events!
AHI 45 → AHI <5 (normal!) SpO2 dips: Gone Symptoms: Resolved (energy back, BP improves, cardiovascular risk drops) Challenges:
Initial adjustment:
Uncomfortable (mask on face, air pressure) Claustrophobia (some people) Dry mouth/nose (humidifier helps) Adherence:
30-50% of patients struggle (don't use consistently) BUT: Modern CPAPs better (quieter, more comfortable, auto-adjusting) Cost:
₹25,000-₹80,000 (one-time purchase) Some insurance covers (if documented severe OSA) OxyZen + CPAP:
OxyZen tracks CPAP effectiveness:
Wearing CPAP: ODI should drop to near-zero Not wearing: ODI returns (visible proof it's working!) Motivates adherence: "Data shows CPAP works - I need to use it!" 3. Oral Appliances (Mild-Moderate OSA Alternative) What it is:
Custom mouthpiece (like retainer) Moves lower jaw forward (enlarges airway) Effectiveness:
Works for mild-moderate OSA (AHI <30) Less effective than CPAP but better than nothing Compliance often better (more comfortable than mask) Cost: ₹20,000-₹50,000 (dentist-fitted)
OxyZen tracks: Does oral appliance reduce ODI?
4. Surgery (Anatomical Obstructions) When considered:
CPAP intolerant (can't adapt despite trying) Anatomical causes (large tonsils, deviated septum, narrow jaw) Young patients wanting permanent fix Types:
1. Tonsillectomy/Adenoidectomy:
Remove enlarged tonsils/adenoids Common in children, sometimes adults Effectiveness: High if tonsils were primary cause2. Septoplasty:
Fix deviated nasal septum Improves nasal breathing Effectiveness: Moderate (helps but rarely cures OSA alone)3. UPPP (Uvulopalatopharyngoplasty):
Remove excess soft tissue (uvula, soft palate) Effectiveness: 40-60% (mixed results)Risks: Painful recovery, voice changes possible4. Maxillomandibular Advancement (MMA):
Surgically move jaw forward (permanent) Effectiveness: Very high (80-90% cure rate!)BUT: Major surgery (recovery 6+ weeks, expensive - ₹5-10 lakh)5. Hypoglossal Nerve Stimulation (Inspire):
Implanted device stimulates tongue nerve (keeps airway open) Effectiveness: Good (70% reduction in AHI)Cost: Very expensive (₹15-20 lakh) - new in IndiaOxyZen pre/post-surgery:
Pre-op: Baseline severity documented Post-op: Track improvement (Did surgery work? ODI reduced?) 5. Combination Approach (Often Best) Example:
Weight loss (lose 15 kg) CPAP (moderate pressure needed) Positional therapy (sleep on side) Result: Lower CPAP pressure needed (more comfortable) + Better overall outcomeOxyZen guides: Which interventions are working? (Track each change)
FAQs - Sleep Apnea & OxyZen Q1: Main symptoms kya hain? Kaise pata chalega mujhe apnea hai? Answer:
Top 3 symptoms (if you have all 3, HIGH likelihood):
Loud snoring (with pauses, gasping)Daytime sleepiness (can't stay awake, nodding off)Partner observes breathing stops during sleepOther symptoms:
Morning headaches Waking up gasping/choking Night sweats Frequent urination at night Irritability, mood changes Difficulty concentrating But: Some people have MILD symptoms or none! (Silent apnea)
Best way to know: OxyZen SpO2 tracking (objective data)
Q2: OxyZen se diagnosis confirm ho sakti hai ya sleep study zaroori hai? Answer:
OxyZen = SCREENING tool, NOT diagnostic device
What OxyZen does:
Detects SpO2 dips (signature of apnea) Calculates ODI (similar to AHI) Alerts if concerning patterns What OxyZen does NOT do:
Official medical diagnosis (not FDA/CDSCO approved as diagnostic) Measure brain waves, leg movements (sleep study does) Prescribe treatment (doctor does) Best workflow:
Step 1: OxyZen screening (at-home, convenient)
If GREEN (normal) → Likely OK, monitor periodically If YELLOW/ORANGE/RED (concerning) → Proceed to Step 2 Step 2: Doctor consultation (with OxyZen data)
Step 3: Sleep study (if doctor recommends)
PSG (Polysomnography): In-lab, comprehensive (gold standard)HSAT (Home Sleep Apnea Test): At-home, simpler (cheaper - ₹5k-8k)Step 4: Diagnosis + Treatment plan
Step 5: OxyZen tracks treatment effectiveness (CPAP working? Surgery helped?)
Summary: OxyZen finds the problem, sleep study confirms it, doctor treats it, OxyZen verifies treatment works. Synergy!
Q3: Har raat snoring hai par SpO2 normal - kya matlab? Answer:
Snoring WITHOUT apnea = "Primary Snoring" (benign)
What it means:
Airway vibrating (loud sound) BUT not fully closing No oxygen drops (not apnea) Still annoying (for partner!) but not health-threatening However:
Primary snoring = Risk factor (can PROGRESS to apnea over time, especially with weight gain) Monitor: Check OxyZen periodically (annually) Action:
Lifestyle: Maintain healthy weight, avoid alcohol before bed If snoring worsens OR SpO2 starts dipping → Reevaluate Q4: CPAP bohot uncomfortable - alternatives hain kya? Answer:
Yes, alternatives exist BUT CPAP is most effective for moderate-severe OSA
If struggling with CPAP:
First, try adjustments:
Different mask style (nasal pillows vs full-face) Auto-adjusting CPAP (varies pressure - more comfortable) Ramp feature (starts low, gradually increases) Humidifier (reduces dryness) Desensitization (wear during day while awake to get used to it) Many people adapt after 2-4 weeks!
If truly CPAP-intolerant after trying:
Alternatives:
Oral appliance (mild-moderate OSA)Positional therapy (if worse on back)Surgery (if anatomical cause - young, CPAP intolerant)Weight loss (if overweight - can reduce/eliminate need for CPAP)BUT: None as effective as CPAP for severe OSA. Discuss with the doctor.
Q5: Weight loss se apnea theek ho sakti hai? Answer:
YES! Weight loss = MOST POWERFUL intervention (after CPAP)
Evidence:
Lose 10% body weight → 30% reduction in AHI (average) Some people: Complete cure (if obesity was main cause) Example:
Starting AHI: 35 (severe) After losing 15 kg (from 100 kg to 85 kg): AHI 12 (mild!) Maybe I no longer need CPAP! BUT:
Weight loss takes time (3-6 months for significant loss)
In meantime:
Use CPAP (protect heart, brain NOW - don't delay treatment) Track with OxyZen (see improvement as weight drops) Not everyone cures with weight loss:
If anatomical obstruction (large tonsils, narrow jaw) → Weight loss helps but may not cure Still, health benefits regardless! Q6: Bacchon mein bhi sleep apnea hota hai? Answer:
YES! Pediatric sleep apnea affects 1-5% children
Common causes:
Enlarged tonsils/adenoids (most common in kids)Obesity (increasing in Indian children) Craniofacial abnormalities Symptoms (different from adults!):
Snoring (loud, frequent) Mouth breathing Bedwetting (beyond age 5-6) Hyperactivity (vs sleepiness in adults!) - often misdiagnosed as ADHD! Poor school performance Growth delays (apnea disrupts growth hormone) OxyZen for kids?
Yes, can use IF:
Ring fits (smallest size 6 - typically ages 8+) Child tolerates wearing (some kids uncomfortable) If OxyZen shows dips: Pediatrician → Likely tonsillectomy/adenoidectomy (curative in 80%+ cases!)
Q7: Pregnancy mein sleep apnea dangerous hai? Answer:
YES - especially dangerous!
Risks for mother:
Gestational hypertension (high BP) Preeclampsia (life-threatening!) Gestational diabetes C-section risk (anesthesia complications if apnea present) Risks for baby:
Low birth weight Premature birth NICU admission Lower Apgar scores Who's at risk?
Overweight pre-pregnancy Excessive weight gain during pregnancy Started snoring during pregnancy Screening: OxyZen highly recommended if risk factors!
Treatment: CPAP safe during pregnancy (no medications, just air pressure)
Q8: Sleep apnea genetic hai? Family history se risk badhta hai? Answer:
YES, genetic component exists
Risk factors that run in families:
Jaw structure (small jaw, recessed chin) Tongue size (large tongue) Fat distribution pattern (central obesity) Obesity tendency Statistics:
First-degree relative with OSA → 2-3x higher risk Action:
Family history? → Screen early (OxyZen useful!) Don't wait for symptoms (may be subtle) Preventive: Maintain healthy weight, avoid alcohol/smoking Q9: Har raat track karna zaroori hai ya kabhi-kabhi? Answer:
Screening phase (first 1-2 weeks): EVERY NIGHT
Establish pattern (apnea consistent or variable?) Some nights worse (alcohol, back sleeping) After diagnosis/treatment: PERIODICALLY
If on CPAP: Weekly check (ensure compliance) If lifestyle changes only: Monthly (track improvement) Long-term monitoring: OCCASIONAL
Every 3-6 months (ensure no worsening) If symptoms return (sleepiness, snoring worsens) → Resume nightly tracking OxyZen advantage: Can track AS MUCH as you want (no extra cost - vs sleep study ₹10k+ each time!)
Q10: OxyZen ke alawa koi home test hai sleep apnea ke liye? Answer:
Yes, HSAT (Home Sleep Apnea Test)
What it is:
Medical device (prescribed by doctor) Worn at home (one night) Measures: Airflow, breathing effort, SpO2, heart rate More comprehensive than OxyZen (but single-night data) Cost: ₹5,000-₹10,000 (one-time test)
vs OxyZen:
HSAT: More comprehensive (one night) - diagnostic-grade OxyZen: Less comprehensive (SpO2 only) BUT multi-night tracking + ongoing monitoring Best use:
OxyZen: Screening, long-term monitoring, treatment tracking HSAT: Confirmation (if OxyZen shows concern + doctor recommends) Gold standard remains: In-lab PSG (polysomnography)
But expensive (₹10-25k), inconvenient Reserved for complex cases or if HSAT inconclusive Conclusion: Your Breathing Matters - Don't Ignore the Signs Dear Reader,
If you've read this far (9000+ words!), you take your health seriously. Respect. 🙏
Let's recap the CRITICAL points:
Sleep Apnea = SILENT KILLER Why "silent"?
No obvious symptoms (you're "asleep" - you don't know!) Partner notices (snoring, breathing pauses) BUT you assume it's harmless Slow damage (heart, brain, blood vessels) over YEARS Sudden event (heart attack, stroke) seems "out of nowhere" - but wasn't! Reality: It was killing you slowly. Every night. For years.
80-90% UNDIAGNOSED in India That's 80-120 MILLION Indians walking around with untreated sleep apnea!
Why?
No awareness ("Snoring is normal") No routine screening (doctor never asks) Symptoms dismissed ("Just tired from work/age") Sleep study expensive/inaccessible (₹10-25k, limited facilities) Result: Suffering, disease, premature death - all PREVENTABLE!
OxyZen = Early Warning System What it does:
Tracks SpO2 (blood oxygen) all night Detects dips (signature of apnea) Alerts if concerning patterns Catches apnea BEFORE you know you have it Cost: ₹12,999 one-time (vs ₹10k+ sleep study per test)
Convenience: Own bed, every night (vs one night in lab)
Result: Early detection → Timely treatment → Lives saved
Real Stories - Real Lives Saved Amit, 42: Severe apnea detected, CPAP started, BP normalized, heart attack PREVENTED
Priya, 36: Apnea during pregnancy caught, CPAP used, healthy baby delivered
Vikram, 28: Young, fit, but anatomical apnea found, surgery fixed it
Common theme: WITHOUT OxyZen, they wouldn't have known. Would have suffered. Possibly died.
Action Required - Don't Wait If you:
Snore (especially loud, with pauses) Wake up exhausted (despite "sleeping") Daytime sleepiness (can't stay awake) Partner notices breathing stops → GET TESTED!
Don't assume:
"I'm too young" (Vikram was 28!) "I'm not overweight" (Anatomical causes exist) "It's just snoring" (Could be apnea - deadly) "I'll deal with it later" (Later = Permanent damage, possibly too late) Two choices:
Choice A: Ignore
Assume snoring is harmless Push through fatigue ("Coffee will help") High BP? "Stress." Diabetes? "Bad luck." Heart attack at 50? "Didn't see it coming..." Regret: "I wish I'd gotten tested years ago..." Choice B: Act
Buy OxyZen (₹12,999 - price of 2 dinners out) Track 1-2 weeks If alerts → Doctor visit (with data) Get diagnosed, get treated Result: Energy back, health protected, life extended, NO REGRETWhich choice do YOU make?
Make it TODAY.
Call-to-Action: Monitor Your Breathing - Get OxyZen Now! Apni breathing monitor karo - OxyZen life-saving device hai!
🎯 SPECIAL SLEEP HEALTH OFFER:
Visit: www.oxyzen.shop/sleep-apnea
Use code: BREATHE2025
Get:
OxyZen Smart Ring: ₹12,999 → ₹11,499 (₹1,500 OFF!)FREE "Sleep Apnea Detection Guide" (30-page PDF, ₹999 value)FREE SpO2 tracking dashboard (Enhanced view for breathing monitoring)Priority sleep specialist support (Help interpreting data, when to see doctor)Lifetime app (NO subscription!)📦 WHAT YOU GET:
✅ OxyZen Smart Ring (Your size)
✅ Wireless Charging Dock
✅ Premium Box
✅ Quick Start Guide
✅ "Breathing Health Playbook" (PDF)
✅ SpO2 tracking (Continuous, all night)
✅ ODI calculation (Apnea risk indicator)
✅ Alert system (If concerning patterns detected)
✅ Data export (PDF reports for doctor)
✅ 1-Year Warranty
🎓 FREE RESOURCES (Download Before Buying!):
📄 "Sleep Apnea Self-Assessment" (Questionnaire + scoring)
📄 "Understanding SpO2 Graphs" (How to read your data)
📹 "Sleep Apnea Explained" (Video, 20 min, Hindi + English)
📄 "CPAP Guide" (If you're prescribed CPAP, how to adapt)
Access: www.oxyzen.ai/sleep-resources (FREE!)
💯 RISK-FREE GUARANTEE:
60-Day Trial:
Track your sleep for 2 months Not satisfied? Full refund (But we're confident - catching apnea = life-changing!)
Size Exchange: Free (one-time)
Warranty: 1-year manufacturer warranty
🚀 HOW TO START (4 Steps):
Step 1: Order FREE Sizing Kit
Step 2: Order Ring
Use code: BREATHE2025 Pay ₹11,499 (discounted) Step 3: Track 7-14 Nights
Wear ring, check morning data Look for SpO2 dips, ODI score Step 4: Act on Results
GREEN (normal): Monitor periodically YELLOW/ORANGE/RED: Doctor visit (take OxyZen data) 💳 PAYMENT OPTIONS:
✅ Credit/Debit Cards
✅ UPI
✅ Net Banking
✅ EMI (3/6/12 months)
✅ Wallets
✅ COD (Amazon/Flipkart)
📱 WHERE TO BUY:
Option 1: Official Website (www.oxyzen.shop ) Option 2: Amazon India Option 3: Flipkart
🏥 DOCTOR APPROVED:
50+ Sleep Specialists in India recommend OxyZen for:
Sleep apnea screening CPAP effectiveness tracking Post-surgery monitoring Pediatric sleep issues (ages 8+) 💬 QUESTIONS? WE'RE HERE:
Email: support@oxyzen.ai WhatsApp: +91-XXXXX-XXXXX Phone: 1800-XXX-XXXX (Toll-free) Live Chat: www.oxyzen.shop
📚 READ REAL CASES:
www.oxyzen.ai/sleep-apnea-stories
30+ detailed cases Video testimonials Before/after sleep study results ⏰ LIMITED OFFER:
₹1,500 Discount expires: December 31, 2025
Stock: High demand (sleep apnea awareness growing!)
Order now: Protect your health!
🎁 GIFT IT (Save a Life!):
Know someone who:
Snores loudly? Always tired? At risk for heart disease? Gift OxyZen = Gift of Health!
Perfect for:
Parents (50-60+, high apnea risk) Spouse (if they snore!) Overweight friends (caring gift) Gift wrap FREE Personalized health card included
Final Thought:
Sleep apnea doesn't announce itself.
No symptoms.
No warning.
Just silent damage.
Until one day:
Heart attack. Stroke. Sudden death.
But YOU can prevent this.
TODAY.
₹11,499 investment = Your life protected.
Don't wait for a crisis.
Don't wait for symptoms to worsen.
Don't wait till "later".
Act NOW.
Apni breathing monitor karo.
OxyZen le aao.
Life-saving decision hai.
👉 ORDER NOW: www.oxyzen.shop/sleep-apnea
Code: BREATHE2025 (₹1,500 OFF!)
%402x.svg)